Case Report - (2016) Volume 17, Issue 3
Tomoko Norose1, Nobuyuki Ohike1, Reika Suzuki1, Hideki Shibata1, Hideyuki Imai1, Tomohide Isobe1, Akira Shiokawa1, Yuichi Takano2, Eiichi Yamamura2, Naotaka Maruoka2, Masatsugu Nagahama2, Nobuyuki Takeyama3, Hiroki Mizukami4, Jun-ichi Tanaka4
Departments of 1Pathology, Division of Gastroenterology, 2Internal Medicine, 3Radiology and 4Gastroenterological and General Surgery, Showa University Fujigaoka Hospital, Yokohama, Kanagawa, Japan
*Corresponding Author:
Nobuyuki Ohike
Department of Pathology
Showa University Fujigaoka Hospital
1-30 Fujigaoka, Aoba-ku
Yokohama 227-8501, Kanagawa, Japan
Phone: +81-45-971-1151
Fax: +81-45-972-6242
E-mail: ohike@med.showa-u.ac.jp
Received January 24th, 2016 - Accepted March 11th, 2016
Context Intraductal papillary mucinous neoplasms of the pancreas can be associated with ordinary ductal adenocarcinomas as well as pancreatic intraepithelial neoplasias in the background pancreas; however, preoperative identification of peripheral pancreatic intraepithelial neoplasias is extremely difficult. Case report The patient was a 79-year-old male with a chief complaint of right hypochondria pain. Several imaging tests revealed a multilocular cystic lesion (6 cm in size) in the pancreatic head with communication to a mildly dilated main pancreatic duct (5 mm in diameter). Dual-echo T1-weighted imaging (T1WI) revealed subtle, focal signals suggesting fat in the upper pancreatic head. The carcinoembryonic antigen level in the pancreatic juice was elevated (1350 ng/mL), however, no malignant cells were detected by cytological examinations. Blood tumor markers were within normal ranges. Under a diagnosis of branch duct type or mixed-type IPMN, pancreaticoduodenectomy was performed. The multilocular cystic lesion was localized to the uncinate process of the pancreas, included excess mucous production, and was histologically diagnosed as non-invasive, branch duct type, intestinal-type IPMN. Conversely, apart from IPMN, small foci of high-grade PanIN corresponding to carcinoma in situ (less than 5 mm in diameter) of the peripheral pancreatic ducts were incidentally noticed within the fatty tissue, which was visualized by dual-echo T1WI. High-grade PanIN/ CIS involved periductal fibrosis and demonstrated the pancreatobiliary phenotype. Genetically, different KRAS mutants were detected in IPMN (G12R) and high-grade PanIN/CIS (G12V), respectively, and a GNAS mutation was detected in IPMN, but not in high-grade PanIN/ CIS. Conclusion A resected case of peripheral high-grade PanIN/CIS concomitant with branch duct type IPMN of the pancreas head was reported. Although this may simply be an incidental association and it is extremely difficult to preoperatively identify microscopic lesions of the peripheral ducts, secondary findings such as focal fatty change may shed light on the detection of such lesions.
Keywords
Carcinoma in Situ; GNAS protein, human; Pancreas
Abbreviations
CEA carcinoembryonic antigen; CIS carcinoma in situ; IPMNs intraductal papillary mucinous neoplasms; PanINs pancreatic intraepithelial neoplasias
INTRODUCTION
Intraductal papillary mucinous neoplasms (IPMNs) of the pancreas can progress to invasive carcinoma. In addition, IPMNs are complicated by ordinary pancreatic ductal carcinoma (PDC) with a frequency of 4-9% as a distinct lesion [1- 5]. Therefore, patients with IPMNs are recognized as a high-risk group for PDCs. Moreover, detailed microscopic observations of resected specimens due to IPMN often reveal scattered small IPMNs or pancreatic intraepithelial neoplasias (PanINs) in the background pancreas.
Both IPMNs and PanINs are pre-invasive lesions of PDCs and share histological similarities, however, they are different entities [6- 9]: IPMNs are characterized by macro-sized cystic dilatation (over 1 cm) of neoplastic ducts, which consist of tall columnar mucinous epithelium with papillary proliferation and excess mucous production. Conversely, PanINs are micro-sized atypical ducts of less than 5 mm, which consist of cuboidal to columnar epithelial cells showing flat to low-papillary proliferation and slight or poor mucous production. Recently, different genetic abnormalities between the two entities have also been clarified [10- 12].
We herein experienced a case of surgically resected pancreatic IPMN accompanied by high-grade PanIN/ carcinoma in situ (CIS) of the peripheral pancreatic duct in the background pancreas. In this report, two issues were discussed. The first issue was whether the two lesions could be clearly distinguished morphologically and genetically, and the second was whether it was possible to detect peripheral high-grade PanIN/CIS in preoperative imaging tests.
CLINICAL FEATURES OF CASE REPORT
The patient was a 79-year-old male with a chief complaint of right hypochondria pain. He had a smoking history of 20-30 cigarettes/day × 35 years. At the time of hospitalization, his height was 165.5 cm; weight: 53 kg (body mass index: 19.4); body temperature: 36.5°C; pulse: 64/min (adjusted); and blood pressure: 122/74 mmHg. There were no signs of anemia in the palpebral conjunctiva, however, yellowing of the bulbar conjunctiva was observed. The abdomen was flat and soft with normal bowel sounds. A mild elevation of the hepatobiliary enzymes was detected on blood biochemistry examinations. Several imaging tests, including computed tomography (CT), magnetic resonance imaging (MRI), magnetic resonance cholangiopancreatography (MRCP), endoscopic ultrasonography (EUS), and endoscopic retrograde cholangiopancreatography (ERCP), revealed a multilocular cystic lesion (6 cm in size on CT and MRCP) with communication to a mildly dilated main pancreatic duct (5.5 mm in diameter on EUS) in the pancreatic head (Figures 1, 2). Heterogeneous density within the loculi was observed on EUS, however, there were no obvious mural nodules. Dual-echo T1-weighted imaging (T1WI) revealed subtle focal signals suggesting fat in the upper pancreatic head (over the multilocular cystic lesion) (Figure 2). Mucous discharge from the papilla of Vater was noted during EUS. Although the CEA level in the pancreatic juice was elevated (1350 ng/mL), no malignant cells were identified by a cytological exam. Blood tumor markers (CEA, CA19-9, and DUPAN-2) were within normal ranges. Under a diagnosis of either branch duct type or mixed-type IPMN, subtotal stomach-preserving pancreaticoduodenectomy was performed. The patient’s course has remained uneventful without recurrence for seventeen months.
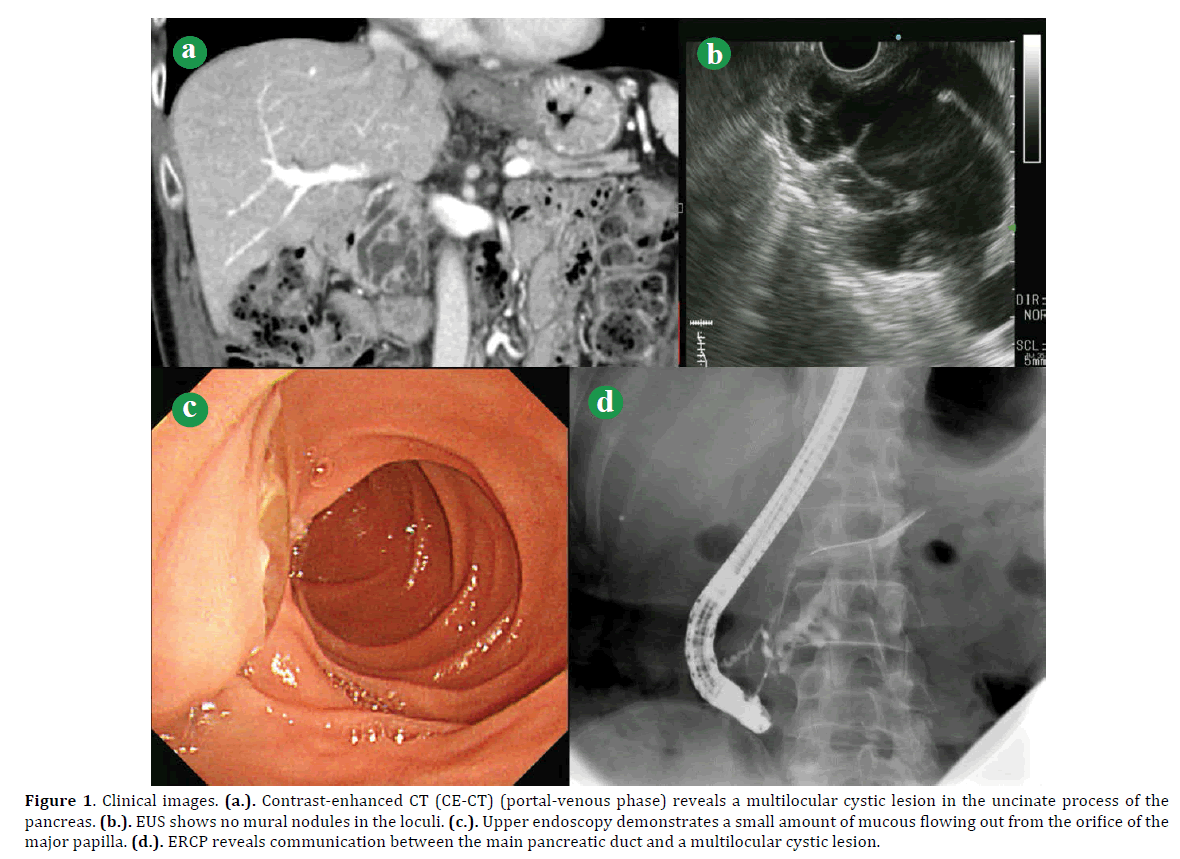
Figure 1. Clinical images. (a.). Contrast-enhanced CT (CE-CT) (portal-venous phase) reveals a multilocular cystic lesion in the uncinate process of the pancreas. (b.). EUS shows no mural nodules in the loculi. (c.). Upper endoscopy demonstrates a small amount of mucous flowing out from the orifice of the major papilla. (d.). ERCP reveals communication between the main pancreatic duct and a multilocular cystic lesion.
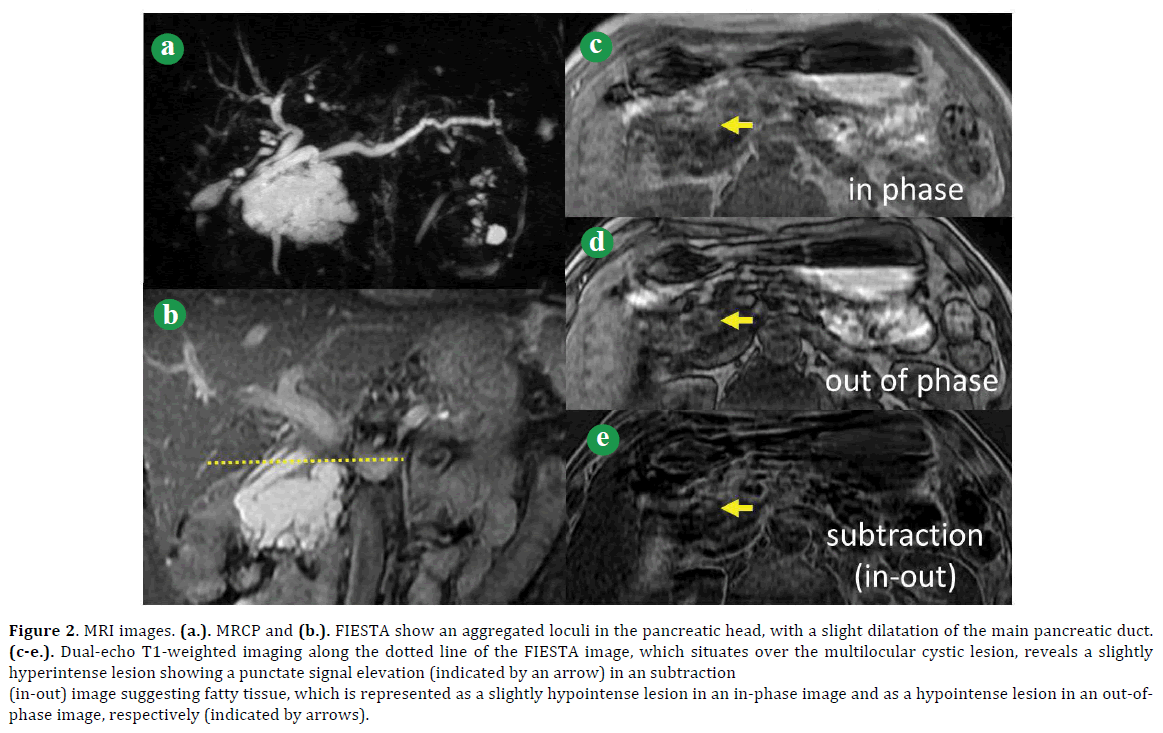
Figure 2. MRI images. (a.). MRCP and (b.). FIESTA show an aggregated loculi in the pancreatic head, with a slight dilatation of the main pancreatic duct. (c-e.). Dual-echo T1-weighted imaging along the dotted line of the FIESTA image, which situates over the multilocular cystic lesion, reveals a slightly hyperintense lesion showing a punctate signal elevation (indicated by an arrow) in an subtraction (in-out) image suggesting fatty tissue, which is represented as a slightly hypointense lesion in an in-phase image and as a hypointense lesion in an out-ofphase image, respectively (indicated by arrows).
PATHOLOGICAL FINDINGS
A multilocular cystic lesion measuring 50 x 45 mm in size was observed in the uncinate process of the pancreas. Excess mucous production was present and communication to the main pancreatic duct was confirmed (Figure 3). Histologically, each loculus was lined by tall columnar epithelium with pseudostratified spindle or oval nuclei and mucous cytoplasm showing flat to papillary proliferation (Figure 4), which was considered to be the intestinal-type IPMN with various grades of dysplasia and partially high-grade. Immunohistochemical staining using the avidin-biotin complex detection method with a BenchMark automated immunostainer (Ventana Medical Systems, Inc., Tucson, AZ, USA) showed negativity for MUC1 (Ma695, 100-fold dilution; Leica Biosystems Newcastle, Newcastle, UK) and p53 (DO-7, 800-fold dilution; Leica Biosystems Newcastle) and positivity for MUC2 (Ccp58, 200-fold dilution; Leica Biosystems Newcastle), MUC5AC (CLH2, 200-fold dilution; Leica Biosystems Newcastle), MUC6 (CLH5, 50-fold dilution; Leica Biosystems Newcastle), and CDX2 (AMT28, 50-fold dilution; Leica Biosystems Newcastle) (Figure 4). No invasive cancer component was associated with the IPMN and the main pancreatic duct was not affected by neoplastic cells. Small-sized, low-grade IPMNs or PanINs with the gastric phenotype were scattered in the branch ducts and peripheral ducts in the background pancreas.
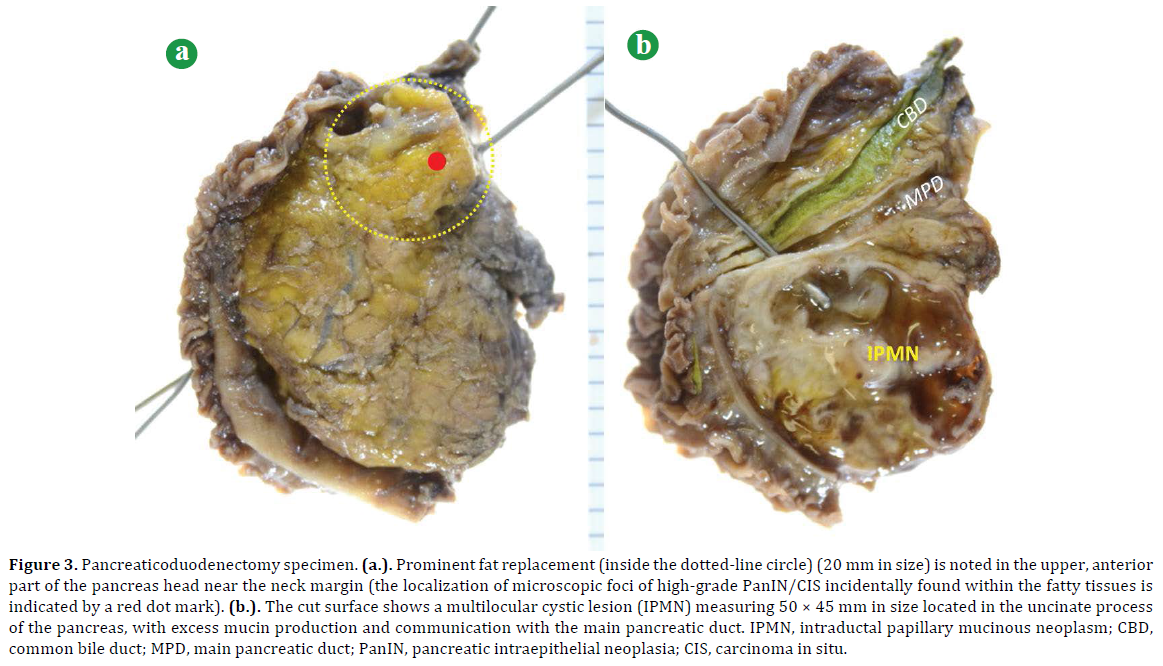
Figure 3. Pancreaticoduodenectomy specimen. (a.). Prominent fat replacement (inside the dotted-line circle) (20 mm in size) is noted in the upper, anterior part of the pancreas head near the neck margin (the localization of microscopic foci of high-grade PanIN/CIS incidentally found within the fatty tissues is indicated by a red dot mark). (b.). The cut surface shows a multilocular cystic lesion (IPMN) measuring 50 × 45 mm in size located in the uncinate process of the pancreas, with excess mucin production and communication with the main pancreatic duct. IPMN, intraductal papillary mucinous neoplasm; CBD, common bile duct; MPD, main pancreatic duct; PanIN, pancreatic intraepithelial neoplasia; CIS, carcinoma in situ.
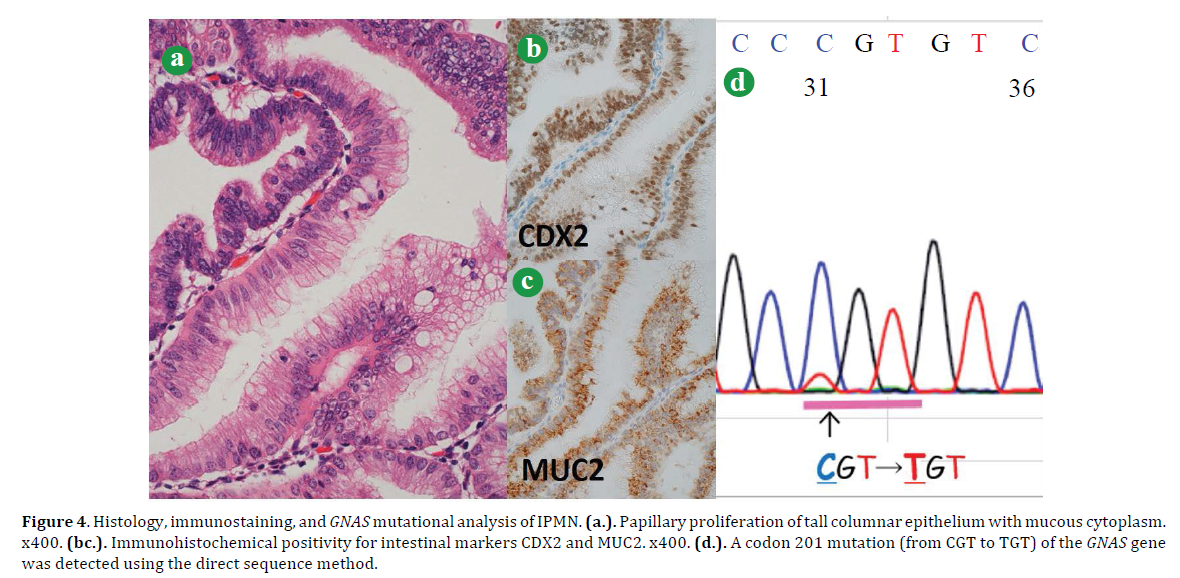
Figure 4. Histology, immunostaining, and GNAS mutational analysis of IPMN. (a.). Papillary proliferation of tall columnar epithelium with mucous cytoplasm. x400. (bc.). Immunohistochemical positivity for intestinal markers CDX2 and MUC2. x400. (d.). A codon 201 mutation (from CGT to TGT) of the GNAS gene was detected using the direct sequence method.
In addition, a prominent fatty area (approximately 20 mm in diameter) was observed in a part adjacent to the pancreatic resection margin (Figure 3), which was apart from IPMN in the uncinate process and corresponded to the region of signals suggesting fat on dual-echo T1WI (Figure 2). Microscopically, small foci of high-grade PanIN/CIS (less than 5 mm in a diameter) of the peripheral pancreatic ducts were found similar to islands within the fatty tissues (Figures 3, 5). The neoplastic ducts consisted of cuboidal to columnar epithelium (pancreatobiliary phenotype) showing low-papillary growth and were surrounded by a fibrous wall with mild inflammation. The immunohistochemical analyses showed positivity for MUC1, CDX2 (partially), and p53; and negativity for MUC2, MUC5AC, and MUC6.
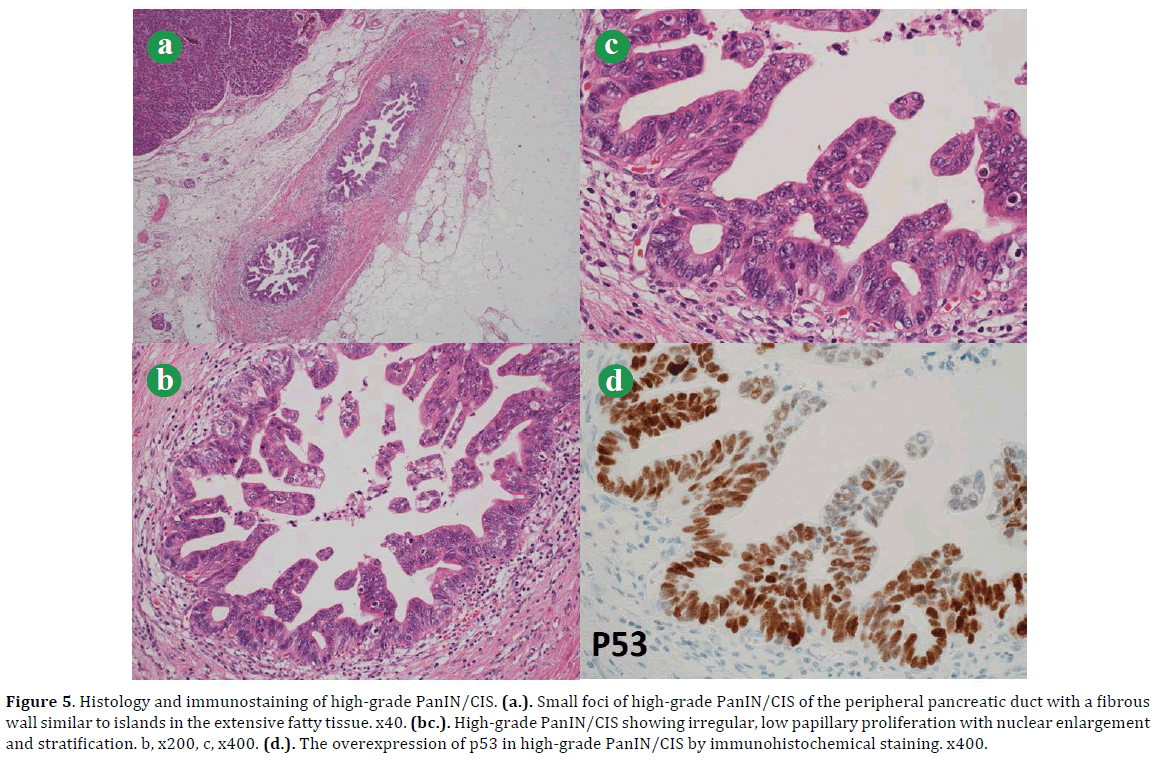
Figure 5. Histology and immunostaining of high-grade PanIN/CIS. (a.). Small foci of high-grade PanIN/CIS of the peripheral pancreatic duct with a fibrous wall similar to islands in the extensive fatty tissue. x40. (bc.). High-grade PanIN/CIS showing irregular, low papillary proliferation with nuclear enlargement and stratification. b, x200, c, x400. (d.). The overexpression of p53 in high-grade PanIN/CIS by immunohistochemical staining. x400.
MOLECULAR ANALYSES
KRAS and NRAS mutations by the PCR-rSSO method and GNAS mutation by the direct sequence method were analyzed for both IPMN and high-grade PanIN/CIS using formalin-fixed paraffin-embedded tissue sections. Analyses were conducted by a clinical examination company (SRL, Yokohama, Japan). As a result, KRAS mutations were detected in IPMN (G12R) and high-grade PanIN/CIS (G12V). Conversely, a GNAS mutation was detected in IPMN (codon 201 mutation from CGT to TGT) (Figure 4), but not in PanIN/CIS.
DISCUSSION
The two lesions of IPMN and high-grade PanIN/CIS in the present case were separately localized, with each exhibiting a distinctive morphology. IPMN was a macro-sized multilocular lesion of approximately 5 cm, which had communication with the main pancreatic duct and was accompanied by excess mucous production. Each loculus was histologically lined by tall columnar epithelium with mucous cytoplasm showing high papillary growth, various cellular dysplasia and intestinal cell lineage. Conversely, high-grade PanIN/CIS was a micro–sized lesion in the peripheral pancreatic duct encountered during the microscopic examination. The neoplastic ducts consisted of cuboidal to columnar cells with high-grade dysplasia showing flat to low-papillary growth, pancreatobiliary cell linage, and the overexpression of p53. In addition, genetic testing showed a GNAS mutation in IPMN, but not in high-grade PanIN/CIS, which is in accordance with data from previous reports that GNAS mutations are detected in approximately 40-70% of IPMNs, with a particularly high frequency (48-100%) in intestinal-type IPMNs; by contrast, the detection rate of a GNAS mutation in PanINs (as well as ordinary pancreatic ductal carcinomas) is very low [10- 12]. Moreover, different KRAS mutants were detected in IPMN (G12R) and high-grade PanIN/CIS (G12V). Therefore, the two neoplasms were regarded to be independent diseases morphologically and genetically; i.e., high-grade PanIN/CIS was concomitant with (not derived from) IPMN. This might simply be an incidental association.
As well as IPMNs, PanINs, especially high-grade ones, are pre-invasive lesions, and the detection of PanIN can lead to the early identification and treatment of pancreatic cancer. However, it is extremely difficult to directly identify high-grade PanINs in clinical images due to microscopic lesions. Therefore, careful attention should be paid to the secondary findings caused by PanINs. When high-grade PanIN/CIS occurs in the main pancreatic duct or its branch ducts, focal stenosis or mild dilatation of the affected ducts may be a clue for the identification of the lesions [13- 16]. In addition, secondary findings such as fibrosis (low echo in EUS) or inflammation of the surroundings of high-grade PanIN/CIS, retention cysts adjacent to highgrade PanIN/CIS, or dilatation of the caudal pancreatic duct could be helpful [13- 16]. Target cells may be directly obtained by pancreatic juice, leading to a cytological diagnosis of malignancy [17]. However, in the cases in which high-grade PanIN/CIS is localized to the peripheral pancreatic ducts, its identification may be impossible.
In the present case, atrophic and fibrotic changes in the pancreatic parenchyma (including so-called “lobulocentric atrophy” [9, 18- 20]) due to compression by IPMN itself, pancreatic duct obstruction by a mucous plug, or partial changes by microscopic low-grade IPMNs or PanINs scattered in the background pancreas were observed. Accordingly, various degrees of fatty replacements were noticed. In particular, fatty change of the high-grade PanIN/CIS region was so territorial and prominent that it was visualized in the fat tissue-demonstrating dual-echo TIWI images (although signals were so subtle to prove the certainty of the radiologic-pathologic correlation). Unfortunately, this area was not covered by the EUS examination, however, presumably punctate findings of low-echo images within the high-echo area (the former reflected high-grade PanIN/CIS and its surrounding fibrosis, while the latter reflected fat tissues) might have been observed. The prominent fatty change appeared to be related to high-grade PanIN/CIS, however, the precise pathogenesis was uncertain. Two phenomena were considered: one was that prominent fatty change of the pancreatic parenchyma gradually formed due to long-existing PanIN with increasing cellular dysplasia, while the other was that high-grade PanIN/CIS showing marked cellular atypia and p53 overexpression abruptly occurred in and obstructed the peripheral pancreatic ducts, resulting in rapid, prominent atrophic to fatty changes in the pancreatic parenchyma. Anyway, focal fatty change may be a helpful clue for screening peripheral high-grade PanIN/CIS, especially for patients with IPMN or familial pancreatic cancer. Accumulations of similar cases and further researches are required.
SUMMARY
We herein reported a surgically resected case of high-grade PanIN/CIS concomitant with branch duct type IPMN of the pancreas, in which distinct morphological and genetic phenotypes of the two lesions were clarified. Although it is extremely difficult to preoperatively identify peripheral high-grade PanIN/CIS, attentive and tenacious observation of secondary findings related to the microscopic lesions using various modalities may lead to a breakthrough.
Conflict of interest
All the authors have no conflicts of interest or financial ties to disclose.