Keywords
Conjunctival lithiasis; Superior limbic keratoconjunctivitis
Introduction
Superior limbic keratoconjunctivitis (SLK) is an inflammatory disease localized in the cornea and conjunctiva near the upper eyelid palpebral conjunctiva and superior limbus [1]. SLK is characterized by Inflammation of the superior palpebral and bulbar conjunctiva, fine punctate staining of the cornea adjacent to the superior corneal limbus, proliferation of superior limbic epithelial cells and filaments of the upper cornea and limbus [2]. SLK patients present with a variety of nonspecific symptoms, most of which occur in bilaterally but may appear asymmetric or occur in unilaterally. The most common symptoms are irritability, foreign body sensation, redness, photosensitivity, mucinous secretions, and inflammatory ptosis [2]. These symptoms are more severe in patients with filamentary keratitis. The discomfort is not severe in the morning, but it gradually becomes worse with time [3].
There are various theories about the mechanism of SLK, but nothing has been clarified yet. Currently, mechanical stimulation is the most important cause. Abnormal interactions between the upper and lower eyelid conjunctiva during eye blinking cause abnormal movement of the upper eye conjunctiva. This movement can occur especially when the superior palpebral conjunctiva is closely attached to the eye such as thyroid eye disease, proptosis, dry eye syndrome, wound and inflammation of upper palpebral conjunctiva [4]. In addition, studies have shown that substances such as TGF-β2, Tenascin, and Integrin β1, which are expressed by mechanical stimuli, are increased in patients with prominent conjunctivitis, further supporting the theory that SLK occurs by mechanical stimulation [5].
Conjunctival lithiasis consists of white blood cells or epithelial cells modified with white or yellow deposits on the conjunctiva of the lid, and amorphous materials consisting of mucopolysaccharides and mucus [6]. Conjunctival lithiasis is generally asymptomatic, but if it protrudes from the surface of the conjunctiva, it may also affect the conjunctiva and cornea, accompanied by inflammation of the eyelid [7]. We report a case of SLK caused by conjunctival lithiasis of the upper palpebral conjunctiva.
Case Summary
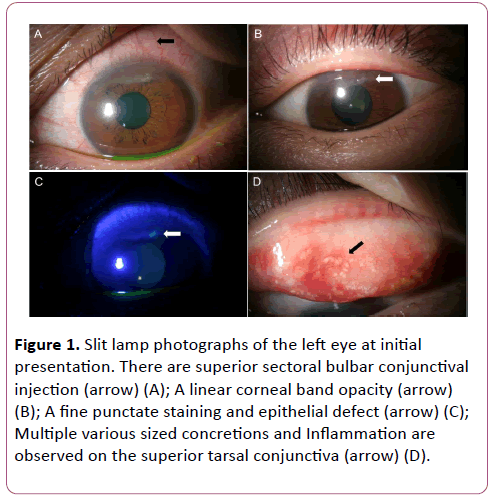
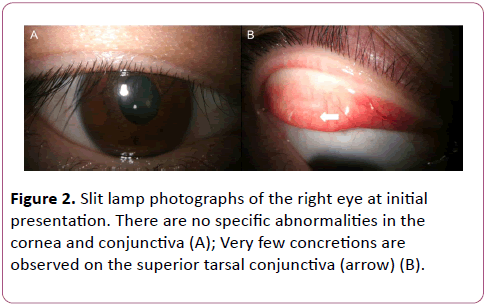
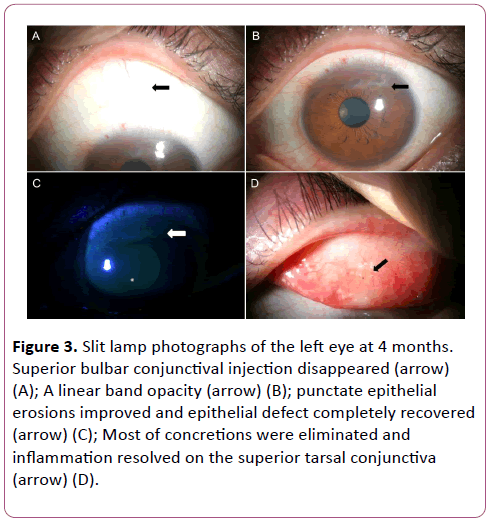
A 40-year-old man without any history of medical disease presented with a persistent left-sided foreign body sensation, pain, and conjunctival congestion that occurred a month ago. The best corrected visual acuity was 20/20 in the both eyes. The intraocular pressure measured by the noncontact tonometer was 16 mmHg in the right eye and 19 mmHg in the left eye. There were no findings such as protrusion of the eyeball and lid lag in the external eye examination. In the slit lamp examination, localized conjunctival injection and redundancy in the superior bulbar conjunctiva, superior corneal epithelial defect, and band shaped corneal opacity were observed in the left eye (Figures 1A-1C). No corneal dystrophy was observed to cause corneal epithelium to be vulnerable to stimulation. No inflammatory cells were found in the anterior chamber and no abnormalities were observed in the lens. Fundus examination and ultrasonography were also normal. When performing the upper eyelid eversion, conjunctival stones of various sizes were observed. (Figure 1D). Some of the conjunctival lithiasis were exposed exposed through the conjunctival epithelium.There was a small number of conjunctival lithiasis found in the upper eyelid in the right eye, but there was no specific finding in the cornea and conjunctiva (Figure 2). The patient had never been diagnosed with conjunctival lithiasis or had previously removed conjunctival lithiasis. We diagnosed SLK due to conjunctival stones and planned to remove conjunctival lithiasis. After topical anesthesia was performed with 0.5% proparacaine hydrochloride (Alcaine®, Alcon, Fort Worth, TX, USA), 2% lidocaine topical anesthesia mixed with 1: 100,000 epinephrine was injected into the upper eyelid conjunctiva and stones were removed using a 30 gauge needle. After the procedure, a bandage contact lens was applied. 0.3% gatifloxacin (Gatiflo®, Taejoon, Seoul, Korea), 0.5% loteprednol etabonate (Lotemax, Bausch & Lomb, Tampa, FL, USA) and 0.3% sodium hyaluronate) were used as eye drops. After 7 days of treatment, subjective symptoms, conjunctival injection, corneal epithelial defect and corneal opacity improved. During the follow-up period of 4 months, the conjunctival injection, superior corneal epithelial defect and corneal erosion disappeared and only a few haziness remained in the superior cornea (Figures 3A-3C). When perfoming the upper eyelid eversion, only a small amount of conjunctival stone was observed and no specific inflammation was observed (Figure 3D). The patient had no recurrence of conjunctivitis and no specific complications.
Figure 1: Slit lamp photographs of the left eye at initial presentation. There are superior sectoral bulbar conjunctival injection (arrow) (A); A linear corneal band opacity (arrow) (B); A fine punctate staining and epithelial defect (arrow) (C); Multiple various sized concretions and Inflammation are observed on the superior tarsal conjunctiva (arrow) (D).
Figure 2: Slit lamp photographs of the right eye at initial presentation. There are no specific abnormalities in the cornea and conjunctiva (A); Very few concretions are observed on the superior tarsal conjunctiva (arrow) (B).
Figure 3: Slit lamp photographs of the left eye at 4 months. Superior bulbar conjunctival injection disappeared (arrow) (A); A linear band opacity (arrow) (B); punctate epithelial erosions improved and epithelial defect completely recovered (arrow) (C); Most of concretions were eliminated and inflammation resolved on the superior tarsal conjunctiva (arrow) (D).
Discussion
SLK is a chronic recurrent inflammatory disease of the superior palpebral and bulbar conjunctiva near the superior limbus, which was first described by Theodore in 1963 as Superior Limbic keratoconjunctivitis (SLK) [8]. Characteristically, there is inflammation of the superior palpebral and bulbar conjunctiva, fine punctate staining around the superior limbus, proliferation of the epithelial cells, and findings of the filament. In addition, there is a decrease in corneal sensitivity and decreased tear secretion.
Symptoms of SLK include injection, foreign body sensation, photophobia, but decreased vision is rare because SLK is confined to the superior part of the cornea. It can occur in all age groups, but it occurs more in women in their 50s.2 Diseases associated with SLK include thyroid eye disease, proptosis, and dry eye syndrome and is known to occur frequently in patients with chronic inflammation of superior palpebral conjunctiva [9-11].
Until now, a clear mechanism for the development of conjunctivitis is unknown, but immunological abnormalities, lack of tears or major tear components, and mechanical stimuli are suggested [4,8,9]. The most important cause is the abnormal mechanical stimulation between the upper palpebral conjunctiva and the upper bulbar conjunctiva. Cher et al. [4] reported that mechanical irritation occurs due to microtrauma of the soft tissues caused by the repetitive movement between two pairs of tissues, ie, the upper palpebral and bulbar conjunctiva, and the conjunctiva and sclera. Physiologically, the mechanical stimulation on the superior limbus is caused by the contraction of the orbicularis muscle when closing the eyes, thereby compressing conjunctiva adjacent to the sclera. This causes the bulbar conjunctiva to slide from a larger diameter sclera to a smaller diameter cornea. When the bulbar conjunctiva sagging past the superior limbus, the connection between the conjunctiva and the sclera is broken by 2-3 mm, and the microfracture occurs, which disrupts the palisade of Vogt of the limbus. It is also reported that factors other than physiological factors change the contact resistance between the palpebral and bulbar conjunctiva. Sheu et al. [12] reported that lack of tears, decreased quality of the eyes, abnormal immune responses could alter the configuration of the conjunctival cells and increase the interconjunctival resistance. In addition, when there is a scar in superior palpebral conjunctiva, mechanical stimulation may also be caused by scar [13]. These repetitive mechanical stimuli cause chronic inflammation that causes SLK, which causes the vicious cycle and continues to cause symptoms.
Several methods are known for the treatment of SLK, and treatment methods based on the etiology of the disease are most effective. Non-surgical treatment methods include artificial tears, topical steroids, cromolyn sodium eye drops, mast cell stabilizers, autologous serum eye drops, and bandage contact lenses. Surgical treatment includes ocular conjunctival resection, silver nitrate application, and punctum occlusion [2,4,12]. In addition, various therapies have been proposed based on the theory that it is caused by mechanical stimulation, such as the injection of borylnithoxine in the orbicularis muscle and the bandage contact lens of large diameter [14,15].
Conjunctival lithiasis consists of amorphous material composed of mucopolysaccharide and mucus, which is a white or yellow dot-shaped lesion in palpebral conjunctiva [6]. It is known to be caused by aging of palpebral conjunctiva, repeated recurrence of chronic keratoconjunctivitis, and inflammation by trachoma [16,17]. In addition, dry eye syndrome and meibomian gland dysfunction are also reported to be potentially related [18,19]. Conjunctival lithiasis is generally asymptomatic, but symptoms may occur in 7% of all patients. If conjunctival lithiasis protrudes to the surface of the conjunctiva, it may cause a foreign body sensation or discomfort, and inflammation may occur if it bursts into the lamina propria of conjunctiva. Therefore, if symptoms appear and a discomfort is felt, it can be removed with a small gauge needle [20].
In this case, a number of conjunctival lithiasis present in superior palpebral conjunctiva increased mechanical friction on superior bulbar conjunctiva, resulting in increased friction, which caused the bulbar conjunctiva to be pushed to the cornea when the eyes closed and force is considered to have been repeatedly applied. Therefore, removal of conjunctival stones, which is the cause of mechanical stimulation, improved the symptoms of cornea and conjunctiva, and did not recur during the follow-up period. In the present case, the patient could not be diagnosed with SLK, which is a chronic and recurrent feature, because the patient complained of symptoms of SLK for the first time and subsequently removed the causative conjunctival stones. However, if the removal of conjunctival stones was not performed, it would have been a chronic recurrence due to sustained stimulation.
To our knowledge, reports of SLKs caused by local causes of eyelids are rare. In 2007 Sheu et al. [12] reported a case of congenital conjunctivitis developed after upper eyelid surgery. However, there has been no report of SLK due to conjunctival lithiasis. We report a case of conjunctival lithiasis with conjunctival lithiasis in which conjunctival lithiasis of superior palpebral conjunctiva was removed and treated without recurrence with artificial tear, antibiotic eye drops, steroid eye drops, and bandage contact lens. SLK does not always occur in all patients with conjunctival lithiasis, and the patient's symptom improvement may be a coincidence. However, mechanical irritation of the conjunctiva is considered to be the most important cause of SLK and the patient's symptoms improved after conjunctival lithiasis removal. Therefore, through the clinical process, the cause of SLK in this case is presumably due to conjunctival lithiasis.
With the exception of mild early stage SLK, treatment with dry eye syndrome and steroid therapy alone has limited therapeutic efficacy. Therefore, treatment for the cause of SLK must be performed together. In addition to the conjunctival lithiasis presented in this case, trachoma, giant papilla of conjunctivitis in spring, and upper eyelid papilla due to contact lens can also show SLK pattern and can be diagnosed as SLK on chronic progression [2,4,17]. Therefore, when treating patients with SLK, careful monitoring of superior palpebral conjunctiva is important and only cornea and conjunctiva treatment should not be performed without superior palpebral conjunctiva evaluation.
References
- Kim HB, Kweon E, Lee JB (1981) Superior limbic keratoconjunctivits. J Korean Ophthalmol Soc 22: 395-398.
- Nelson JD (1989) Superior limbic keratoconjunctivitis (SLK). Eye (Lond) 3(Pt 2): 180-189.
- Bainbridge JW, Mackie IA, Mackie I (1998) Diagnosis of Theodore’s superior limbic keratoconjunctivitis. Eye (Lond) 12(Pt 4): 748-749.
- Cher I (2000) Superior limbic keratoconjunctivitis: multifactorial mechanical pathogenesis. Clin Experiment Ophthalmol 28: 181-184.
- Matsuda A, Tagawa Y, Matsuda H (1999) TGF-beta2, tenascin, and integrin beta1 expression in superior limbic keratoconjunctivitis. Jpn J Ophthalmol 43: 251-256.
- Chin GN, Chi EY, Bunt AH (1980) Ultrastructural and histochemical studies of conjunctival concretions. Arch Ophthalmol 98: 720-724.
- Duke-Elder S (1965) System of Ophthalmology. St Louis: CY Mosby 585-586.
- Theodore FH, Ferry AP (1970) Superior limbic keratoconjunctivitis. Clinical and pathological correlations. Arch Ophthalmol 84: 481-484.
- Kadrmas EF, Bartley GB (1995) Superior limbic keratoconjunctivitis. A prognostic sign for severe Graves ophthalmopathy. Ophthalmology 102: 1472-1475.
- Wilson FM 2nd, Ostler HB (1986) Superior limbic keratoconjunctivitis. Int Ophthalmol Clin 26: 99-112.
- Wright P (1972) Superior limbic keratoconjunctivitis. Trans Ophthalmol Soc U K 92: 555-560.
- Sheu MC, Schoenfield L, Jeng BH (2007) Development of superior limbic keratoconjunctivitis after upper eyelid blepharoplasty surgery: support for the mechanical theory of its pathogenesis. Cornea 26: 490-492.
- Raber IM (1996) Superior limbic keratoconjunctivitis in association with scarring of the superior tarsal conjunctiva. Cornea 15: 312-316.
- Mackie IA (1995) Management of superior limbic keratoconjunctivitis with botulinum toxin. Eye 9: 143-144.
- Chun YS, Kim JC (2009) Treatment of superior limbic keratoconjunctivitis with a large-diameter contact lens and Botulium Toxin A. Cornea 28: 752-758.
- Chang SW, Hou PK, Chen MS (1990) Conjunctival concretions. Polarized microscopic, histopathologic, and ultrastructural studies. Arch Ophthalmol 108: 405-407.
- Wilson RP (1936) The pathology of trachoma. Bull Ophthalmol Soc Egypt 29: 1-5.
- Haicl P, Janková H, Jirsová K (2006) Dry eye syndrome in patients with conjunctival concretions. Cesk Slov Oftalmol 62: 415-422.
- Haicl P, Janková H (2005) Prevalance of conjunctival concretions. Cesk Slov Oftalmol 61: 260-264.
- Kulshrestha MK, Thaller VT (1995) Prevalence of conjunctival concretions. Eye (Lond) 9: 797-798.