- (2009) Volume 10, Issue 1
Pandanaboyana Sanjay, Sim Yeeting, Carole Whigham, Hannah K Judson, Christoph Kulli, Francesco M Polignano, Iain S Tait
Department of Hepatobiliary and Pancreatic Surgery, Ninewells Hospital and Medical School. Dundee, Scotland, United Kingdom
Received September 13th, 2008 - Accepted November 19th, 2008
Context Current management of gallstone pancreatitis in a university hospital. Objective Comparison of current management of gallstone pancreatitis with recommendations in national guidelines. Setting Tertiary care centre in Scotland. Subjects One-hundred consecutive patients admitted with gallstone pancreatitis. Methods All patients that presented with gallstone pancreatitis over a 4- year period were audited retrospectively. Data were collated for radiological diagnosis within 48 hours, ERCP within 72 hours, CT at 6-10 days, and use of high-dependency or intensive therapy units in severe gallstone pancreatitis, and definitive treatment of gallstone pancreatitis within 2 weeks as recommended in national guidelines. Results Forty-six patients had severe gallstone pancreatitis and 54 patients mild pancreatitis. Etiology was established within 48 hours in 92 patients. Six (13.0%) out of the patients with severe gallstone pancreatitis were managed in a high dependency unit. Fifteen (32.6%) patients with severe gallstone pancreatitis underwent CT within 6-10 days of admission. Four (8.7%) of the 46 patients with severe gallstone pancreatitis had urgent ERCP (less than 72 hours). Overall 22/100 patients unsuitable for surgery underwent endoscopic sphincterotomy as definitive treatment. Seventy-eight patients had surgery, with 40 (51.3%) of these patients undergoing an index admission cholecystectomy, and 38 (48.7%) patients were discharged for interval cholecystectomy. Overall 81 patients with gallstone pancreatitis had definitive therapy during the index to same admission (cholecystectomy or sphincterotomy). Two (5.3%) patients were readmitted whilst awaiting interval cholecystectomy: one with acute cholecystitis and one with acute pancreatitis. There were no mortalities in this cohort. Conclusion This study has highlighted difficulties in implementation of national guidelines, as the use of critical care, timing of ERCP and CT, and definitive treatment prior to discharge did not concur with national targets for gallstone pancreatitis.
Cholecystectomy; Clinical Audit; Gallstones; Pancreatitis; Guidelines as Topic
APACHE: Acute Physiology and Chronic Health Evaluation; BSG: British Society of Gastroenterology; HDU: high dependency unit; ICU: intensive care unit
Gallstones are the most common (30-50%) preventable cause of pancreatitis in the United Kingdom [1]. Recurrent attacks of gallstone pancreatitis carry a mortality rate of 10% and a major morbidity rate of 30- 40% [2]. Whilst it has been suggested that the course and outcome of acute pancreatitis is not influenced by the aetiological factor, patients with gallstone pancreatitis represent a clinical cohort that benefit from specific endoscopic and surgical interventions with the risk of recurrent pancreatitis reduced in these patients following removal of gallstones [2]. In this context appropriate management of gallstone pancreatitis assumes significance. In 2005, revised guidelines for management of acute pancreatitis were published by the working party of British Society of Gastroenterology (BSG), the Association of Surgeons of Great Britain and Ireland, the Pancreatic Society and the Association of Upper Gastrointestinal Surgeons [3]. Specific guidance was suggested for management of gallstone pancreatitis. Previous prospectively audited studies [4] against earlier BSG guidelines (1998) [5] have suggested that management targets are not being met. The aim of this study was to determine the current management of gallstone pancreatitis in a university teaching hospital and compare this practice with that proposed in published national guidelines.
An audit of all consecutive patients that presented with gallstone pancreatitis over a 4-year period (2002-2005) to a university hospital was performed. This hospital was also a tertiary referral centre for management of patients with severe pancreatitis. The patients were identified from Lothian Surgical Audit Database. Gallstone pancreatitis was defined when the following criteria were met: clinical history consistent with pancreatitis, elevated serum amylase level more than 3- fold the upper reference limit (greater than 300 U/L; reference range: 0-100 U/L), and radiological or ERCP evidence of gallstones. Obstructive jaundice was defined as elevated serum bilirubin (reference range: 0- 15 μmol/L and/or elevated alkaline phosphatase (reference range: 50-90 U/L)
Data were collected from case notes review and hospital laboratory database onto a standard proforma. The data collected included demographics of the patients, time to diagnosis, Glasgow severity scores, serum C-reactive protein (CRP) levels, severity stratification within 48 hours, time to ERCP, CT scan within 6-10 days of presentation in severe cases and utilisation of high dependency unit (HDU) and intensive care unit (ICU) facilities. APACHE II (Acute Physiology and Chronic Health Evaluation) scores were calculated retrospectively for all patients from case notes and hospital laboratory database. Patients were stratified into mild and severe groups; severe pancreatitis was defined as the presence of CRP level at 48 hours greater than 150 mmol/L, and Glasgow severity score greater than 3 both at admission and within 48 hours, and APACHE II score equal to, or greater than, 8 within first 24 hours of admission. In addition data regarding whether or not definitive treatment (cholecystectomy or endoscopic sphincterotomy) was performed within the same hospital admission (index) or at a later date (interval) was determined.
In patients who did not undergo index cholecystectomy, the number of readmissions with recurrent pancreatitis or gallbladder related problems was obtained. The data obtained was compared against the published guidance to assess compliance with the guidelines. The specific guidelines which were compared included diagnosis and severity stratification with 48 hours of admission, CT scan with 6-10 days of admission, definitive management of gallstone pancreatitis on the same admission, use of HDU and ICU facility and overall mortality.
Descriptive statistics were computed: frequencies, median, and range.
One-hundred patients were admitted with gallstone pancreatitis during the study period. The median age of the study group was 68 years (range: 20-90 years). The male to female ratio was 1:3. Pancreatitis was established secondary to gallstones within 48 hours of presentation in 92 patients. The diagnosis was made on the basis of clinical presentation, hyperamylasaemia (85 patients) and ultrasound evidence of gallstones (all patients). In 82 patients severity stratification was performed within 48 hours according to the guidelines and in the remaining 18 patients severity stratification was done after 48 hours. The median amylase and median CRP levels (at 48 hours) were 1,155 U/L (range: 24-5,760 U/L) and 126 mmol/L (range: 3-432 mmol/L), respectively. Forty-nine patients had biochemical evidence of obstructive jaundice. The median APACHE II score was 7 (range: 0-22).
Forty-six patients were stratified as severe pancreatitis, based on raised CRP, GSS, and APACHE II score, and 54 patients as mild pancreatitis. The median APACHE II score in patients with severe pancreatitis was 9 (range: 8-22), while the median APACHE II score in patients with mild pancreatitis was 4 (range: 0-7). Fifteen (32.6%) patients with severe gallstone pancreatitis underwent CT within 6-10 days of admission. Forty-nine patients had biochemical evidence of obstructive jaundice; 21 (42.9%) had mild pancreatitis and 28 patients had severe pancreatitis (57.1%). Four out of these 49 patients (8.2%) underwent ERCP within 72 hours. Nine (18.4%) patients with obstructive jaundice had multiple stones on ultrasound.
Twenty-two patients were considered unfit for surgery because of medical comorbidities (American Society of Anesthesiologists; ASA grade 3 and 4) and therefore underwent endoscopic sphincterotomy as a definitive treatment. All 22 patients were assessed by consultant anaesthetist and were considered high risk for surgery. Of the remaining 78 patients, 40 patients (51.3%) underwent index cholecystectomy in the same admission as per the BSG guidelines.
Thirty-eight patients did not undergo an index cholecystectomy and were discharged home and then readmitted for an interval cholecystectomy. Nineteen (50.0%) of these patients had severe pancreatitis. Therefore, of the 46 patients with severe pancreatitis, 16 (34.8%) were considered unfit for surgery and underwent endoscopic sphincterotomy as definitive treatment with no further follow up, 11 (23.9%) patients had cholecystectomy in the same admission, and 19 patients (41.3%) were discharged and readmitted for interval cholecystectomy. Thirty-five (76.1%) patients with severe gallstone pancreatitis were considered unfit for surgery at the initial admission (16 endoscopic sphincterotomies and 19 discharges for readmission).
The median time from the diagnosis of acute pancreatitis to surgery was 7.5 days (range: 2-30 days) in the same-admission cholecystectomy group; and 63 days (range: 13-210 days) in the interval cholecystectomy group. The median total hospital stay was 10 days (range: 4-65 days) for patients in the same-admission cholecystectomy group and 12 days (range: 4-32 days) for patients with interval cholecystectomy.
Overall, 81 patients underwent definitive therapy during the initial admission (41 endoscopic sphincterotomies and 40 cholecystectomies). Of the 41 patients who underwent endoscopic sphincterotomies, 22 were unfit for surgery whilst 19 patients were discharged and readmitted for a cholecystectomy at a later date. By definition according to the guidelines, endoscopic sphincterotomy constitutes as definitive treatment, therefore, although 19 patients did come back for a cholecystectomy at a later date, they were still considered as having definitive treatment during the initial admission.
Six (13.0%) patients with severe gallstone pancreatitis were managed on a surgical HDU or ICU. Two patients (5.3%) who were discharged for an interval cholecystectomy were readmitted whilst awaiting surgery, one with acute cholecystitis and one with acute pancreatitis. There were no mortalities in this cohort. There were no deaths recorded during the study period. The comparison of the results from this audit with the national guidelines are summarised in Table 1.
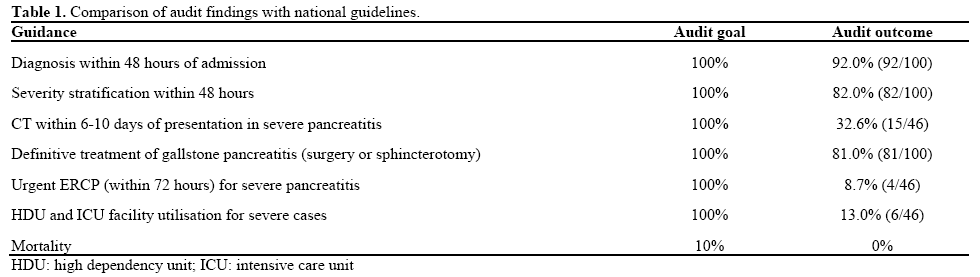
This audit has highlighted difficulties in meeting the targets proposed in national guidelines, as the use of critical care, timing of ERCP and CT, and definitive treatment prior to discharge did not concur with published guidelines for management of gallstone pancreatitis. However, delayed definitive treatment did not result in significant unplanned readmissions or morbidity related to cholelithiasis.
Although acute cholecystitis is the most common presentation of gallstones, gallstone pancreatitis represents the most severe form of the disease with mortality rates ranging from 2 to 17% [6, 7]. The incidence of pancreatitis has increased substantially across the world in the last two decades [7, 8, 9, 10] and in some countries has risen by more than 30% [7, 10]. In this context it becomes important to appropriately manage patients presenting with gallstone pancreatitis. Several recent audits have suggested the management of acute pancreatitis is suboptimal [11, 12, 13]. Interestingly few audits have assessed the impact of guidelines on management of “gallstone pancreatitis” specifically. Sargen et al. [4] in a prospective audit of gallstone pancreatitis found that targets were not achieved in definitive treatment of gallstone pancreatitis prior to discharge resulting in readmission with biliary-pancreatic disease. Toh et al. [11] reported that only one-third of patients with mild gallstone pancreatitis undergo definitive treatment within 4 weeks, and two further audits in UK hospitals revealed index cholecystectomy rates of 6.6% [4] and 20-22% [12]. Barnard et al. [14] compared all published audits to the BSG guidelines and noted that approximately 49% of the patients underwent definitive treatment of gallstones prior to discharge, although more recent audits have suggested increased compliance with BSG guidelines [15]. Whilst the specific reasons to why published studies failed to meet the BSG guidelines are not clear; limitations in access to operating theatre time and problems related to cancellation of elective surgery are implicated.
In gallstone pancreatitis the principal concern with a delayed (interval) cholecystectomy is that this predisposes the patients to further of episodes pancreatitis and biliary disease. In this study, 81% of patients with gallstone pancreatitis had definitive therapy during the same admission. However, the majority of the patients with severe gallstone pancreatitis (35/46, 76.1%) were unsuitable for a surgical intervention during the index admission. These patients were preferentially discharged home and readmitted within 6 months for an interval cholecystectomy. Though this practice does not comply with the BSG guidelines, there is a reasonable a case for delayed cholecystectomy in patients with severe pancreatitis. These patients often have peri-pancreatic fluid collections [16, 17] and an early cholecystectomy increases the risk of a subsequent second procedure to manage persistent fluid collections that do not resolve spontaneously [16]. A delayed cholecystectomy (more than 6 weeks) in this group facilitates simultaneous management of the pseudocyst, and an overall reduced hospitalization compared to early cholecystectomy. Furthermore, literature search identified a single randomised controlled trial comparing early and delayed cholecystectomy for gallstone pancreatitis [18]: index cholecystectomy was associated with a mortality of 47% whereas interval cholecystectomy was associated with a mortality of 11% in patients with severe gallstone pancreatitis.
In this study the outcome measure that scored worst against the BSG recommendations was provision of ERCP within 72 hours of admission. Similar observations were noted in other recent audits [15]. Mofidi et al. in a recent study noted that 48% of patients with severe pancreatitis underwent ERCP within 72 hours of admission [15]. Although this may depend on local service provision, other identifiable causes include difficulty in provision of out of hours ERCP [11, 19, 20] limiting urgent ERCP only to patients with cholangitis [15] and dilated common bile duct [21]. There is substantial evidence to suggest that urgent ERCP has a beneficial effect in reducing mortality in patients with gallstone pancreatitis and obstructive jaundice or cholangitis [22, 23]. Eight percent of all our patents with biliopancreatic obstruction underwent urgent ERCP. In the context of current evidence, these results are unjustified and clearly there is need to improve service provision to comply with the BSG guidance.
The mortality in severe acute pancreatitis is reported to be around 10-20% [24] and about 20% of patients with severe AP require management in an ICU to control organ failure [25] and reduce the mortality of these patients to less than 20% [26]. Previous audits have suggested that care within an ICU and HDU setting for severe cases does not meet the BSG targets [11, 15]. Several reasons are suggested for non-compliance including lack of resources and wrong stratification of disease severity. Utilisation of ICU and HDU facilities in this study was suboptimal. The main reason for this is inadequate numbers of ICU and HDU beds to accommodate all those that merit care within a critical care facility. Admission to ICU has been shown to improve long term functional outcome in survivors with severe pancreatitis [27]. Although it incurs increased hospital costs, great majority of patients survive to have good long term quality of life [27].
The results from the present audit suggest some aspects of care in the management of gallstone pancreatitis are suboptimal, especially with regards to the use of critical care facilities, timing of ERCP and CT, and definitive treatment during the index admission. Clinical resources to provide appropriate services (HDU/ERCP), early referral to upper gastro-intestinal specialists and education of all emergency surgeons is essential if we are to achieve the management targets suggested within current national guidelines.
Presented as a poster at the Association of Upper Gastrointestinal Surgeons, Annual Meeting, Cardiff, 2007. Published as abstract: British Journal of Surgery 2007; 95 (S5):46.
The authors have no potential conflicts of interest