Research Paper - (2010) Volume 18, Issue 4
Public Health Specialty Registrar, NHS Nottinghamshire County, UK
Objectives To consider the recent evidence which examines factors that are associated with uptake of cervical and breast screening in the British South Asian community and to consider the effectiveness of interventions to improve uptake in this group. MethodsA search strategy was developed and key databases were searched to identify primary research studies that examined the uptake of cervical and breast screening in British women of South Asian origin. Studies published prior to 1996 were excluded from the review. ResultsSeventy-eight studies were identified and ten were included in the review. Observational studies demonstrated mixed results on the effect of ethnicity on uptake of screening. Controlling for confounders attenuated the effect in all studies and removed its effect entirely in some. Investigation of low uptake in qualitative and quantitative research indicates that South Asian women were more likely to have incorrect addresses and language or cultural barriers to screening than other women. Few interventional studies were identified and all varied in their design. The success of interventions was mixed and the lack of control groups in some studies made it difficult to draw conclusions on their effectiveness. ConclusionThere is a poor uptake of cervical and breast screening by South Asian women compared with the general population in Britain. Evidence is inconclusive as to whether this is due to a residual effect of ethnicity following control for socio-demographic and local health service variables. Currently there is a lack of robust experimental studies on which to base interventions intended to increase uptake in this population.
breast screening, cancer, cervical screening, review, South Asian
How this fits in with quality in primary care
What do we know?
Uptake of cervical and breast screening is lower in South Asian women than in the rest of the population.
What does this paper add?
The uptake of screening is dependent on a large number of factors but the independent effect of ethnicity remains unclear. The influence of socio-demographic and practice factors on screening uptake varies across populations. There is a lack of evidence to support interventions to increase the uptake of screening in this population.
The UK National Screening Programmes for cervical and breast cancer are now well established following their introduction in 1988. Women aged 50–64 are invited for breast screening once every three years and those aged 25–64 are invited for cervical screening every three or five years depending on their age.[1] Following their introduction, uptake of these programmes has gradually increased until recent years. In England, breast screening coverage (the percentage of women screened within three years) has remained static at just under 70% since 2000.[2] However, coverage of cervical screening has fallen over the last ten years and in 2007–2008 fell below 80% for the first time since the early 1990s.[3]
Screening coverage is not uniform across the population. For example, cervical screening data demonstrate that younger women are less likely to have had a cervical screen (66.2% coverage in women aged 25– 29) and coverage at a primary care trust level varies between 66.7% and 85.7%.[3] It is estimated that 7.9% of eligible women have never had a cervical screen.[3] A similar pattern exists for breast screening.[2] Other factors that have been associated with low screening coverage include economic and social deprivation4 and non-white British ethnicity.[5,6] However, as identified in a review conducted by Hoare in 1996, it is not clear to what degree these factors confound one another[7] and evidence of size of effect or causal relationship is weak. Many of these studies were published at an early stage of the National Screening Programmes and as such may not reflect the current picture;[8] the public health challenge of identifying and targeting groups with low uptake remains.[9]
The aim of this scoping review was twofold: to consider the recent evidence examining socio-demographic, healthcare and other factors that are associatedwith coverage of cervical and breast screening in the British South Asian community and to consider the effectiveness of interventions to improve uptake in this group. For the purpose of the review South Asia was defined as the countries of Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan and Sri Lanka.
Ovid MEDLINE (1996 to August week 4 2009), EMBASE (1996 to week 36 2009), the British Nursing Index (1994 to September 2009) and CAB Abstracts (1990 to week 35 2009) were searched on 7 September 2009. Database content from 1996 onwards was searched in order that the review would reflect the current picture of cancer screening. Search terms were designed to elicit studies considering the following parameters: ‘South Asian’, ‘cancer screening’ and ‘UK’ (details of the search strategy and search terms used can be found in Figure 1). Titles and abstracts of studies were reviewed by the author for inclusion according to the search strategy. Only primary research studies from the UK published after 1996 were included. The reference lists and new citations of selected studies were reviewed to identify any additional studies. No attempt was made to identify unpublished or grey literature. A total of ten studies was identified and included in the narrative review.
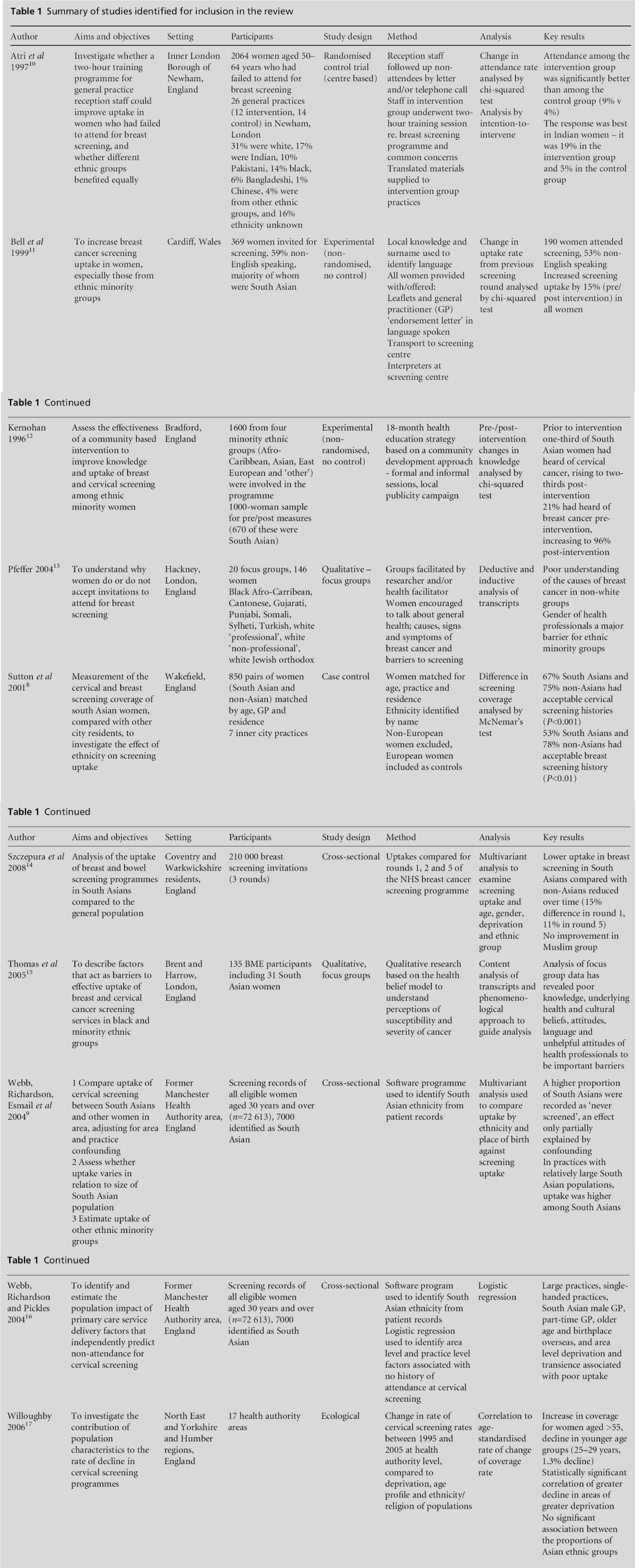
Factors that affect the uptake of screening are likely to differ between breast and cervical screening programmes, in part due to the different age groups. However, due to the scarcity of literature, for the purpose of this review breast and cervical cancer have been considered together. All studies included in the review have been summarised in Table 1.
Socio-demographic and healthcare system factors associated with cancer screening uptake
Four large-scale observational studies investigating the effect of ethnicity on screening uptake whilst controlling for other factors were identified and are discussed below.
Sutton, Storer and Rowe8 investigated the uptake of breast and cervical screening programmes by South Asian women compared with non-Asian women. Pairwise matching was used to control for the effect of age, residence and general practice. Significantly higher rates of breast and cervical screening uptake were found in non-Asians compared with South Asians (78% vs 53%, p<0.01; 75% vs 67%, p<0.001, respectively). One of the criticisms of this paper is that women’s ethnicity was determined by two researchers ‘flagging women whose names appeared to be of South Asian origin’ (p. 183). It is therefore impossible to ascertain how accurate this method was in comparison to the standard method using computer software with known sensitivity and specificity;[18] any misclassification would lessen the effect detected between groups. Questions also arise with regard to the exclusion criteria used. The authors excluded only non-European women from the control group. However, the factors that affect the uptake of screening in South Asian women may be due to migrant status and therefore may also impact upon European migrant groups, e.g. language barriers, transience, etc. Including European migrant women within the control group may have lessened the effect of ethnicity detected. Additionally, the uni-classification of all South Asian women may have masked subgroup characteristics.
Szczepura, Price and Gumber[18] considered breast screening uptake patterns in South Asian groups compared with non-Asians (n=210 000). Ethnic origin of individuals was determined using computer software validated against local name datasets and results were verified by manual checks. This approach also allowed for identification of five South Asian subgroups (Hindu–Gujarati; Hindu-other; Muslim; Sikh; South Asian other). Lower rates of screening in South Asian groups remained after controlling for age and socio-economic deprivation. Subgroup analysis showed that between 2001 and 2004 South Asian women were significantly less likely to have had breast screening compared with non-Asian women (Muslim women odds ratio (OR) 0.40, 95% confidence interval (CI) 0.35–0.46; Sikh women OR 0.79, 95% CI 0.72–0.88). One of the strengths of this study is that it included Asian subgroups in the analysis rather than assuming ethnic homogeneity. This can be highlighted by considering the different likelihood of screening compared to non-Asian women across these groups.
By contrast, other studies published around the same time did not identify an effect of ethnicity after controlling for confounding variables.Webb, Richardson, Esmail et al[9] considered cervical screening uptake by ethnicity and place of birth in 72 000 women. They found that the lower screening uptake in South Asian women (69.5% vs 73% ‘others’, p<0.001) was explained by area and practice-level variables. Practices with small South Asian populations were found to be associated with lower rates of screening uptake. The authors used computer software to identify the ethnic origin of women from women’s names and then enhanced this by using place of birth information. However, the authors did not use these data to stratify women according to their immigration status, i.e. those of South Asian ethnicity born in the UK and those born in South Asian countries, instead analysing all ‘South Asian’ women as one group.
The advantage of verifying the computer identified ethnicity is the opportunity to identify subgroups. However, these subgroups were not identified and information on place of birth was only available for one third of women.
Willoughby, Faulkner, Stamp et al1[7] conducted an ecological study to consider factors that may have contributed to the decline in screening rates between 1995 and 2005. No correlation was found between declining rates of cervical screening and the size of the South Asian population (r2=0, p=0.56). This study does little to increase the understanding of the impact of ethnicity on rates of screening; population level screening rates may not be sensitive enough to detect changes within a relatively small proportion of the population. Considering rates of screening within different ethnic groups is likely to be a more effective way of identifying whether ethnicity contributes to this rate decline. Additionally, the authors considered a static measure of ethnicity, making an assumption that these measures did not change over time. A more informative approach would have been to compare the year-on-year changes in the ethnic profile of the populations against the screening rate.
Potential mechanisms for poor uptake
Three studies were identified that investigated potential mechanisms for poor uptake; these are discussed below. Two of these studies were qualitative and one cross-sectional in design.
A study by Webb, Richardson and Pickles16 considered the effect of primary care and individual factors on cervical screening uptake. The strongest predictor of no uptake was an overseas birth place (adjusted OR 3.75; 95% CI 3.26–4.32). This finding at a population level does little to suggest possible causative factors, which may include transience, language and health service knowledge barriers. Other smaller intervention studies can help to explain low uptake in those with overseas places of birth; some have found that many South Asian women, born outside but living in the UK, often return to their place of birth either permanently or for extended periods.10–12 Recent estimations of the proportion of incorrect addresses for South Asian non-attendees are between 21% and 25%[11,12] and between 8% and 15% of women have been out of the country at the time of invitation.[10,12] This highlights the need for accurate patient registers to ensure that women receive their invitations for screening.
Findings from qualitative studies give useful insight into the barriers to screening that South Asian women experience. Pfeffer[13] used focus groups to explore women’s perception of their risk of breast cancer and their reasons for compliance with screening. The groups were encouraged to talk about their health, and understanding of breast cancer and screening. Groups varied in their composition; some were naturally occurring whereas others were constructed for the purpose of the research; this appeared to impact on the depth and type of information gathered from each group. Understanding of breast cancer risk and women’s perceptions of their own risk were found to be characterised by ethnicity and culture. The South Asian groups reported that their risk of breast cancer was low as they did not smoke or drink and breastfed their children. These groups also reported a reluctance to take up the screening invitation due to cultural issues such as being examined by a male healthcare professional and exposing their breasts. The themes emerging from this research not only offer potential explanations for the poor uptake in South Asian (and other ethnic minority) groups but also identify opportunities to intervene. However, as the authors commented, these may be common themes for all women who do not access breast screening and hence require testing within other population groups.
Thomas, Saleem and Abraham[15] used focus groups to explore knowledge of cancer, and access and barriers to screening in minority ethnic groups. Key barriers for all the groups, but particularly South Asian women, included the lack of culturally and religiously sensitive services. Language was the most commonly cited barrier to accessing screening in Muslim and Gujarati communities. This included a lack of translated materials, inaccurate translations and low literacy levels. The number of South Asian women in this study was relatively small and relied on volunteer recruitment from local groups, so is unlikely to be representative of all South Asian women.
Interventions to increase cancer screening uptake
Although the rate of breast and cervical screening in South Asian populations is low there is a dearth of interventional studies that consider approaches to improving uptake. Just three studies were identified, of which only one was of a randomised controlled design. All three studies are discussed below.
Bell, Branston, Newcombe et al[11] investigated the effect of a mix of interventions to increase the uptake of screening in women registered with three inner city general practices. Women were provided with information in a language they were able to understand, free transport to and from the practice and the support of a link worker at their appointment. Uptake of screening improved across the three practices from 35% to 51% (45% in the non-English speaking group). The authors concluded that the provision of translated literature and link workers appeared to be effective interventions in terms of increasing the uptake of screening in this cohort. However, these conclusions seem to have little supportive empirical or statistical evidence and without a control group it is not possible to directly attribute the findings to the interventions.
Kernohan[12] conducted a community development programme to improve knowledge of breast and cervical cancer and screening in ethnic minority women. The use of a community development approach fits with evidence that found that general practiceswith a larger South Asian population had better uptake of screening, assumed to be a result of community empowerment and social norms.[16] South Asian women were found to have the lowest levels of knowledge at baseline and showed the greatest improvement (heard of mammography pre-programme 21%; post-programme57%; p<0.05). Self-reported uptake of screening also increased (breast cancer screening – threefold increase; cervical cancer screening – 30% increase, no p value given). This study is interesting as it highlights women’s low level of knowledge at baseline of both screening services and cancer. This finding is even more noteworthy considering that the study relied upon a convenience sample of women already involved in a health promotion programme, so their awareness may well have been an overestimation of that of the wider population.
Atri, Falshaw, Gregg et al[10] undertook a randomised controlled trial to investigate whether a short training session for reception staff improved the uptake of breast screening for women who had previously not attended. Reception staff in the intervention group underwent a two-hour training session informing them about the screening programme and women’s fears. The reception staff in the control group did not receive this training. Reception staff in both groups were asked to contact women who had not responded to an invitation to attend mammography by letter and/or telephone call. A 5% increase in attendance of initial non-attendees in the intervention group compared to the control group was demonstrated, with a 4%increase in attendance in the control group froma baseline attendance of 49% and a 9% increase in the intervention group from a baseline attendance of 48%. No clinical or statistical significance of this absolute increase in attendance is given despite the relative increase in attendance (OR 2.3, 95% CI 1.1–5.3, p=0.04). Indian women in the intervention group were more likely to subsequently attend screening compared to controls (OR 2.2, 95% CI 1.3– 3.8); other ethnic groups, including Pakistani and Bangladeshi, did not demonstrate such a significant increase. The authors suggest that the significant results seen in the Indian women may be due to many of the reception staff being fluent in several commonly spoken languages. This highlights the fact that interventions must meet local needs in order to maximise their effect.
Role of ethnicity
All of the studies reviewed demonstrated lower screening uptake in South Asian women than non- South Asian populations. The studies reveal discrepancies in the effect of ethnicity, following adjustment for potential confounders, on the uptake of breast and cervical screening. Two studies demonstrated that ethnicity did have an effect8,18 whereas two of the studies indicated that ethnicity had no effect.[9,17] The lack of agreement may be due to a number of factors: different study designs, the variation in methods used to identify the ethnicity of women, the range of variables considered and the heterogeneity of control groups.
The uptake of screening in South Asian women varied across different areas and studies. Part of this effect may be explained by factors including the absolute and relative sizes of South Asian communities [16] and how established these communities are. New British South Asian communities may have a larger proportion of women who have been born outside the UK,[16] poorer English language skills or social norms that reduce access to services.[12] Established communities may be larger and include a greater proportion of English speaking women. Additionally, recent immigrant communities are likely to differ in their composition from those established communities whomostly immigrated to the UKseeking labour after the Second World War. There was no attempt in any of the studies to stratify women according to whether they had been born in the UK or were first generation immigrants. The degree to which ethnicity and other variables affect screening uptake is likely to differ in these different populations due to a range of factors, including English language skills and cultural barriers.
Studies that attempt to explain the mechanisms that determine screening uptake in South Asian women identify key factors including perceived risk, cultural or language barriers and the transient population.[11–13,19] The relative influence of these factors on the uptake of screening in comparison to socio-demographic factors has not been investigated; such studies would assist in identifying potential areas for intervention. Poor English language skills, particularly reading skills, are important barriers to accessing healthcare in ethnic minority adults;[20] these are likely to be of particular importance in screening services that rely on automated, paper-based call and recall systems.
Reviewing the range of study populations, methodologies and findings of these studies highlights the variations in screening uptake, factors associated with uptake and barriers across South Asian populations. This emphasises the importance of considering the heterogeneity of these groups rather than assuming homogeneity.[13,18,21]
Effectiveness of interventions
There are few studies that have investigated the effect of interventions to increase the uptake of screening and those that have been done have shown mixed results. This is likely to be due in part to lack of statistical power, lack of control groups or randomisation and the lack of differentiation of the populations studied. These factors perhaps reflect the challenges in conducting robust experimental studies in general healthcare settings. Despite well-intentioned and targeted interventions three of the studies demonstrated an increase in uptake across all ethnic groups, suggesting that the effect of the interventions may have been due to the contact with women rather than the content per se.[10–12] The lack of robust evidence from these studies does not mean they should be dismissed but highlights the need for well-designed studies to evaluate the clinical and cost-effectiveness of targeted interventions in increasing screening uptake in South Asian women.
Study limitations
This scoping narrative review was not intended to be a comprehensive and systematic review of the literature and so is limited in its findings, particularly as it was restricted to the UK. The titles, abstracts and included papers were reviewed by the single author, potentially reducing the reliability of the study. Additionally, no grey or unpublished literature was included; given the role of publication bias and the lack of conclusive evidence in the published studies this may have been an important limitation as many ‘non-significant’ studies may not have been published and thus excluded. and studies. This emphasises the need for local needs assessment work to identify the size and constitution of the community and barriers to screening in this group, to ensure evidenced best practice is effectively implemented.
A common limitation of all these studies was the difficulty of identifying women of South Asian origin and establishing measures of need such as preferred language. General practices should be encouraged to improve their recording of patients’ ethnic origin and key details such as preferred language. Such information would enable practices to highlight women’s specific needs on receipt of prior notification lists and to ensure that women receive information in a form that is appropriate to their needs.
These studies also highlight the crucial element of individual and community support for women who fail to attend for screening even though this effect may not be exclusive to South Asian women. Local screening programmes and general practices should consider how existing resources such as multilingual workers and health trainers can be utilised to support women in overcoming their barriers to screening.
There is a poor uptake of cervical and breast screening by South Asian women compared to the general population. However, it remains unclear to what degree the disproportionate representation of South Asian women in deprived, inner city, isolated communities affects uptake; how other variables that are known to negatively affect screening uptake and that are more common in South Asian groups (e.g. incorrect addresses, transient population, language and cultural barriers and poor awareness of screening programmes) influence uptake; and the residual effect of ethnicity.
The few studies that have investigated the effect of interventions to increase the uptake of screening have shown mixed results. However, they all highlight the need to tailor interventions to the local population. The lack of studies and the heterogeneity of their design and of the populations studied suggest that the possibility of a large, robust, systematic review being conducted may be some time off.
Epidemiologists and front-line health professionals alike need to continue the determined efforts to increase screening coverage in this group.
I would like to acknowledge the support of Dr Sarah Rodgers, Research and Evaluation Team, NHS Nottinghamshire County and Dr Heather Roberts, Course Leader, Masters in Public Health, University of Nottingham.
This review was initially conducted as part of my Masters degree in public health.
None.
Ethical approval was not required for this review.
Not commissioned; externally peer reviewed.
None.