- (2013) Volume 14, Issue 3
John G Lieb II1*, Phillip P Toskes2
1Division of Gastroenterology, University of Pennsylvania. Philadelphia, PA, USA
2Division of Gastroenterology, University of Florida. Gainesville, FL, USA
*Corresponding Author:
John G Lieb II
9 Penn Tower, Division of Gastroenterology
Hospital of the University of Pennsylvania
1 Convention Blvd; Philadelphia
PA 19104; USA
Phone: 215 349 8222
Fax 215 823 4179
E-mail: john.lieb@uphs.upenn.edu
Received August 25th, 2012 – Accepted January 30th, 2013
Context Estrogens are thought to cause pancreatitis by raising triglyceride levels but whether there are other effects on the pancreas is debatable. Objective To better elucidate the relationship between estrogens and pancreatitis and pancreatic function in a pilot study. Design/setting/patients Our retrospectively collected database of 224 patients who had undergone secretin stimulation testing was queried for females with available medication histories, who were then divided into two groups: those taking estrogens (E) and those not on estrogens (N). Mann Whitney U and Fisher’s exact tests were used. Results Seventy of the patients in the database were females with available medication histories. Thirty-five (50.0%) were taking estrogens. Twenty-nine (82.9%) of the E patients experienced any type of pancreatitis (i.e., acute pancreatitis, acute relapsing pancreatitis, chronic pancreatitis) while only 19 (54.3%) of the N patients did (P=0.019). During secretin stimulation testing, the peak bicarbonate levels for E and N patients were 80±18 and 90±23 mEq/L, respectively (P=0.058). When patients with any type of pancreatitis were excluded, E patients still displayed decreased peak bicarbonate levels in response to secretin (90±18 vs. 104±19 mEq/L; P=0.021). Weight, age, triglyceride levels, frequency of patients with cholecystectomy and biliary stones did not significantly differ between the two groups (E and N respectively). Conclusions These pilot data suggest exogenous estrogens may be related to the development of acute pancreatitis and acute relapsing pancreatitis, and probably to a lesser degree chronic pancreatitis, perhaps through a triglyceride independent mechanism. During secretin stimulation testing, peak bicarbonate production may be diminished in women on estrogens (even inthose who have never had pancreatitis). Further study is necessary to better define the relationship between estrogen use,pancreatitis, and pancreatic function.
Keywords
Abdominal Pain; adverse effects [Subheading]; Estrogens; Pancreatic Function Tests; Pancreatitis; Pancreatitis, Acute Necrotizing; Pancreatitis, Chronic; Secretin
Abbreviations
SST: secretin stimulation testing
INTRODUCTION
Estrogens are known to be related to pancreatitis but this is thought to be due to effects on serum triglycerides or biliary stone formation [1, 2, 3, 4]. Some case reports have suggested there may be a relationship between estrogens and acute pancreatitis independent of triglycerides, including a case of a woman taking an herbal supplement (Avlimil®, Vianda Co., Cincinatti, OH, USA) containing phytoestrogens who developed acute pancreatitis [5], and a post menopausal woman taking estrogens who had two well defined and separated episodes of acute pancreatitis [6], both of whom had no change in lipid profile or evidence of biliary lithiasis. Of note on rechallenge, the woman taking the herbal supplement did not get recurrence of the pancreatitis. Another interesting case described a woman who was well when taking both estrogens and progestins but then developed acute pancreatitis when she stopped the progestins [7]. However, outside of case reports, there has been very little evidence to suggest that estrogens could cause pancreatitis in patients with normal lipids and without gallstones up to this point. For example, one large retrospective epidemiologic study in Denmark of over 1,000 women discharged with acute pancreatitis and 10,000 controls did not show any evidence of an effect of estrogens on the development of pancreatitis [8]. However, this study included only women over age 45 in their analysis.
We had already developed a database of patients who had presented to the University of Florida for a question of chronic pancreatitis, and therefore had undergone secretin stimulation testing (SST), 91% of whom had chronic unexplained abdominal pain [9]. SST is a test that has proven very accurate in the diagnosis of chronic pancreatitis, even in patients with no other obvious evidence of chronic pancreatitis and represents one of the most sensitive tests of pancreatic function [10, 11]. We typically consider patients with a peak bicarbonate level of less than 80 mEq/L to have SST results consistent with chronic pancreatitis.
As we were developing and filling the database we noticed that a seemingly inordinate number of patients with acute relapsing pancreatitis and chronic pancreatitis, often with unexplained etiologies for their disease, were taking estrogens. Thus we set out to use this database, within the limits available, to run a pilot study to address the question of whether patients taking estrogens might have increased rates of pancreatitis (acute, chronic and acute relapsing). Since we also had SST data (pancreatic function) on all these patients, we felt this endeavor could contribute to knowledge of pancreatic physiology.
METHODS
Two-hundred and 24 patients with secretin stimulation testing performed at the University of Florida already included in our database were investigated for the presence of accurate/retrievable medication histories. Of note, many of these patients were from the 1990s and thus handwritten charts were reviewed. Some were not retrievable. Seventy women were found that had available medication histories, 35 of whom (50.0%) were taking estrogens and 35 (50.0%) were not and were thus divided into two groups, we termed “E” and “N”, respectively. Patients were included in the estrogens group if they were actively taking oral, injectable or transdermal estrogens, esterified estrogen with methyltestosterone, and tamoxifen. Patients were excluded in the case of pancreatitis caused by hyperparathyroidism, pancreatic or ampullary cancer, trauma, or an obvious medication. Patients with significant biliary, lipid, and alcohol histories were not excluded due to small numbers and in order to better determine an interaction between estrogens and these factors.
The rates of acute pancreatitis, acute relapsing pancreatitis, and chronic pancreatitis in those two groups were then compared along with triglyceride levels, presence of gallstones/biliary stones, peak bicarbonate levels and volume of pancreatic juice collected during SST respectively in those two groups. Fasting triglyceride levels were recorded from the chart. As best as could be discerned in this retrospective fashion, these were levels taken between attacks of pancreatitis when the patient was feeling well. When several levels were taken from the patient, the highest value was recorded and used in this study. Clinical chronic pancreatitis, acute pancreatitis, and acute relapsing pancreatitis were defined according to the previous study on this database (see Lieb et al. [9]). Alcohol use was retrieved from the chart when possible. In order to better quantify the alcohol amounts documented on the chart, “heavy alcohol use” was converted to 60 g/day and “social alcohol use” was converted to 5 g/day.
STATISTICS
These values were then compared with Mann Whitney U testing, (for continuous variables) and Fisher’s exact testing for categorical variables. Such nonparametric methods were used since they are generally more robust and require fewer assumptions especially with these fairly small numbers. Tests were two-sided and P values were considered significant when less than 0.05. Since the database was a retrospective collection of prospectively occurring data, relative risks could be calculated together with their 95% confidence intervals. No Bonferroni correction was applied given the small size and pilot nature of this study. Statistical analyses were performed with SAS version 9.2 (SAS Institute, Cary, NC, USA). Unless otherwise indicated values are indicated ± standard deviation (SD).
ETHICS
This study was approved by the IRB of the University of Florida. The study protocol conforms to the ethical guidelines of the “World Medical Association (WMA) Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964 and amended by the 59th WMA General Assembly, Seoul, South Korea, October 2008. No informed consent was needed because this study is a retrospective analysis of a database collected for other reasons.
RESULTS
Of the 35 patients taking estrogens, the vast majority (24, 68.6%) were taking Premarin® (Wyeth Pharma, Madison, NJ, USA; hitherto referred to as conjugated equine estrogens). One patient was taking an Estraderm® (Norvartis Co., East Hanover, NJ, USA; estradiol transdermal) patch at 0.05 mg with estrogen “injections”. One patient was taking “estrogen 1.75 mg by mouth once daily and progestin.” Three others were taking just an estrogen patch without a dose given. Two were taking oral Estrace® (Warner Chilcott Laboratories, Rockaway, NJ USA; henceforth refered to as oral estradiol) 1 mg daily. One patient taking esterified estrogens with methyltestosterone and one taking tamoxifen were included (doses not listed). In addition, two patients were listed as taking oral estrogens but the exact type and dose were not specified on the chart. The dose was not listed in 10 (41.7%) of the 24 patients who were taking conjugated equine estrogens, while eight of the 14 patients were taking 0.625 mg of conjugated equine estrogens, one patient was taking 0.9 mg, four patients were taking 1.25 mg daily, and one patient was taking 0.3 mg daily. No patients were recorded to be on oral contraceptives. The majority of the patients were post hysterectomy (23, 65.7%) and in the remaining 12 of the patients there was no listing of hysterectomy on the chart. Because of the lack of dose data on many patients and the small sample size, subgroup analysis based on dose/type of estrogen preparation was not possible.
As far as baseline data (Table 1), among the two groups (E and N, respectively), weight (65.9±15.5 and 64.8±16.7 kg; P=0.741) and age (52.2±10.9 and 47.6±15.6 years; P=0.118) did not differ significantly. Seventeen patients (48.6%) in the E group and 16 (45.7%) in the N group had available lipid profiles with mean triglycerides of 280±250 and 286±198 mg/dL, respectively; P=0.631. Only two (5.7%) of the E and three (8.6%) of the N were believed (as documented in the pancreatic clinic notes) to have had pancreatitis from hypertriglyceridemia (P=1.000).
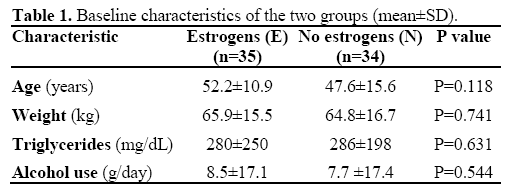
The frequency of patients with either prior or recent cholecystectomy (19, 54.3% vs. 18, 51.4%; P=1.000), gallbladder stones (2, 5.7% vs. 5, 14.3%; P=0.428), common bile duct stones (1, 2.9% vs. 2, 5.7%; P=1.000), sphincter of Oddi dysfunction (manometrically proven) (3, 8.6% vs. 2, 5.7%; P=1.000), or biliary dyskinesia on cholescintigraphy (2, 5.7% vs. 4, 11.4%; P=0.673) or gallbladder sludge (2, 5.7% vs. 0; P=0.493) between the E and N groups, respectively, did not differ significantly (Figure 1).
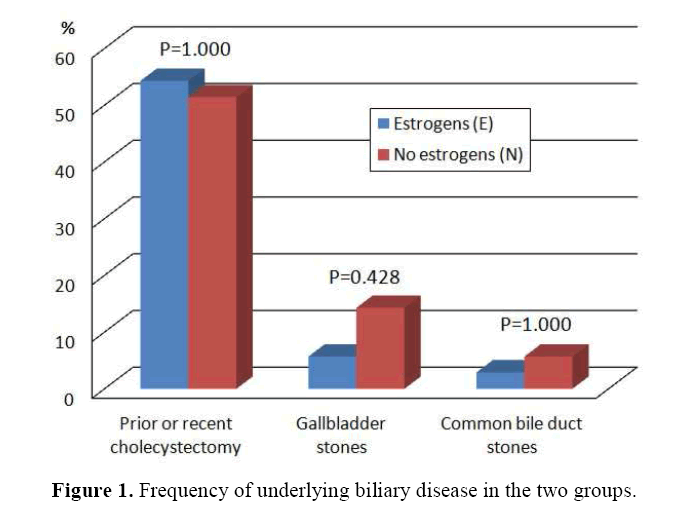
Figure 1. Frequency of underlying biliary disease in the two groups.
Patients in the non-estrogens group (N) were more frequently diagnosed with gastroparesis than those on estrogens (E) (20, 57.1% vs. 10, 28.6%; P=0.029).
Four patients in the estrogens group (11.4%) and 6 in the non-estrogens group (17.1%) lacked any alcohol history whatsoever. Average alcohol (ethanol) consumption was 8.5±17.1 g/day in the estrogens group (13 patients) and 7.7±17.4 g/day in the group not taking estrogens (10 patients), showing a nonsignificant difference (P=0.544). Eighteen patients in the estrogens group (58.1%) and 19 in the nonestrogens group (65.5%) reported no alcohol consumption in the paper chart (P=0.603).
Nineteen patients in the E group (54.3%) and 15 in the N group (42.9%) had chronic pancreatitis by clinical criteria (P=0.473; relative risk: 1.27, 95% confidence interval: 0.78-2.07). Twenty-nine of the E patients (82.9%) experienced any type of pancreatitis (acute, acute relapsing, chronic) while only 19 of the N patients (54.3%) did (P=0.019; relative risk: 1.53, 95% confidence interval: 1.09-2.14) (Figure 2).
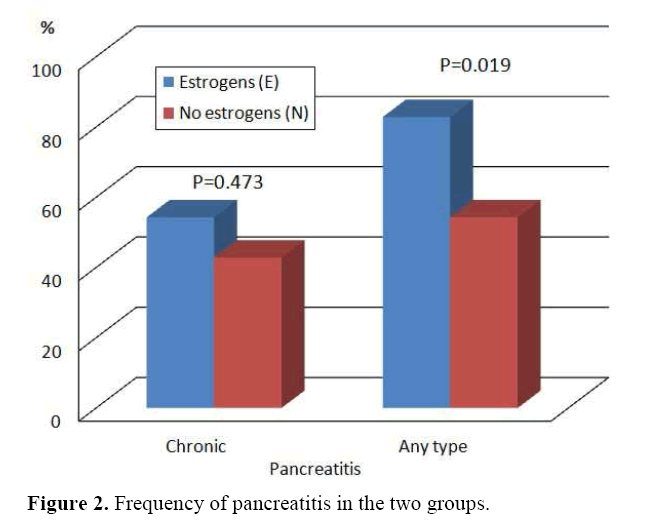
Figure 2. Frequency of pancreatitis in the two groups.
During SST, the mean peak bicarbonate levels for E and N patients were 80±18 and 90±23 mEq/L, respectively (P=0.058; Figure 3). Total volume of pancreatic juice collected during secretin stimulation testing was not significantly different (212±91vs. 213±107 mL, respectively; P=0.961). When patients with any type of pancreatitis were excluded, E patients still displayed significantly decreased peak bicarbonate levels in response to secretin (90±18 mEq/L, n=6 vs. 104±19 mEq/L, n=16; P=0.021). Total volumes were still similar at 209±95 vs. 208±72 mL (P=0.945).
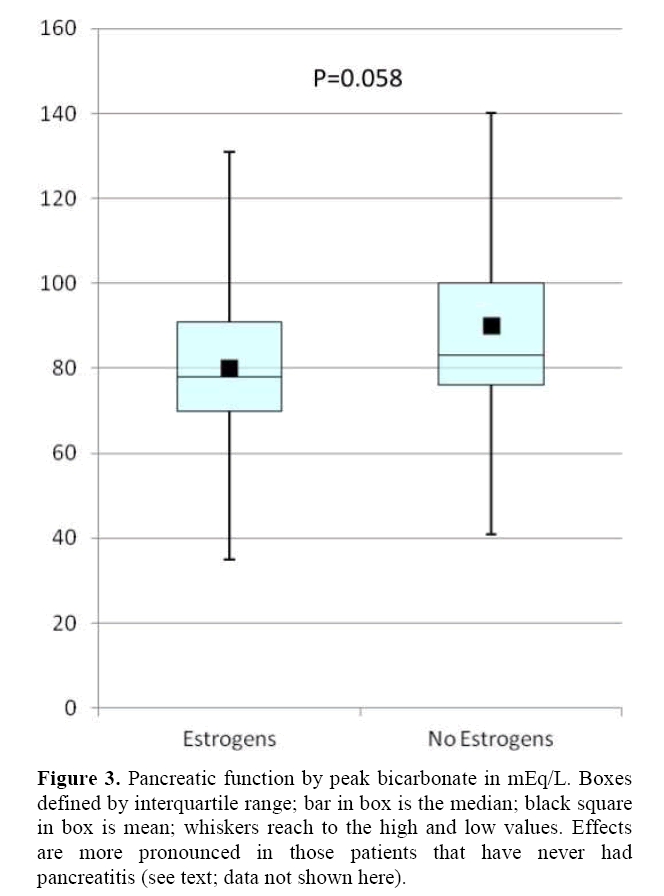
Figure 3. Pancreatic function by peak bicarbonate in mEq/L. Boxes defined by interquartile range; bar in box is the median; black square in box is mean; whiskers reach to the high and low values. Effects are more pronounced in those patients that have never had pancreatitis (see text; data not shown here).
DISCUSSION
Within its obvious limitations, this pilot retrospective study suggests, but certainly does not prove, the following: 1) estrogens may be related to acute or acute relapsing pancreatitis; 2) the effect of estrogens on chronic pancreatitis is less certain from these data, though a trend probably exists and we hypothesize it may be related to relapses of acute pancreatitis; 3) estrogens probably have some effects on pancreatic function and especially they may diminish peak bicarbonate production, probably independent of whether acute pancreatitis is present or not; 4) in this population, these effects of estrogens on patients with chronic abdominal pain, are likely unrelated to hyperlipidemia or biliary lithiasis.
Mechanisms for these effects are uncertain. Although no conclusions can be drawn regarding mechanisms from the data in this study, for the purposes of hypothesis generation we feel it is worthwhile to speculate as reported in the following suggestions.
One group recently found that estrogens may increase duodenal production of bicarbonate in women in Hong Kong [12] and this could perhaps suppress basal response to endogenous secretin, though probably should not affect the supraphysiologic doses of secretin intraveounsly given during SST. However, it is possible that estrogens may increase duodenal bicarbonate production as from Brunner’s glands and thus decrease endogenous secretin, thus removing a trophic effect of secretin on the pancreas. And thus when exogenous secretin is given via SST, the pancreas may not respond as well as in those who are not taking estrogens.
Secretin, for example, is hypothesized to reduce the rate of post ERCP pancreatitis [13] perhaps by flushing the pancreas of damaging substances such as contrast and bile reflux. Although a recent well done study did not show a difference, it was performed at a tertiary medical center known for its ERCP skills where baseline cannulation rates and ease of cannulation were doubtless much higher than in most small centers. Thus the ability of secretin to prophylax for post ERCP pancreatitis has not quite been disproven in our opinion.
If the role of secretin is established in preventing pancreatitis, it is conceivable then that if exogenous estrogens may negatively feedback on secretin production, bile reflux into the pancreatic duct and sphincter of Oddi spasm may be more likely to cause acute pancreatitis in patients taking estrogens. It is also conceivable that estrogens may lead to biliary microlithiasis that was not tested for, controlled for, or detected much in this study. It is also conceivable that estrogens may alter postprandial lipids even more commonly than fasting lipids, which have previously only been thought to be altered in patients on estrogen who have underlying hyperlipidemia. We did not measure postprandial lipids in these patients on estrogen, but this might be a line of interesting further investigation [14]. Data over the past few decades finally indicated that estrogens may increase the rate of stroke and less favorably alter lipid profile than previously thought [15]. Part of the hypothesized increase in cardiovascular disease in patients taking estrogens may be related to increased inflammation from estrogen use [16, 17]. If estrogens increase the inflammatory process, it is possible this could result in an increase in pancreatitis. On the other hand, some evidence suggests estrogens induce anti-inflammatory processes [18].
Estrogens may also represent a missing link between obesity and severity of pancreatitis. Obesity’s reported increase on the severity of acute pancreatitis is well known [19]. Also adipose tissue may act as a repository for endogenous or exogenous hormones. Some have even hypothesized that overweight patients may be more highly estrogenized [20]. Obese men may be particularly vulnerable since the testosterone produced is quickly aromatized to estrogen and stored in adipose tissue. If it is true that obese patients are more highly estrogenized, estrogen may be a mechanism by which obesity increases the severity of pancreatitis. It is also possible that estrogens may lead to obesity or change fat distribution that may make pancreatitis more likely. Of course, in contrast some have also suggested that estrogens reduce the typical weight gain experienced during menopause [21].
However, admittedly, there are several drawbacks to this pilot study. This is a small study. Many patients did not have complete medical histories available. We included only patients who had undergone secretin stimulation testing since they were available in our database for study. These patients are already enriched in pancreatic diseases and are suspected of having chronic pancreatitis for a variety of reasons. On the other hand, these are interesting patients, nearly all of whom have chronic abdominal pain that has hitherto been unexplained. As such, it is conceivable many of these patients had undergone hysterectomy/ oophorectomy for abdominal pain of presumed gynecologic origin and then required estrogen replacement. It could be then that estrogen use is just a marker of chronic abdominal pain, not a cause. Or simply that this group of patients, as a result of chronic unexplained abdominal pain, is highly enriched in post hysterectomy/oophorectomy patients (patients on estrogens). However, this statement alone cannot explain the much higher rate of pancreatitis in patients taking estrogen compared to patients in the database with chronic abdominal pain not taking estrogens. Many of these charts are rather old and there could be a bias in reporting estrogen use and taking an estrogen history in institutions where estrogens are thought to be related to pancreatitis or at institutions where hyperlipidemic pancreatitis is prevalent.
Another issue is that patients on estrogens tended to be perimenopausal. Thus, although the ages of patients on or not on estrogens were not statistically dissimilar, there was a trend; i.e., patients on estrogen tended to have less variability in age, whereas patients not on estrogen tended to be bimodal with respect to age, either fairly young or fairly old. This could have biased the data, though this bias would probably be present for any observational study of estrogen use which probably peaks around menopause.
Also, there are somewhat more gastroparesis patients in the group not taking estrogens, which was somewhat of a surprise, and could reflect referral bias in that, because more patients in the estrogen group had chronic pancreatitis, gastric emptying testing may not have been done, since a reason for the chronic abdominal pain had been found. However, potentially estrogens may have effects on gastric emptying which could have decreased the pH of the duodenal fluid collected on estrogen patients, in turn affecting the SST results. Although gastric emptying studies were significantly different in the estrogens vs. the nonestrogens groups, not every patient had one.
Also there were no reports of oral contraceptive use. This is a bit unusual and probably reflects the fact that a history of oral contraceptive use is not typically solicited during gastrointestinal consultation. This may have biased the results since many of the women listed in the nonestrogen group may have been taking oral contraceptive pills. Or perhaps, fewer women than expected were found to be on oral contraceptive pills due to the high rate of post hysterectomy status in this population.
Also we did include one patient on tamoxifen. Tamoxifen’s effects are complex and may not accurately represent the effects of conventional estrogens on the pancreas.
Our decision not to exclude patients with significant alcohol, hyperlipidemic or biliary histories was a complex one and may have affected the data. If we had excluded all of these patients the study would not have been statistically plausible or generalizable. However, very few of the patients were thought to have hyperlipidemia as a cause of their pancreatitis (3 in the non-estrogen group and two in the in the estrogen group). To truly determine the role of estrogens in idiopathic pancreatitis, we admit that we would have to find not only many patients with idiopathic pancreatitis but also many on estrogens.
Although alcohol consumption data appear to be similar in both groups, the alcohol use in the chart at times was not precisely quantified. This is common in any study of alcohol use, utilizing chart review. Also there could be errors related to assuming “heavy drinking” was 60 grams daily (though there were only two “heavy drinkers” in each group). Also the assumption of 5 g/day in “social drinkers” may be error prone. In addition, each group had no alcohol data for about 10-20% of patients. It seems unlikely though that alcohol use should be much more pronounced in one group and thus unlikely that these factors affected the interpretation of the results.
Nevertheless, these results we feel are interesting, especially in light of the fact that up to 20% of pancreatitis patients remain idiopathic in spite of an exhaustive search at tertiary medical centers [22]. Could estrogen use explain a portion of these patients? Further studies are needed in larger populations. Further study of cholecystokinin-stimulation testing in patients on estrogens may be worthwhile to see if pancreatic ecbolic secretion is affected as much as the hydraulic secretion. In the meantime, pancreatologists need to take careful medication histories especially in regards to estrogen-containing conventional prescriptions as well as homeopathic and herbal preparations.
Financial support
None
Conflicts of interest
None