- (2008) Volume 9, Issue 4
Itaru Naitoh1, Takahiro Nakazawa1, Hirotaka Ohara1, Tomoaki Ando1, Kazuki Hayashi1, Fumihiro Okumura1, Shozo Togawa2, Yasuhiro Kitajima2, Tessin Ban2, Katsuyuki Miyabe2, Koichiro Ueno2, Hiroaki Yamashita2, Takashi Joh1, Hitoshi Sano2
1Department of Gastroenterology and Metabolism, Nagoya City University Graduate School of Medical Sciences. Nagoya, Japan.
2Department of Gastroenterology, Gifu Prefectural Tajimi Hospital. Tajimi, Japan
Received April 14th, 2008 - Accepted May 29th, 2008
Context Obstructive jaundice in chronic pancreatitis is generally caused by stenosis of the bile duct in the pancreas. Obstructive jaundice caused by the impaction of a pancreatic stone in the papilla is markedly rare, with only seven cases reported to date. Case report We report a case of obstructive jaundice caused by the impaction of a pancreatic stone in the papilla. A 41-year-old male with chronic pancreatitis was admitted because of epigastric pain. Blood analysis revealed increased levels of hepatobiliary system enzymes, mild jaundice and an increase in pancreatic enzymes. Computed tomography revealed a number of pancreatic stones in the main pancreatic duct, and a stone with a diameter of about 1 cm in the pancreatic head. Swelling of the papilla was observed using duodenoscopy while endoscopic ultrasonography revealed a strong echo with acoustic shadows in the papilla. Percutaneous transhepatic biliary drainage was performed for the obstructive jaundice. Contrast medium from the percutaneous transhepatic biliary drainage route regurgitated into the pancreatic duct and revealed the impaction of pancreatic stones in the common channel. The patient was referred to our hospital for treatment of the stone impaction. We performed a needle knife precut papillotomy and extracted a white stone which was diagnosed as a pancreatic stone by composition analysis. Conclusion Impaction of a pancreatic stone in the papilla is a markedly rare cause of obstructive jaundice in chronic pancreatitis. A needle knife precut papillotomy was effective in removing the impacted pancreatic stone in the papilla.
Calculi; Jaundice, Obstructive; Pancreatitis, Chronic; Sphincterotomy, Endoscopic
PTBD: percutaneous transhepatic biliary drainage
Obstructive jaundice in chronic pancreatitis is caused by stenosis of the bile duct and requires biliary drainage. Although obstructive jaundice by impaction of a biliary stone in the papilla is common, obstructive jaundice caused by impaction of a pancreatic stone in the papilla is rare [1, 2, 3, 4, 5, 6]. To date, cases of obstructive jaundice caused by the impaction of a pancreatic stone in the papilla have been treated with surgery and endoscopic procedures.
Endoscopic biliary drainage for obstructive jaundice is now a common procedure. A precut papillotomy is also occasionally performed if endoscopic biliary cannulation is difficult. In the past, it was believed that only expert endoscopists should perform precut papillotomies because of the high complication rate. In fact, however, the complication rate is comparable to that of a standard sphincterotomy [7, 8].
We herein report a case of obstructive jaundice resulting from the impaction of a pancreatic stone in the papilla. The impacted pancreatic stone was successfully extracted with a needle knife papillotomy.
472 IU/L (reference range: 37-125 IU/L). Computed tomography (CT) revealed a number of pancreatic stones in the main pancreatic duct, and a stone with a diameter of about 1 cm in the pancreatic head (Figure 1). Magnetic resonance cholangiopancreatography (MRCP) showed dilation of the main pancreatic duct and common bile duct, and a number of hypointense regions in the main pancreatic duct. Duodenoscopy showed swelling of the papilla while endoscopic ultrasonography revealed a strong echo with acoustic shadows in the papilla.
Conservative treatment led to resolution of the epigastric pain and normalization of the elevated pancreatic enzymes. However, since the jaundice was aggravated, percutaneous transhepatic biliary drainage (PTBD) was performed. The contrast medium from the PTBD route regurgitated into the pancreatic duct and revealed impaction of the calcified stone in the papilla (Figure 2). The patient was then referred to our hospital where the impacted pancreatic stone was treated endoscopically. Since a conventional papillotome could not be inserted into the region because of the presence of the impacted stone, a needle-knife precut papillotomy was performed. The precut incision was extended to the roof of the papilla in a 12 o’clock direction, and a whitish stone measuring 10x8 mm was exposed at the site of excision and removed with the basket (Figure 3).
Composition analysis by infrared spectroscopy indicated that 99% of the stone was calcium carbonate, leading to the diagnosis of a pancreatic stone. Cholangiography from the PTBD route after the precut papillotomy was normal and the flow of contrast medium to the duodenum was observed. The PTBD tube was removed several days later. Endoscopic retrograde cholangiography revealed that the stones in the main pancreatic duct of the pancreas head had disappeared spontaneously. Extracorporeal shock wave lithotripsy ESWL) was performed to extract the stones in the tail of the pancreas, following which no stones were detected.
Chronic pancreatitis is known to often be associated with obstructive jaundice or pancreatic stones. The incidence of chronic pancreatitis accompanying stenosis of the bile duct caused by inflammatory swelling of the pancreas head or a pseudocyst is 10-30% [9, 10, 11, 12], of which 28% of cases are complicated by obstructive jaundice or cholangitis, requiring treatment [12]. Obstructive jaundice and acute pancreatitis caused by the impaction of a biliary stone in the papilla are sometimes encountered, but obstructive jaundice caused by the impaction of a pancreatic stone in the papilla is markedly rare, with only seven cases reported to date [1, 2, 3, 4, 5, 6]. Table 1 summarizes these previous cases and our present case.
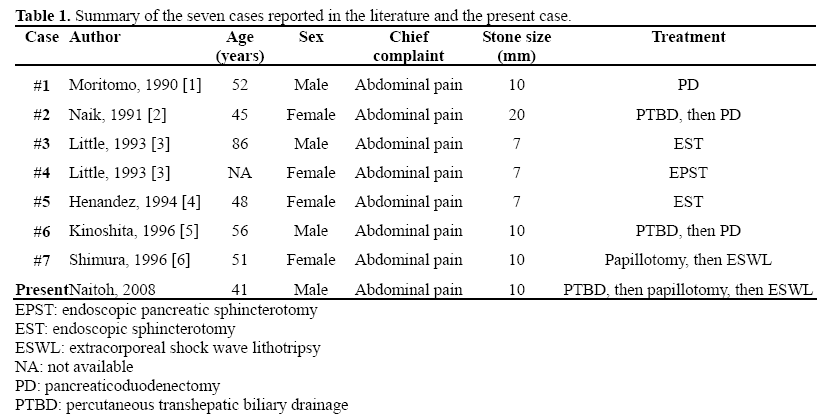
The mechanism of the development of obstructive jaundice caused by pancreatic stones may be similar to that of pancreatitis caused by biliary stones. Impaction of pancreatic stones in the common channel or main pancreatic duct near the papilla results in obstruction of the bile duct, leading to obstructive jaundice. While biliary stone-induced pancreatitis is considered to be caused mainly by small stones, the pancreatic stones causing impaction in the papilla in the seven patients reported to date were relatively large, measuring 7 to 20 mm. Surgical treatment was performed in three of the seven patients, of whom two had a long common duct (20 mm) and malfusion of the pancreatobiliary ducts. [1,5]. Notwithstanding the small number of patients, impaction in the papilla was considered to more likely occur in patients having a long common duct and large pancreatic stones.
Endoscopic methods are generally used for the treatment of obstructive jaundice caused by the impaction of biliary stones in the papilla. Obstructive jaundice caused by the impaction of pancreatic stones in the papilla was treated endoscopically in four of the seven patients reported to date [3, 4, 6] while the remaining three underwent surgical treatment [1, 2, 5]. Endoscopic methods included endoscopic sphincterotomy, endoscopic pancreatic sphincterotomy and needle knife precut papillotomy, and the stone was removed using a balloon or basket. In three of the four patients who underwent endoscopic treatment, the impacted pancreatic stone in the papilla was released while performing cannulation; endoscopic sphincterotomy was performed in two of the three patients and endoscopic pancreatic sphincterotomy in one, followed by stone extraction with a basket or balloon. In the remaining patient, as in our patient, the impacted stone was not released by cannulation, and extraction was instead done by needle knife precut papillotomy [6].
Precut papillotomy is performed when biliary cannulation is difficult. The general opinion has been that precut papillotomy should be performed only by expert endoscopists because of its high rate of complications such as acute pancreatitis and perforation. However, recent reports suggest that the frequency of acute pancreatitis is 0% to 2%, which is comparable to that of a standard sphincterotomy [7, 8]. Needle knife precut papillotomy is also used for impaction of biliary stones in the papilla, in which the impacted stones are often released at the time of cannulation, and a conventional papillotome can be inserted. However, if the impacted stones are not released, a needle knife papillotomy should be performed.
Until development of the less invasive endoscopic pancreatic sphincterotomy method, surgical treatment was the primary method for the removal of pancreatic stones. Since then, the extraction of pancreatic stones using a basket catheter has been performed. In patients with chronic pancreatitis, however, the pancreatic duct often bends and is stenosed. Because the stone is sometimes large and impacts the pancreatic duct, endoscopic removal alone may be difficult. Since first being applied to the treatment of pancreatic stones [13] in 1986, the adoption of ESWL has been rapid, thanks to its high efficiency in stone clearance, safety and usefulness for stones which are difficult to remove endoscopically. In many countries, it is common to first attempt an endoscopic method and then apply ESWL in cases in which the endoscopic method alone is not sufficient. In Japan, treatment with ESWL alone has provided good results [14, 15], and endoscopic methods are additionally used depending on the condition of the patient.
The number of pancreatic stones caused by chronic pancreatitis is often large [15]. In our patient, there was a pancreatic stone in the pancreatic head, measuring about 7 mm, which was spontaneously released, probably because a precut papillotomy was performed. A large number of pancreatic stones were also present in the tail of the pancreas. Additional ESWL was performed because of the possibility of impaction of these stones. In patients with impacted stones in the papilla and many other stones in the pancreatic duct, a precut papillotomy is considered effective in reducing the risk of papillary re-impaction.
In our case, since PTBD had already been performed, ESWL might have been selected as the first treatment method for the impacted stone. However, endoscopic treatment can improve the jaundice and remove stones at the same time. The PTBD tube was removed immediately. Otherwise, ESWL requires many sessions and if the impacted stone is removed by ESWL, the remaining stones might be re-impacted in the papilla. We therefore selected endoscopic treatment. In patients in whom the insertion of a papillotome is impossible due to the impaction of pancreatic stones in the papilla, as in our patient, a needle knife precut papillotomy is useful because it allows improvement of jaundice and removal of the stones at the same time.
Obstructive jaundice caused by the impaction of pancreatic stones in the papilla is markedly rare. A needle knife precut papillotomy is considered useful in treating this condition.
The authors have no potential conflicts of interest