Research Article - (2023) Volume 8, Issue 6
A Comparison of Occupational Blood Lead Level (BLL) Prevalence and Airborne Lead Concentration in Utah and Nationally
Kuhre J,
Sleeth D,
Handy R* and
Schaeffer C
Department of Family and Preventive Medicine, Cihan University-Ebril, Kurdistan, Iraq
*Correspondence:
Handy R, Department of Family and Preventive Medicine, Cihan University-Ebril, Kurdistan,
Iraq,
Tel: 3854198722,
Email:
Received: 23-Mar-2023, Manuscript No. IPJHMCT-23-15934;
Editor assigned: 27-Mar-2023, Pre QC No. IPJHMCT-23-15934 (PQ);
Reviewed: 10-Apr-2023, QC No. IPJHMCT-23-15934;
Revised: 23-May-2023, Manuscript No. IPJHMCT-23-15934 (R);
Published:
30-May-2023, DOI: 10.21767/2473-6457.23.6.51
Abstract
The healthy people 2010 lead objective sought to reduce the number of employees occupationally exposed to lead with Blood Lead Levels (BLLs) ≥ 25 μg/dL to 0. Concurrently, occupational limits have been set at 50 ug/m3 for lead in the air. To determine whether Utah and the U.S. met these prior national goals, this retrospective study compared elevated BLL prevalence from Utah and U.S. employees from 2000-2009 against the healthy people 2010 goal. Lead air concentrations were also compared against U.S. Occupational Exposure Limits (OELs). Results found that elevated BLL prevalence statistically significantly declined for both Utah and the nation but did not reach the intended goal of healthy people 2010. Lead air concentrations similarly declined but were higher than proposed OELs, suggesting additional research is needed.
Keywords
BLLs; Air concentrations; Demolition; Public health; Reproductive systems
Introduction
Occupational exposure to lead continues to threaten worker
health, with an estimated 1.6 million workers regularly
exposed to lead [1]. The construction industry accounts for
nearly half of these, as these workers frequently perform
demolition, renovation, and remediation of buildings
constructed prior to the banning and widespread
discontinuation of lead based paint in the 1970’s [2]. Two
other industries at risk for lead exposures are metalworking
(melding and manufacturing) and the manufacturing of lead
acid batteries, the latter of which accounts for 70% of the lead
used in the United States today [3,4]. In these industries, the
primary exposure route of lead is through inhalation [5].
While lead exposures are sometimes resolved through a
natural excretion process, if the level of intake is higher than
the rate of excretion, it can cause Blood Lead Levels (BLL) to
rise. In the U.S., 95% of elevated BLL (defined as ≥ 25 μg/dL)
in adults are associated with work related exposures.
Lead is associated with numerous adverse health effects and
considerable financial costs. The health impacts of lead
exposure range broadly from impairments to daily functioning
(e.g. depression and poor concentration) to damage to the
cardiovascular, nervous, kidney, and reproductive systems.
One estimate in 2016 found that while the direct medical
costs associated with occupational lead exposure were $141
million, including the indirect costs due to lost work time and
productivity brought the total as high as $392 million [6]. In
fact, the true costs of occupational lead exposure may be
higher, as any exposure to lead at work can also lead to
employees carrying lead contamination home.
Reducing exposure to lead has become a leading occupational
safety priority. OSHA concurs with recommended exposure
limits from the National Institute for Occupational Safety and
Health (NIOSH), and the American Conference of
Governmental Industrial Hygienists (ACGIH), which are all set
at 50 μg/m3 for an 8 hour shift [7-9]. However, there is a
considerable discrepancy between regulations and recommendations in terms of BLL. In 2015, in response to
additional research on associations between lead exposure
and increased mortality by cardiovascular disease and cancer,
NIOSH reduced the maximum recommended adult BLL to 5
μg/dL [10-12]. However, OSHA regulations require only that
employees with BLLs ≥ 50 μg/dL (for the construction industry)
and ≥ 60 μg/dL (for general industry) be removed from work
until their levels have decreased to ≤ 40 μg/dL [13]. Given that
both general scientific consensus and that NIOSH’s
recommendations are substantially lower, such regulations
may result in at risk occupational populations experiencing
high levels of exposure.
Several surveillance programs have been instituted to monitor
occupational lead exposure, but air levels and BLL are tracked
separately. OSHA records air sample results into the Chemical
Exposure Health Data (CEHD), which includes personal, area,
and bulk air samples on various toxic agents, including lead air
levels [14]. NIOSH’s Adult Blood Lead Epidemiology and
Surveillance (ABLES) program tracks laboratory-reported BLLs
in adults that are occupationally exposed to lead. The most
recent ABLES data (2016) for 26 out of the participating 37
states puts the prevalence of BLLs ≥ 25 μg/dL at 2.8 per
100,000 employed adults 16+ years old, and the prevalence
for BLLs ≥ 10 μg/dL at 15.8 per 100,000 working adults 16+
years old [15]. These data are a key source of information for
Healthy People, a nationwide initiative by the U.S.
Department of Health and Human Services (DHHS) that seeks
was to reduce the number of employees occupationally
exposed to lead with BLLs ≥ 25 μg/dL to 0.16 [16,17]. As of
2020, 41 states contribute to the ABLES program, which
requires that participating states share all BLL data. However
CEHD and ABLES have not yet been combined for analysis.
To examine the efficacy of lead exposure recommendations
and regulations, this study compares BLL prevalence in the
state of Utah and nationwide using the healthy people 2010
goal and timeline (2000-2009) as a benchmark: Prevalence per
100,000 employed adults with BLLs ≥ 25 ug/dL for each year in
both Utah and the nation. Air concentrations from the same
period in the CEHD will be compared with national BLL
prevalence and U.S. Occupational Exposure Limits (OELs).
Utah was chosen for state level analysis because Utah has
multiple industries where workers risk lead exposure (an
estimated 236,030 jobs, or 16.2% of the employed
population), including smelting and refining of metals, power
plant activity, and mine tailings. We hypothesize that:
• There was a statistically significant decrease in the
prevalence of elevated BLL between the years 2000 and
2009 for workers in the state of Utah and the U.S. as a
whole.
• That this decrease coincides with a decline in reported
lead air concentration levels.
Materials and Methods
To determine the changing prevalence of employed adults
with BLLs ≥ 25 ug/dL, a retrospective investigation was
conducted using data from the national ABLES dataset from the years 2000-2009 and Utah’s Environmental Public Health
Tracking Network (EPHTN), Utah’s contribution to the ABLES
program. BLL data are collected through local clinical
laboratories and are reported on a weekly or monthly basis,
then stored in the Utah Blood Lead Registry (UBLR).
A secondary analysis examined the same time frame, but
compared the ABLES dataset to OSHA’s CEHD to determine if
the change in elevated BLL prevalence was associated with
any change in lead air concentration. As these data are public
and de-identified, no Institutional Review Board (IRB)
approval was required.
All BLL data was from either the Utah EPHTN or the ABLES
dataset and collected between the years of 2000-2009. BLLs
from unemployed adults and children were excluded. Lead air
concentrations between 2000-2009 from OSHA’s CEHD were
also extracted. Only data from personal samplers with
concentration values listed in mg/m3 were included from
CEHD.
Data from the EPHTN and ABLES dataset were available in
Excel (Microsoft, Redmond, WA) format and did not require
cleaning. Data extracted from the CEHD were cleaned and
converted to Excel for analysis in SAS 9.4 (SAS Institute, Cary,
NC). The OSHA data cleaning application process, which
included removal of all blanks, duplicates, and erroneous
data, was used.
After this process, more than 20% of the CEHD data (per year)
still contained multiple concentrations measured below the
limit of detection that prohibited statistical analysis. An
iterative approach was therefore used to estimate the
measured amount of lead in the air for each non-detectable
concentration. This was accomplished by using the “ND Expo–
Treatment of non-detects in industrial hygiene samples” web
application. As this application requires that at least 20% of
the data be detectable sample, the 2009 lead concentration
year (which had 18% of detectable data) was excluded from
analysis.
All datasets were tested for normality using the Shapiro-Wilks
test (W-statistic). As the data were found to be normally
distributed, parametric tests were then used to generate a
time series for each dataset throughout the decade. To
investigate the presence of declines in high BLL prevalence in
Utah and the nation, and statistically significant reductions in
national air lead concentrations for the period, linear
regressions were generated for each variable. For all analyses,
an alpha level of 0.05 was used. Finally, linear regression was
used to compare:
• Utah’s BLL prevalence to the nation’s BLL prevalence.
• Nation’s BLL prevalence to lead air concentration.
Results
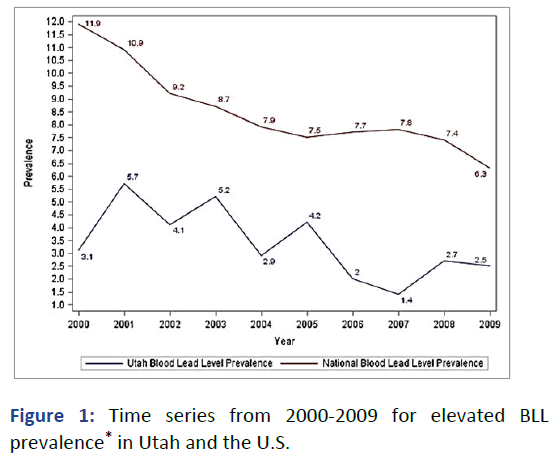
Both the national and Utah BLL prevalence per 100,000
employed adults 16+ years old with BLLs ≥ 25 ug/dL between
declined between 2000-2009 (Figure 1) from 11.9 in 2000 to
6.3 in 2009.
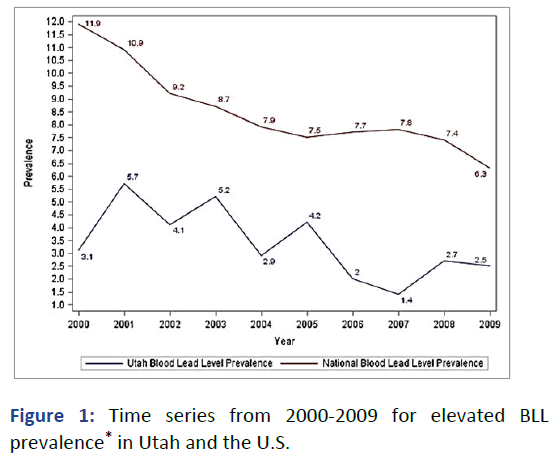
Figure 1: Time series from 2000-2009 for elevated BLL
prevalence* in Utah and the U.S.
*Per 100,000 employed adults 16+ years old with BLLs ≥ 25
ug/dL.
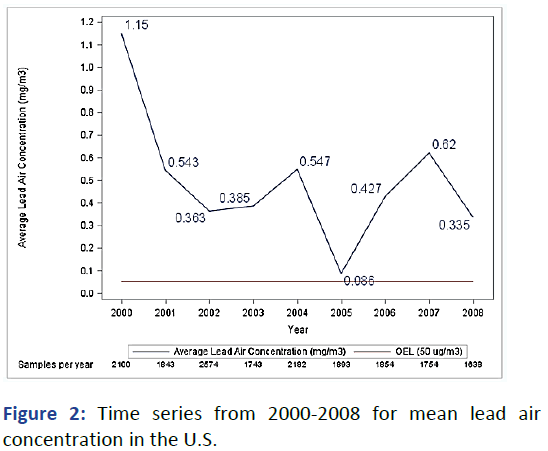
However, national mean lead air concentrations were
recorded above the OEL every year between 2000-2008
(Figure 2). Average lead air concentration peaked in 200
at 1.15 mg/m3, but decreased afterwards with a low of
0.086 mg/m3 in 2005.
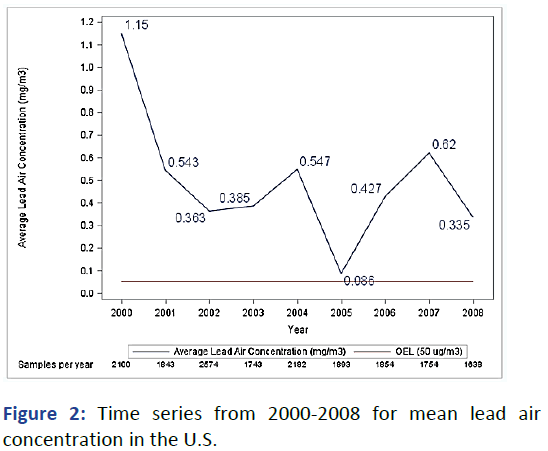
Figure 2: Time series from 2000-2008 for mean lead air
concentration in the U.S.
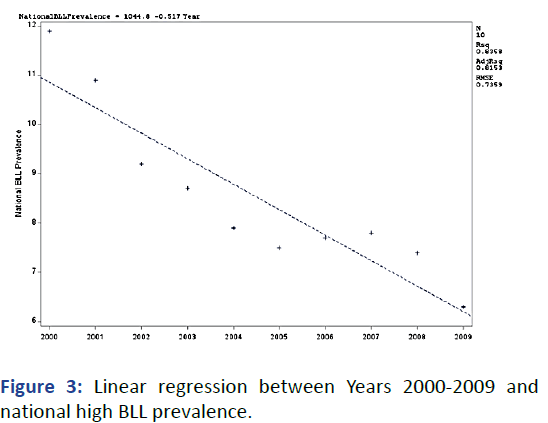
The nation’s BLL prevalence had an overall decline of 0.517
per year, with an R2 of 0.84 and p-value of 0.0002 (alpha 0.05)
(Figure 3) suggesting that time accounts for the variance in
national BLL prevalence.
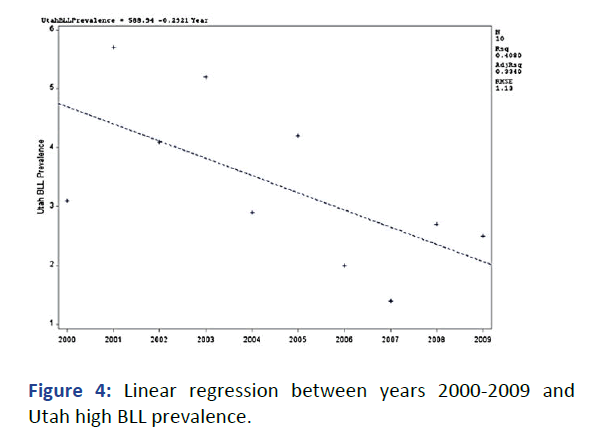
Utah’s elevated BLL prevalence, conversely, maintained a
pattern of rising and falling until 2007, when the prevalence
decreased to 1.4 per 100,000 employed adults 16+ years old
(Figure 4). Utah’s high BLL prevalence decline was 0.292 per
year, with a weak R2 of 0.41. The linear regression’s slope pvalue
(Table 1) was 0.0468, demonstrating statistical
significance.
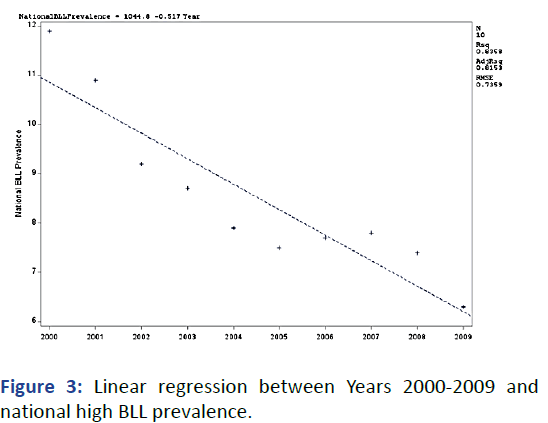
Figure 3: Linear regression between Years 2000-2009 and
national high BLL prevalence.
*Per 100,000 employed adults 16+ years old with BLLs ≥ 25
ug/dL.
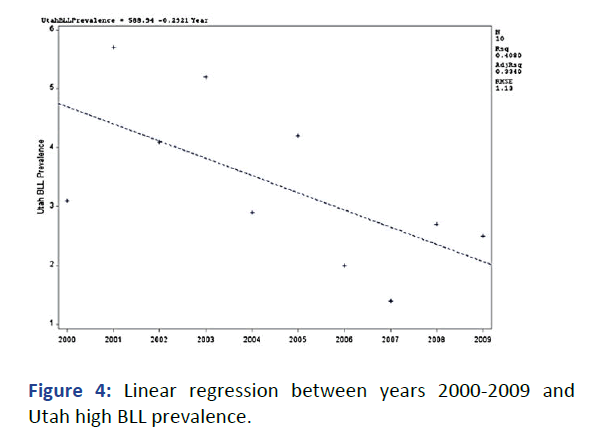
Figure 4: Linear regression between years 2000-2009 and
Utah high BLL prevalence.
*per 100,000 employed adults 16+ years old with BLLs ≥ 25 ug/
dL.
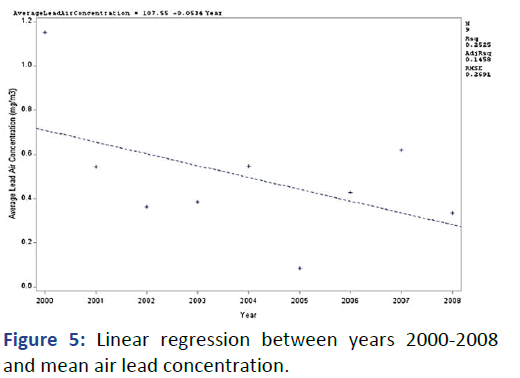
The mean air lead concentration over time (Figure 5) was
estimated to decline 0.053 mg/m3 per year; however, the R2 value was 0.25, while the slope’s p-value was 0.1680 (Table 1),
indicating that the slope is not significantly declining.
Although the model was able to predict a decline in air lead
concentration, the high p-value and low R2 suggest that more
information is needed to improve the model.
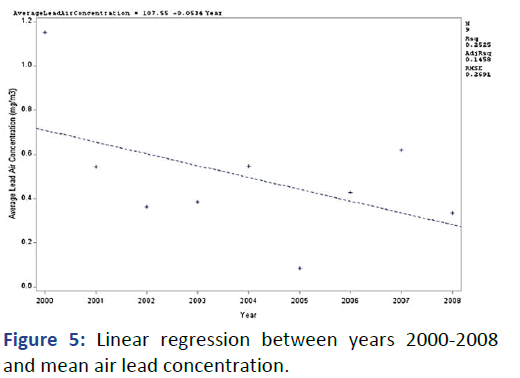
Figure 5: Linear regression between years 2000-2008
and mean air lead concentration.
| Dataset |
Slope |
p-value |
| Utah BLL prevalence |
-0.2921 |
0.0468 |
| National BLL prevalence |
-0.517 |
0.0002 |
| Average air lead concentration |
-0.0534 |
0.168 |
Note: BLL; Blood Lead Level.
Table 1: Slope and p-value for the three linear regressions over time.
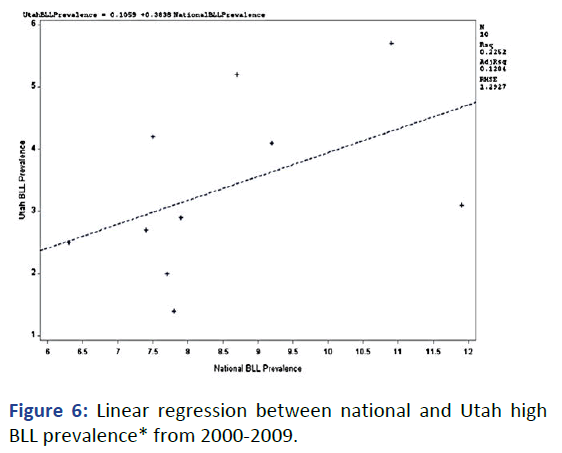
Figure 6 is the linear regression comparing Utah’s high BLL
prevalence to the nation’s high BLL prevalence from
2000-2009. To predict Utah’s BLL prevalence from national
prevalence, it was decided that the national BLL prevalence
would be the x-variable with Utah’s BLL prevalence as the yvariable.
This setup seems more practical to estimate
individual state prevalence from a single dataset such as
ABLES. Setting the regression in this way demonstrates a 0.38
prevalence increase in Utah to a single prevalence increase in
the nation. But the model has a very weak R2 of 0.23,
suggesting it is not appropriate for prediction.
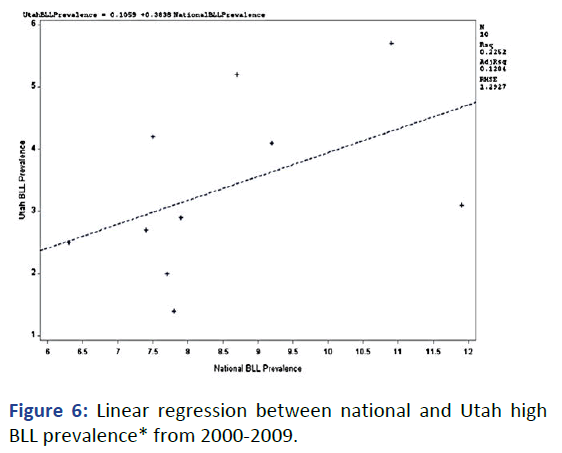
Figure 6: Linear regression between national and Utah high
BLL prevalence* from 2000-2009.
*Per 100,000 employed adults 16+ years old with BLLs ≥ 25
ug/dL.
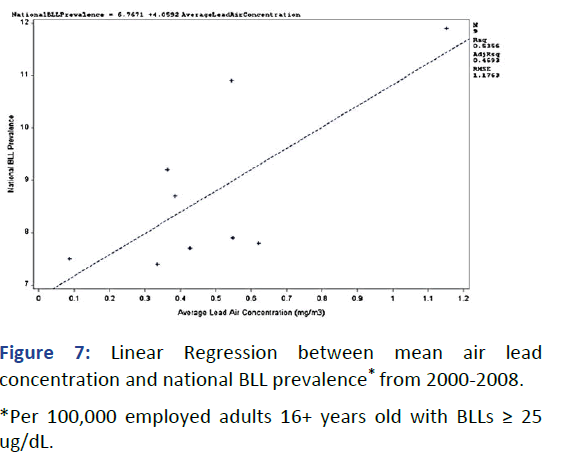
The linear regression plot comparing national high BLL
prevalence (y-axis) and national average air concentration (xaxis,
listed at mg/m3) can be seen in Figure 7. Every
1.0 mg/m3 increase in lead air concentration corresponded
to an estimated four additional cases per 100,000 employed
adults with BLLs ≥ 25 ug/dL. The model has a moderate R2 of
0.536, advising caution if to be used for predictive purposes.
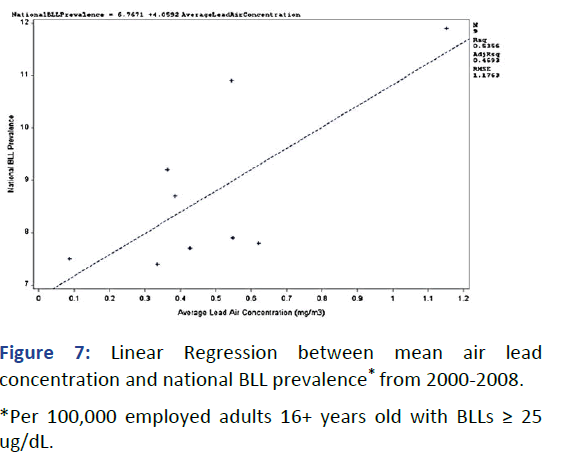
Figure 7: Linear Regression between mean air lead
concentration and national BLL prevalence* from 2000-2008.
*Per 100,000 employed adults 16+ years old with BLLs ≥ 25
ug/dL.
Discussion
We hypothesized that:
• There was a statistically significant decrease in the
prevalence of high BLL between the years 2000 and 2009
for workers in the state of Utah and the U.S. as a whole.
• This decrease coincides with a decline in reported lead air
concentration levels.
Our methodology and findings align with previous work on a
lead exposure database built from a retrospective collection
of 1,111 datasets from 175 published papers (lead data from
area samples, personal measurements, and blood
biomonitoring). Like this study, we compared national BLL and
national air lead concentration to estimate trends over time
and found that high BLL prevalence generally declined each
year. Our study expands the knowledge base by comparing
each data set from 2000-2009 to determine alignment to the
2010 healthy people goals.
Although Utah and the nation failed to meet the healthy
people 2010 objective to reduce the number of employees
occupationally exposed to lead with BLLs ≥ 25 μg/dL to 0 μg/
dL, the U.S. did see a statistically significant overall decline in
elevated BLL prevalence over the time frame. This decline is
likely due to many different government regulations, including
limits on lead within drinking water; banning of many lead
containing objects, and institution of BLL surveillance
programs. This decline also indicates that the healthy people
2010’s goal was perhaps overly optimistic, especially given
healthy people’s 2020 occupational lead objective is much
more modest, aiming to reduce by 10% the number of adult
workers 16+ years older with BLLs ≥ 10 ug/dL. Similarly, while
Utah failed to reach the healthy people 2010 goal, our findings
indicate that Utah’s high BLL prevalence decline was
statistically significant. A larger dataset (i.e., more years of
data) may increase that significance even more. However, the
model comparing Utah and the U.S. prevalence was much
weaker, suggesting that the nation’s BLL prevalence is a poor
predictor of Utah’s BLL prevalence. However, standardized
state level guidelines from the Utah Lead coalition may soon
bring Utah into line with national expectations and trends. Air
monitoring remains the primary method to effectively predict
extreme BLLs without biomonitoring. Every 1.0 mg/m3 increase in lead air concentration corresponded to four
additional cases per 100,000 employed adults with BLLs ≥ 5
ug/dL. However, caution should be employed when using this
model for prediction, given the R2 value of 0.54.
Several limitations may affect the generalizability of these
results, including numerous types of bias from each of the
collected datasets arising from the collection, storage,
analysis, and reporting of samples. While the extent of this
bias is unknown, the collection and analysis of blood lead and
airborne lead are relatively simple and common procedures
with written guidance. Data for the average lead air
concentration could also be biased due to the various
sampling methodologies. To avoid bias, most samples are
collected on a random basis; however, the CEHD was collected
by OSHA inspectors. These inspectors may perform random
sampling when selecting which companies to investigate, but
the OSHA officers are primarily concerned with compliance
testing and compliant response. This sampling purpose
involves selecting companies with worst case scenarios, which
means the average air lead concentration may be biased towards an overestimate o f t he national me an exposure
concentration.
The small sample size is another potential limitation. Only ten
samples were extracted from the BLL prevalence datasets,
one average for all the years between 2000-2009. While CEHD
contains numerous data points, these were condensed into
ten average air lead measurements for comparison to the
other datasets. This limited number of samples reduced our
statistical power; nonetheless, we observed a statistical
decline between the two BLL prevalence datasets. The
national BLL prevalence that has been referred to throughout
this study is also not necessarily representative of the entire
nation. Only about 25 states participated in ABLES at the start
of 2000, and not all states that joined since 2000 have sent
data every year. That being said, ABLES data continues to be
the best source of BLL prevalence for the nation as most
states send their BLL results to this database. Finally, although
the primary lead exposure in this study is believed to be
occupational, the measured BLL could also be from nonoccupational
sources such as gun use, recreational activities,
residential lead paint, and environmental lead.
Future studies should consider focusing on socially
and economically disadvantaged populations, as these
groups are more likely to live in houses that used lead paint,
live closer to lead emitting facilities and may not have
received adequate information on lead containment.
Several studies have advocated for identifying and
tracking BLL throughout multiple high risk populations
and educating them on the physical and mental harm,
health assessments, and treatments. Vulnerable
occupational populations, like refugees or immigrants,
may be particularly at risk. Future studies can expand upon
this knowledge and continue to look at various agents over
different periods, such as past or current healthy people
initiatives, different states, different agencies, and different
databases and techniques.
Conclusion
Lead is a serious health concern that primarily affects
occupational workers. By monitoring air lead concentration,
and blood lead levels, employees can be alerted before
chronic damage takes place. Using multiple datasets, we
predicted that from 2000-2009 Utah and U.S. prevalence of
individuals with ≥ 25 ug/dL BLL would decrease along with
national air lead concentration to align with goals of healthy
people 2010. Although Utah’s and the nation’s BLL high
prevalence failed to reach desired levels, there was an overall
prevalence decrease throughout the studied decade. Utah’s
prevalence levels were significantly lower than national ones
but fell into patterns of peaks and declines. Air lead
concentrations have mostly decreased as well, though all
years were still found to be above the OEL. Every 1.0 mg/m3 increase in lead air concentration corresponded to an
estimated four additional cases per 100,000 employed adults
with BLLs above 25 ug/dL. This alarming discovery is essential
for future occupational health research and requires further
investigation.
References
- Levin R, Vieira CLZ, Rosenbaum MH, Bischoff K, Mordarski DC, et al. (2021) The urban Lead (Pb) burden in humans, animals and the natural environment. Environ Res. 193:110377.
[Crossref] [Google Scholar] [PubMed]
- Koh DH, Locke SJ, Chen YC, Purdue MP, Friesen MC (2015) Lead exposure in US worksites: A literature review and development of an occupational lead exposure database from the published literature. Am J Ind Med. 58(6):605-616.
[Crossref] [Google Scholar] [PubMed]
- Dignam T, Kaufmann RB, LeStourgeon L, Brown MJ. Control of Lead sources in the United States, 1970-2017: Public health progress and current challenges to eliminating lead exposure. J Public Health Manag Pract. 2019;25(1):S13-S22.
[Crossref] [Google Scholar] [PubMed]
- Levin R. The attributable annual health costs of U.S. occupational lead poisoning. Int J Occup Environ Health. 2016;22(2):107-120.
[Crossref] [Google Scholar] [PubMed]
- Lanphear BP, Rauch S, Auinger P, Allen RW, Hornung RW. Low level lead exposure and mortality in US adults: A population based cohort study. Lancet Public Health. 2018;3(4):177-184.
[Crossref] [Google Scholar] [PubMed]
- Schober SE, Mirel LB, Graubard BI, Brody DJ, Flegal KM (2006) Blood lead levels and death from all causes, cardiovascular disease, and cancer: Results from the NHANES III mortality study. Environ Health Perspect. 114(10):1538-1541.
[Crossref] [Google Scholar] [PubMed]
- Koh DH, Locke SJ, Chen YC, Purdue MP, Friesen MC (2015) Lead exposure in US worksites: A literature review and development of an occupational lead exposure database from the published literature. Am J Ind Med. 58(6):605-616.
[Crossref] [Google Scholar] [PubMed]
- Walter A, Alarcon M (2015) Elevated blood lead levels among employed adults united states, 1994–2013. MMWR Morb Mortal Wkly Rep. 63(55):59-65.
[Crossref] [Google Scholar] [PubMed]
- Tong S, von Schirnding YE, Prapamontol T (2000) Environmental lead exposure: A public health problem of global dimensions. Bull World Health Organ. 78(9):1068-1077.
[Google Scholar]
- Tsirlin A, Oo Y, Sharma R, Kansara A, Gliwa A, et al. (2014) Pheochromocytoma: A review. Maturitas. 77(3):229-238.
[Crossref] [Google Scholar] [PubMed]
- Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, et al. (2007) Pheochromocytoma: Recommendations for clinical practice from the first international symposium. Nat Clin Pract Endocrinol Metab. 3(2):92-102.
[Crossref] [Google Scholar] [PubMed]
- Davutoglu V, Soydinc S, Celkan A, Kucukdurmaz Z (2004) Left ventricular free floating ball thrombus complicating aortic valve stenosis. J Heart Valve Dis. 13(2):197-199.
[Google Scholar] [PubMed]
- Adler JT, Meyer-Rochow GY, Chen H, Benn DE, Robinson BG, et al. (2008) Pheochromocytoma: Current approaches and future directions. Oncologist. 13(7):779-793.
[Crossref] [Google Scholar] [PubMed]
- Vinnakota S, Jentzer JC, Luis SA (2021) Thrombolysis for COVID-19 associated bioprosthetic mitral valve thrombosis with shock. Eur Heart J. 42(39):4093-4093.
[Crossref] [Google Scholar] [PubMed]
- Steinsapir J, Carr AA, Prisant LM, Bransome ED (1997) Metyrosine and pheochromocytoma. Arch Intern Med. 157(8):901-906.
[Google Scholar] [PubMed]
- Walther MM, Keiser HR, Linehan WM (1999) Pheochromocytoma: Evaluation, diagnosis, and treatment. World J Urol. 17:35-39.
[Crossref] [Google Scholar] [PubMed]
- Bryant J, Farmer J, Kessler LJ, Townsend RR, Nathanson KL (2003) Pheochromocytoma: The expanding genetic differential diagnosis. J Natl Cancer Ins. 95(16):1196-1204.
[Crossref] [Google Scholar] [PubMed]
Citation: Handy R, Kuhre J, Sleeth D, Schaeffer C (2023) A Comparison of Occupational Blood Lead Level (BLL) Prevalence and
Airborne Lead Concentration in Utah and Nationally. J Heavy Met Toxicity Dis. 8: 12.
Copyright: © 2023 Kuhre J, et al. This is an open-access article distributed under the terms of the Creative Commons
Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original
author and source are credited.