- (2015) Volume 16, Issue 3
David X Jin1, Aaron J Small1, Charles M Vollmer2, Nirag Jhala3, Emma E Furth3, Gregory G Ginsberg1, Michael L Kochman1, Nuzhat A Ahmad1, Vinay Chandrasekhara1
Departments of 1Internal Medicine, 2Surgery and 3Pathology and Laboratory Medicine, Hospital of the University of Pennsylvania, Philadelphia, Pennsylvania
Received February 19th, 2015 – Accepted March 28th, 2015
Context Carcinoembryonic antigen analysis of pancreatic cyst fluid is the tumor marker of choice for preoperatively differentiating mucinous from non-mucinous cystic lesions. Objective We aim to determine the most accurate cyst carcinoembryonic antigen cut-off value for distinguishing mucinous cysts from non-mucinous cysts with a focus on discriminating intraductal papillary mucinous neoplasms. Methods The results of pancreatic cyst aspiration carcinoembryonic antigen levels from a single center were retrospectively collected and evaluated for a diagnosis of a mucinous cyst and an assessment of malignancy using surgical histology as the diagnostic standard in 86 patients. Results The median cyst carcinoembryonic antigen level (ng/mL) was significantly higher in mucinous cysts compared with non-mucinous cysts (218 vs 4.4; P=0.0006) and in intraductal papillary mucinous neoplasms compared with non-mucinous cysts (135 vs 4.4; P=0.0027). A cyst carcinoembryonic antigen cut-off of 30.7 ng/mL was most accurate (87.2%) for differentiating mucinous from non-mucinous cysts and specifically for differentiating intraductal papillary mucinous neoplasms from non-mucinous cysts (82.7%). Cyst carcinoembryonic antigen levels were not significantly different between malignant and non-malignant mucinous cysts (68.5 vs 238.1; P=0.51). Conclusions Pancreatic cyst fluid carcinoembryonic antigen can accurately differentiate histologically verified mucinous lesions, including intraductal papillary mucinous neoplasms, from non-mucinous lesions with an optimal cut-off that is much lower than previously reported values. Cyst carcinoembryonic antigen levels are not a reliable predictor of malignancy.
Carcinoembryonic Antigen; Pancreatic Cyst
CEA carcinoembryonic antigen EUS endoscopic ultrasound FNA fine needle aspiration HUP Hospital of the University of Pennsylvania IPMN intraductal papillary mucinous neoplasm MCN mucinous cystic neoplasm SCA serous cystadenoma
A greater number of incidental pancreatic cystic lesions are being diagnosed due to increased usage of abdominal imaging [1]. These lesions are found in 1% to 2.6% of asymptomatic adults, with prevalence increasing with age [2, 3]. With growing experience and a better understanding of their natural history, it has become clear that these cystic lesions encompass a broad spectrum of benign, borderline, and malignant tumors [4]. As such, differentiating among them and accurately predicting those at highest risk of malignancy has a profound impact on management.
Mucinous cysts, comprised of mucinous cystic neoplasms (MCNs) and intraductal papillary mucinous neoplasms (IPMNs), are considered neoplastic lesions associated with an increased risk of pancreatic adenocarcinoma [5]. IPMNs arise from pancreatic ducts and are classified into main duct (MD-IPMN), branch duct (BD-IPMN), or mixed type [6]. MCNs characteristically lack communication with the pancreatic ductal system and are histologically differentiated from IPMNs by the presence of ovariantype stroma. As such, they occur almost exclusively in premenopausal women [5, 7, 8].
Series have shown that the prevalence of malignancy, defined as high-grade dysplasia or invasive carcinoma, varies from 36%-100% in MD-IPMNs to 6%-47% in BD-IPMNs [9-13]. The rates are lower in MCNs (11- 39%) but greater than 10% have invasive carcinoma on surgical histology [8, 14]. Considering the risk of malignant degeneration and high likelihood of cure with early detection and operative resection, all mucinous cystic lesions require risk stratification to determine which would benefit from surgical intervention versus continued surveillance imaging based on patient and cyst characteristics [15]. Furthermore, it is critical to differentiate mucinous cystic lesions from non-neoplastic pancreatic cysts prior to committing an individual to surgery or long-term surveillance.
With increased use of endoscopic ultrasound (EUS) and fine-needle aspiration (FNA), carcinoembryonic antigen (CEA) analysis of pancreatic cyst fluid has emerged as the test of choice for distinguishing mucinous from nonmucinous cysts, owing to its superior accuracy when compared to cytology, other tumor markers, or molecular analysis [16-26]. While it has been shown that mucinous lesions contain elevated cyst CEA levels compared to their non-mucinous counterparts, various centers have reported a wide range of diagnostic cut-off values (30 ng/ mL to 800 ng/mL), with few studies evaluating the optimal cyst CEA level for specifically diagnosing IPMNs [23-26].
Using surgical pathology as the gold-standard, we report the performance characteristics of CEA levels from EUSguided aspiration of pancreatic cyst fluid to determine the optimal cut-off value for predicting mucinous neoplasia, with particular focus on IPMNs. In addition, we investigate if cyst CEA levels can predict malignancy in mucinous cystic lesions of the pancreas.
Patients
Between January 2000 and June 2012, 394 patients underwent operative resection of a pancreatic cystic lesion at our tertiary care center, of which 221 received a pre-operative EUS. Of these, 86 patients had cyst fluid sampled for CEA analysis and were included in our study. Patient demographics, EUS findings, cross sectional imaging results, cyst fluid analysis, and surgical histology were retrospectively evaluated. The study was approved by the institutional review board of the University of Pennsylvania.
Endoscopic Ultrasound Technique
All patients underwent EUS examination with a curvilinear array endoscope. The examination provided high resolution imaging of the pancreas and information on cyst size, location, and characteristics. Cystic lesions were aspirated until decompression if possible using one passage of a 22-gauge needle (Cook Medical, EUS-3N, Bloomington, IN) under EUS guidance. Fluid was sent for biochemical and cytological analysis. In our practice, cyst aspirates were sent for CEA analysis in a serum separator tube (BD Vacutainer, Franklin Lakes, NJ) if more than 1 mL could be collected. Otherwise, fluid was only sent for cytopathology. In cases with multiple cystic lesions, the largest cyst was aspirated.
Biochemical Markers
Cyst fluid concentrations of CEA (measured in nanograms per milliliter) were determined using the sandwich electrochemiluminescence (ECL) method on a Roche Elecsys System (Indianapolis, IN). Samples were run without dilution unless cyst CEA levels resulted greater than 1000 ng/mL. A universal diluent (Roche Diagnostics, Indianapolis, IN) was used in these cases with a maximum dilution of x100 (100,000 ng/mL). For the purposes of this study, cyst fluid viscosity, amylase, or other tumor markers were not analyzed.
Cytology
Cytological analysis of cyst fluid samples was performed by specialized GI cytopathologists at the Hospital of the University of Pennsylvania (HUP). Samples were prepared using liquid-based preparations stained with routine Papanicolaou or hematoxylin and eosin stains. Each sample was analyzed for evidence of a mucinous cystic lesion and the presence of cytological high-grade dysplasia or carcinoma.
Histology
Primary histological interpretation of the resected specimens was performed by specialized GI pathologists at HUP. The cysts were classified as (1) mucinous cystic lesions (MCN or IPMN) or (2) non-mucinous cystic lesions (all others). All mucinous lesions were re-evaluated for the presence of mesenchymal ovarian-like stroma, which is a requisite feature for classification as MCN [5]. Degrees of dysplasia in mucinous lesions were categorized according to WHO classification [27]. Those exhibiting adenocarcinoma with or without invasion were classified as malignant. The remaining were classified as nonmalignant mucinous lesions.
Analyses were restricted to patients with histological confirmation of cyst type. Results were expressed as means with standard deviation if data were normally distributed. Otherwise, results were expressed as medians with interquartile range. The Wilcoxon rank-sum test and two sample t-test were used to compare the differences between two groups of a priori interest for non-parametric data and parametric data, respectively. The two sample test of proportions was used when comparing rates or proportions for statistical differences between two groups. A two-sided P<0.05 was considered statistically significant.
Receiver operator characteristic (ROC) curves using cyst CEA values were plotted to predict (1) a mucinous from a non-mucinous cyst and (2) an IPMN from a nonmucinous cyst. The area under each ROC curve (AUC) was calculated. A cyst CEA cut-off was selected to maximize the AUC, thereby maximizing the proportion of correct cyst classifications. Sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), and accuracy rates were determined using this value. Performance characteristics using previously reported cyst CEA cut-offs (192, 300, 800 ng/mL) were calculated for comparison [23, 24, 26]. Data analysis was performed using STATA version 12.1 (Stata Corp, College Station, TX).
Patients
A total of 86 patients (32 male, 54 female) were included in this study. The mean age at time of surgical resection for all cysts was 65.0 ± 13.0 years. There was no significant difference in age or gender between those with mucinous cysts and those with non-mucinous cysts. As has been previously described, MCNs preferentially affected female patients (84.0% vs 53.9%; P=0.010) and younger patients (56.5 ± 15.3 vs 70.0±8.6 yrs; P=0.0001) when compared to IPMNs [8]. Patient demographics are shown in Table 1.

Cyst Characteristics
Histological examination revealed a final diagnosis of 77 mucinous cystic lesions (52 IPMN, 25 MCN) and 9 non-mucinous cystic lesions. Of the 52 IPMNs, 12 met histologic criteria for MD-IPMN (main pancreatic duct communication and dilation >5mm). The other 40 were classified as BD-IPMNs. Of the non-mucinous cysts, four were SCAs, two were cystic neuroendocrine neoplasms, two were pseudocysts, and one was an acinar cystadenoma.
Of the 77 mucinous cysts, 64 were histologically nonmalignant while the remaining 13 were categorized as malignant (6 with invasive adenocarcinoma, 7 displaying adenocarcinoma without invasion). When examining mucinous subtypes, IPMNs and MCNs had similar rates of malignancy (19.2% vs 12.0%; P=0.43). Our study also corroborated that MD-IPMNs had higher rates of malignancy than BD-IPMNs (41.7% vs 12.5%; P=0.025).
There was no difference in cyst location when comparing mucinous vs non-mucinous or malignant vs non-malignant mucinous cysts. As has been previously described, MCNs were found more frequently in the body/tail of the pancreas when compared to IPMNs (88.0 vs 48.1%; P=0.0008) [8, 14]. There was no difference in cyst size when comparing mucinous vs non-mucinous, MCN vs IPMN, MD-IPMN vs BD-IPMN, or malignant vs non-malignant mucinous cysts. Cyst characteristics are shown in Table 1.
Carcinoembryonic Antigen Level
The median cyst CEA level (ng/mL) for mucinous cysts was significantly higher than that for non-mucinous cysts (218, interquartile range 60.8-991 vs 4.4, IQR 1.0-28.6; P=0.0006). The median cyst CEA level for IPMNs was similarly higher than that for non-mucinous cysts (135, IQR 50.6-860; P=0.0016). Cyst CEA levels did not differ significantly between MCNs vs IPMNs, MD-IPMNs vs BDIPMNs, malignant vs non-malignant mucinous cysts, or malignant vs non-malignant IPMNs. Table 2 summarizes and Figure 1 illustrates the distribution of cyst CEA levels based on cyst type.

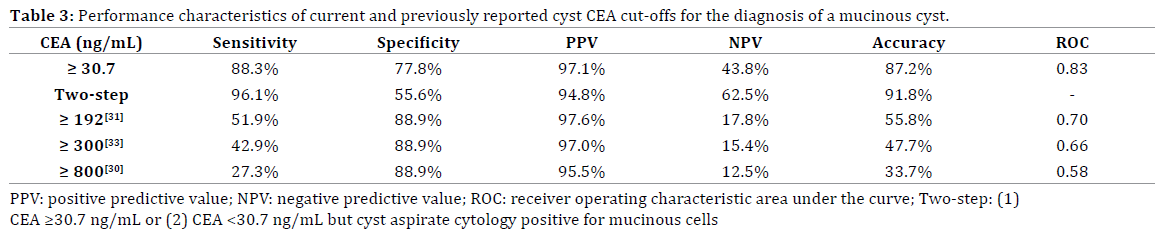
ROC analysis demonstrated that a cyst CEA cut-off of 30.7 ng/mL yielded the greatest accuracy for differentiating mucinous from non-mucinous cysts (Se 88.3%, Sp 77.8%, PPV 97.1%, NPV 43.8%, accuracy 87.2%, AUC 0.83, Figure 2) and specifically IPMNs from non-mucinous cysts (Se 83.7%, Sp 77.8%, PPV 94.7%, NPV 50.0%, accuracy 82.7%, AUC 0.82). Previously reported higher cyst CEA cut-offs were less accurate at discriminating mucinous from nonmucinous cysts (Table 3).
Cytology
Of the 86 patients included in our study, 84 had cyst fluid cytology sent during pre-operative EUS-FNA evaluation. Sensitivity, specificity, PPV, NPV, and accuracy of cyst mucinous cytology as a predictor of mucinous cyst were 57.9%, 75.0%, 95.7%, 15.8%, and 59.5%, respectively. Of the 77 patients with a histologically proven mucinous cyst, 76 had cyst fluid cytology evaluated for malignancy during pre-operative evaluation. The proportion of cysts with cytology positive for malignancy did not differ significantly between malignant and non-malignant mucinous cysts (23.1% vs 7.9%; P=0.11). In general, the presence of malignancy on cytological analysis of cysts aspirates was a poor predictor of malignancy on surgical histology (Se 23.1%, Sp 92.1%, PPV 37.5%, NPV 85.3%, accuracy 80.3%).
The increased discovery rate of pancreatic cystic lesions this past decade has been associated with a concurrent rise in the use of cross sectional imaging [1]. Most are incidentally identified in asymptomatic patients making subsequent management decisions challenging [28, 29].
These lesions can be broadly grouped into non-neoplastic and neoplastic types. Because of their varied malignant potential, neoplastic cysts should be further differentiated into mucinous and non-mucinous subtypes. This distinction has profound implications on management and surveillance. In our study, 17% of patients with mucinous cystic lesions were also noted to have malignancy on histological analysis. The prevalence of malignancy increased when examining a subgroup of IPMNs (19%) and particularly MD-IPMNs (42%). Other investigators have reported similar prevalence rates [9, 30-32]. In contrast, there was no histological evidence of adenocarcinoma with or without invasion in any of the non-mucinous cysts in our study, owing to the extremely low potential for malignancy in serous cystadenomas and relatively low grades of dysplasia in cystic neuroendocrine neoplasms [33, 34].
The diagnosis of pancreatic cysts involves the use of cross sectional imaging, EUS characteristics, and cyst fluid analysis. While computed tomography (CT) and magnetic resonance imaging (MRI) are excellent at identifying the presence of cystic lesions and visualizing mural nodules, septations, or calcifications, they are relatively inaccurate at differentiating mucinous from non-mucinous lesions [35- 39]. EUS has been used to aid the diagnosis of pancreatic cystic lesions through direct imaging and characterization of morphologic features [40]. However, accuracy in using EUS imaging alone in diagnosing mucinous lesions is less than 50% and interobserver agreement among experienced endosonographers for diagnosing pancreatic cysts is low [25, 41].
EUS-FNA for cyst fluid analysis has become the preferred method for discriminating mucinous from non-mucinous cysts. A number of cyst fluid markers, including glycoproteins (CEA, CA 19-9, CA 125, CA 15-3, CA 72-4) secreted from the epithelial lining, extracellular mucin and fluid viscosity, enzymes (amylase, lipase), and cytology have been proposed for use in differentiating the major types of cystic lesions [16-19, 22]. Of these, cyst CEA has been shown to be the most helpful in identifying mucinous neoplasms and has been recommended [23- 26]. The reason for this may be due to differences in cyst histology. Non-mucinous cystic lesions, of which the majority are pseudocysts or serous cystadenomas, either lack the epithelial lining to produce CEA, or contain simple cuboidal epithelium that generally does not secrete CEA, respectively [42]. In contrast, mucinous cysts contain epithelial cells that secrete mucin and CEA directly into cyst fluid [43].
More recently, detailed molecular analysis of KRAS and GNAS mutations, loss of heterozygosity (LOH), and measurements of DNA amount in pancreatic cyst fluid have been shown to be useful for differentiating mucinous from non-mucinous cysts [22, 44-46]. However, there is poor agreement between cyst CEA and molecular DNA analysis for the diagnosis of mucinous cysts and multiple studies have shown cyst CEA to be the more accurate of the two [20, 21, 47]. Combining cyst CEA with molecular DNA analysis appears to improve the sensitivity, but significantly increases the cost of the procedure without significantly improving patient management decisions. Furthermore, molecular DNA analysis does not appear to differentiate or predict malignant cysts [20, 21].
Needle-based confocal laser endomicroscopy (nCLE) has been shown to differentiate serous cystadenomas from other lesions with optical imaging alone [48]. However, preliminary experience with nCLE has been associated with higher rates of adverse events than EUS-FNA [49].
Studies have determined a wide range of cyst CEA levels (14.3 to 800 ng/mL) as the “optimal” cut-off for distinguishing mucinous from non-mucinous cysts [23- 26, 50-52]. Using histological analysis as the diagnosticstandard, we determined that a cut-off of 30.7 ng/mL achieved the highest accuracy for discriminating between the two. This value is much lower than previously reported values of 110 ng/mL by Cizginer et al, 192 ng/ mL by Brugge et al, and 800 ng/mL by van der Waaij et al, but closely resembles a study by Snozek et al which found a level of 30 ng/mL to be the optical CEA cut-off in an analysis of 442 pancreatic cyst fluid patients [23-25, 53]. Using the most widely adopted CEA cut-off of 192 ng/mL in our cohort would have accurately differentiated mucinous from non-mucinous cysts only 55.8% of the time versus an 87.2% accuracy using a lower cut-off of 30.7 ng/mL. The use of a two-step diagnostic approach for mucinous cysts, defined as: (1) cyst CEA ≥30.7 ng/mL or (2) cyst CEA <30.7 but cyst aspirate cytology positive for mucinous cells, yielded similar accuracy when compared to using cyst CEA alone. The broad range of optimal cut-offs may be due to differences in analytical methods as it is difficult to ascertain the effects of using different diluents or dilution assays to measure cyst fluid aspirates. However, using the described method for CEA analysis, we found a relatively low cyst CEA cut-off increased accuracy without sacrificing specificity (Table 3). Differences in these cut-off values highlight a need to develop a standardized methodology for processing cyst fluid for CEA analysis. In lieu of such availability, each institution should validate and establish optimal cut-off values for their own laboratories processing these specimens.
Our findings demonstrate that a cyst fluid CEA of 30.7 ng/mL is not only useful in the diagnosis of all mucinous cysts (including both MCNs and IPMNs), but maintains its diagnostic accuracy (PPV=94.7%) when looking at a subset of only histologically verified IPMNs. The lack of difference in median cyst CEA levels between MCNs and IPMNs can be attributed to the fact that the histopathological features of the two subtypes are almost identical except for the presence of ovarian-like stroma in MCNs [5].
Few studies have shown a utility of cyst CEA levels in predicting malignancy. Several groups have demonstrated that CEA can predict malignancy; however in these studies the CEA cut-offs vary greatly (200 to 5000 ng/mL) [53-55]. Others have shown CEA to be an unreliable predictor of malignancy [25, 56]. In our study, there was no significant difference in median cyst CEA levels between malignant and non-malignant mucinous cysts; however, an unexpected trend towards lower levels was observed with malignancy. The wide range of cyst CEA levels in the 13 malignant cysts (Figure 1; 3.2 – 49802 ng/mL) and the low incidence of malignancy in our study (13/77, 17%) limits our ability to fully examine the role of cyst CEA in predicting malignancy. The lack of an association between degree of cyst CEA elevation and dysplasia limits its value beyond that of identifying a mucinous lesion. While cyst CEA has utility in guiding patient management, it cannot be used a sole marker for identifying lesions that need operative resection.
The present study has a number of weaknesses. Patients were selected from those who underwent operative resection of a pancreatic cyst. While this allowed us to use surgical pathology as the diagnostic-standard to compare cyst CEA levels, there is inherent selection bias in the subjects themselves. The determination for surgical resection was made based on recommendation of the surgeon and patient acceptance or preference and likely reflects the concern for malignancy based on pre-operative findings. As such, the majority of cysts in our study were of the higher risk, mucinous variety. Nonetheless, the prevalence rates of malignancy were consistent with prior reports of surgically-resected mucinous and nonmucinous cysts. Finally, the majority of patients (61%) who underwent pre-operative EUS did not undergo FNA or did not have sufficient cyst fluid for CEA analysis and were excluded from the study.
In conclusion, our study demonstrates that a much lower cyst CEA cut-off than previously reported predicts mucinous cystic lesions of the pancreas with greater accuracy. This finding has profound implications for identifying individuals with neoplastic lesions that require long-term surveillance imaging. This same CEA cut-off of 30.7 ng/mL was validated in a subgroup of patients with IPMNs. Cyst CEA cannot reliably distinguish MCN from IPMN or a malignant from a non-malignant mucinous cyst and should not be used for further risk stratification.
The authors would like to acknowledge the efforts of Dr. Pari Shah and Dr. Gregory Bernstein in data collection.
The authors had no conflicts of interest