Herraiz Roda JL1,2*, Maazouzi Y1, Llueca Abella A1,2, Delgado Barriga K3, Piquer Simó D1, Guijarro Colomer M1, and Cañete Mota A1
1Department of Obstetrics and Gynecology, General Hospital of Castellon, Spain
2Department of Medicine, University Jaime I, Castellon, Spain
3Department of Radiology, General Hospital of Castellon, Spain
*Corresponding Author:
Herraiz Roda JL
Department of Medicine, University Jaime I. Castellon, Spain
Tel: +34964728000
E-mail: sgo.herraiz@gmail.com
Received date: January 18, 2016 Accepted date: March 08, 2016 Published date: March 09, 2016
Keywords
Urethrocutaneous fistula; Transobturator tape; Recurrent vulvar abscess; Female patient
Introduction
The transobturator tape procedure (TOT) is a highly effective technique used to resolve cases of female stress urinary incontinence. It is a safe procedure with relatively few peroperative and early post-operative complications compared to the tension free vaginal tape (TVT). Nevertheless, recent studies have demonstrated that the incidence of late postoperative complications following a TOT procedure are relatively frequent and include: perineal pain, de novo dyspareunia, and vaginal erosion [1].
The urethrocutaneous fistula is an uncommon complication in the female population that is defined as an abnormal connection between the urethra and the skin, usually affecting the perineum [2]. It may develop as a surgical complication of urethral strictures, repair of hypospadias [3], prostate surgery, chronic untreated periurethral abscesses, trauma and parasitic infections involving Schistosoma hematobium o Dracunculus medinensis in endemic regions [4,5]. In the female population of developing countries, the incidence of urogenital fistulas is mainly caused by obstetric injuries and severe pelvic pathology due to the high prevalence of untreated gonorrhea and other sexually transmitted diseases [6]. In contrast, such fistulas are much less frequent in developed countries and are most often seen as sequelae of gynecologic interventions, and less often as complications of obstructed labor during childbirth [7,8]. Although rare in female patients, the incidence of urethrocutaneous fistula after hypospadias repair varies from 4 to 28% of all cases and remains problematic for pediatric urologists despite the progress in surgical techniques [3]. Patients suffering from this type of fistula usually present recurring perineal infection or urine trickling [2]. As for its diagnosis, a cystourethroscopy allows a direct visualization of the fistula; however, the radiographic diagnosis depends fundamentally on the retrograde urethrography and fistulography, since both can demonstrate the location of the communication. In case of abscess formation, an associated complication, a CT scan may be useful [2,5].
We present a case of a 53 years old woman who developed a urethrocutaneous fistula after a TOT procedure four years ago as a surgical treatment of female stress urinary incontinence which was diagnosed recently after presenting various episodes of vulvar abscesses.
Case Description
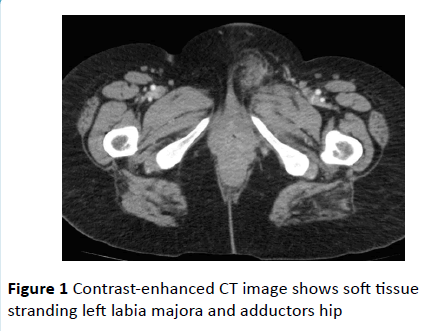
A 49-year-old woman, G2P2 with no personal medical history of interest, underwent a TOT procedure to treat her stress urinary incontinence in 2011. There were no incidents during the surgery and no per-operative or early postoperative complications were reported. The patient did not refer any urogenital symptoms until April of 2014 when she visited the gynecology emergency room due to a painful left vulvar 5 cm fluctuating mass which was diagnosed as a labia majora abscess, and was treated with cloxacillin per os. The patient visited the ER once again on May of 2014 due to the persisting mass. An inguinal ultrasound was performed in order to rule out an inguinal hernia in the differential diagnosis. The patient’s blood work revealed a leukocytosis of 18,000/mm3 and a high level of C-reactive protein, compatible with an inflammatory process, and was subsequently hospitalized in our gynecology ward in order to receive intravenous antibiotherapy (Figure 1).
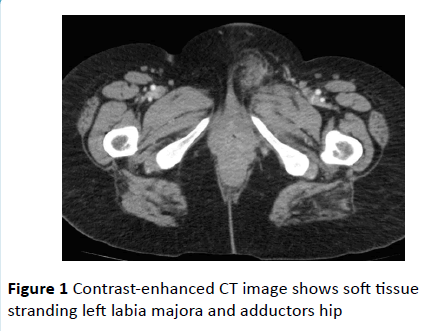
Figure 1 Contrast-enhanced CT image shows soft tissue stranding left labia majora and adductors hip
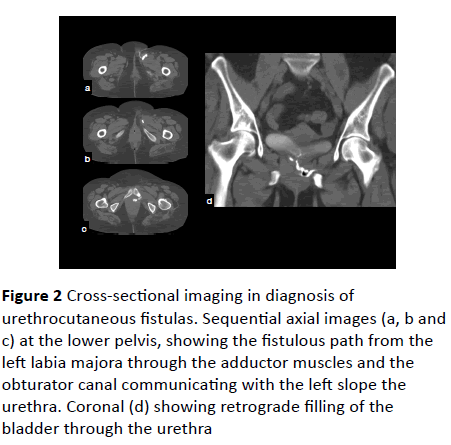
Due to the lack of response to the medical treatment, the abscess was incised and drained under anesthesia, and the patient was discharged two days later. Our patient received a postoperative follow-up and once again presented a left vulvar abscess which was spontaneously draining a purulent discharge from the mons pubis. A pelvic MRI was performed in order to study the tumor, which revealed the fistulized abscess. The patient underwent a second intervention in February of 2015 which included the exeresis of the fistulized vulvar abscess, reaching the left round ligament. The patient received intraoperative prophylactic antibiotics and was discharged with amoxicillin per os, experiencing a lessening although not a complete disappearance of the symptoms (Figure 2).
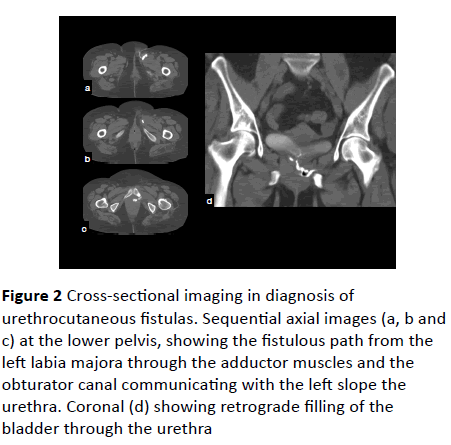
Figure 2 Cross-sectional imaging in diagnosis of urethrocutaneous fistulas. Sequential axial images (a, b and c) at the lower pelvis, showing the fistulous path from the left labia majora through the adductor muscles and the obturator canal communicating with the left slope the urethra. Coronal (d) showing retrograde filling of the bladder through the urethra
She was then referred to our hospital’s urology department for further evaluation. A physical exam of the genital area revealed an indurated area in the left side of the anterior vaginal wall, involving the left suburethral sling territory. A fistulography was then performed, which confirmed the urethrocutaneous fistula. The patient underwent a fistulectomy and exeresis of the suburethral sling in October of 2015. She also received intraoperative antibiotherapy, as well as oral amoxicillin/clavulanic acid during the following 10 days, and the Foley catheter was maintained during the following three weeks post-surgery. Six months later, in the postoperative follow-up, the patient referred mixed incontinence and is currently being treated with Mirabegron 50mg.
Discussion
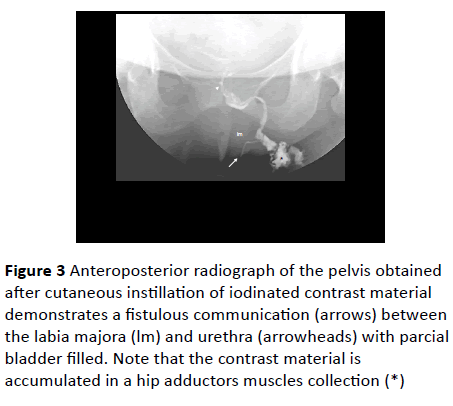
The late postoperative complications of the TOT procedures are most likely underreported and, although less frequent than in TVT procedures, should be taken into account and properly explained to the patient preoperatively. The Kaelin-Gambirasio et al. [1] study concludes that an important risk factor for erosion, one constituting 60% of the associated complications according to Boyles et al. [9] is the type of sling material used for the TOT, such as the Obtape® sling. The urethrocutaneous fistula is a very rare postsurgical complication y is most frequently seen in male patients having undergone hypospadias repair surgery. The small sized urethrocutaneous fistulas may heal spontaneously; however, most fistulas require surgical correction [10] (Figure 3).
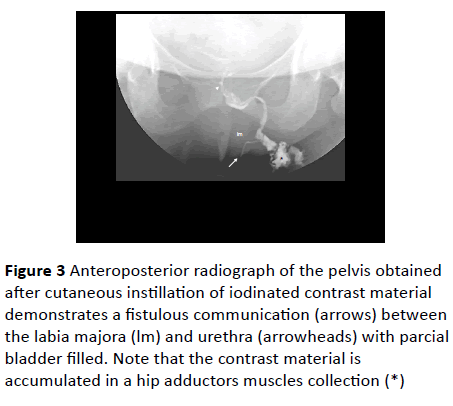
Figure 3 Anteroposterior radiograph of the pelvis obtained after cutaneous instillation of iodinated contrast material demonstrates a fistulous communication (arrows) between the labia majora (lm) and urethra (arrowheads) with parcial bladder filled. Note that the contrast material is accumulated in a hip adductors muscles collection (*)
The type of sling used in the TOT procedure in 2011 is unkown, which hinders the cause and effect hypothesis. Knowing the type of mesh might have helped us determine whether the TOT sling was truly the cause of the urethrocutaneous fistula, although we can only infer that our patient’s case is a consequence of the surgery, due to the lack of studies regarding the incidence of urethrocutaneous fistula following a TOT surgery. Further studies involving various cases of urethrocutaneous fistulas are needed to reach valid conclusions.
Conclusion
The urethrocutaneous fistula is a rare post-surgical complication that occurred in a 53 year old patient, after a TOT procedure four years ago, who presented various episodes of recurring left vulvar abscesses. The fistulectomy and exeresis of the suburethral sling followed by the administration of wide spectrum antibiotics resolved the case and the patient is currently asymptomatic. Various studies are needed in order to confirm the association between the TOT surgery and the urethrocutaneous fistula complication.
References
- Kaelin-Gambirasio I, Jacob S, Boulvain M, Dubuisson J, Dallenbach P (2009) Complications associated with transobturator sling procedures: analysis of 233 consecutive cases with a 27 months follow-up. BMC Women's Health 9(1): 28.
- Burivong W, Leelasithorn V, Varavithya V (2011) Common lower urinary tract fistulas: A review of clinical presentations, causes and radiographic imaging. International Journal of Case Reports and Images 2(1): 1.
- Chung J, Choi S, Kim B, Chung S (2012) Risk Factors for the Development of Urethrocutaneous Fistula after Hypospadias Repair: A Retrospective Study. Korean Journal of Urology 53(10): 711.
- Coulibaly N, Sangaré I (2015) Urethrovaginal Fistula in a 5-Year-Old Girl. Case Reports in Urology 1-4.
- Yu N, Raman S, Patel M, Barbaric Z (2004) Fistulas of the Genitourinary Tract: A Radiologic Review1. RadioGraphics, 24(5): 1331-1352.
- Olajide A, Olajide F, Kolawole O, Oseni I, Ajayi A (2013) A Retrospective Evaluation of Challenges in Urethral Stricture Management in a Tertiary Care Centre of a Poor Resource Community. Nephro-Urology Monthly 5(5): 974-977.
- Waaldijk K (1989) The surgical management of bladder fistula in 775 women in Northern Nigeria. Benda BV, Nymegen.
- Wall LL, Karshima JA, Kirschner C, Arrowsmith SD (2004) The obstetric vesicovaginal fistula: characteristics of 899 patients from Jos, Nigeria. Am J ObstetGynecol 190: 1011.
- Boyles S, Edwards R, Gregory W, Clark A (2006) Complications associated with transobturator sling procedures. International Urogynecology Journal 18(1): 19-22.
- Waterman B, Renschler T, Cartwright P, Snow B, Devries C (2002) Variables in Successful Repair of Urethrocutaneous Fistula After Hypospadias Surgery. The Journal of Urology 726-730.