Research Article - (2012) Volume 2, Issue 5
1Department of Clinical Psychology, University of Social Welfare and Rehabilitation, Iran
2Department of Psychology, University of Social Welfare and Rehabilitation, Iran
3Department of Psychiatry, University of Social Welfare and Rehabilitation, Iran
4Department of General Psychology, Science and Research branch, Islamic Azad University, Tehran, Iran
This research investigates the efficacy of GCBT, GCRT and CCT in reducing positive and negative symptoms of schizophrenic patients and improving their cognitions and social functioning. A Randomized Controlled Trial was used to compare the efficacy of these three methods on patients who receive treatment as usual (TAU). 60 inpatient people with schizophrenia and persistent negative and positive symptoms were selected from Razi hospital in Tehran. Patients were at age 25 to 55 years; had diagnosis of schizophrenia for at least 2 years and were persistent to medication. 40 of them received 32 sessions treatment over 3 months and 20 of them were in waiting list. All Patients received TAU throughout the study. The positive and negative symptoms scales (SAPS & SANS), NOSIE & NCSE completed for all patients on sessions first, eight, sixteenth, twenty fourth, and thirty sixth. Multivariate repeated measure was used for data analysis. Multivariate repeated measure showed the efficacy of combined cognitive therapy. The effect size showed the efficacy of CRT first- CBT next combination on improving cognitive scales but CBT first combined therapy is more effective on general psychopathology. It is more effective on negative and positive scales and behavioral functioning than other types of therapy. GCBT with remediation therapy components is the efficient supplementary therapy in combination with pharmacotherapy in treatment of patients with schizophrenia.
Schizophrenia, Group Cognitive – Behavior Therapy (GCBT), Group Cognitive Remediation Therapy (GCRT), Combined Cognitive Therapy (CCT).
Schizophrenia is a severe psychiatric illness, afflicting approximately 1% of the population worldwide [22]. As is clear from a review of the characteristic symptoms and impairments of schizophrenia, this disorder is multiply handicapping, impacting all aspects of life. Schizophrenia remains a debilitating disorder despite the development of drug treatments [27]. In the treatment of schizophrenia use of psychotherapy is clear, for one, pharmacotherapy commonly considered as cornerstone in the treatment of schizophrenia have limitations. Despite using medication, relapse rates remain substantial. Furthermore, a considerable number of schizophrenic patients don’t response to medication despite of ongoing medication regimen. Current neuroleptic drugs have little beneficial effects on negative symptoms, residual cognitive impairments, and social functioning [20]. Various researches considered a multimodal and integrative intervention with pharmacotherapy, psychotherapy and social support as a sufficient treatment for schizophrenic patients [15]. However, the question is which of them is more effective?
From the available meta-analyses, social skills training, cognitive remediation, psycho educational coping-oriented interventions with families and relatives, as well as cognitive behavioral therapy emerge as effective adjunctions to pharmacotherapy. Social skills training consistently effectuates the acquisition of social skills, cognitive remediation leads to short-term improvements in cognitive functioning, family interventions decrease relapse and hospitalization rates, and cognitive behavioral therapy results in a reduction of positive symptoms. These benefits seem to be accompanied by slight improvements in social functioning [15]. But different interventions is not yet well- known the idea of combination of CBT and CRT which can cover both positive and negative symptoms of schizophrenia commented. It can improve neuropsychological functioning and therefore improve social and behavioral functions. In Integrated psychotherapies, different researches integrated Cognitive remediation therapy, Social skills training and Problem solving education but there is a gap for effective empirically based Cognitive psychotherapies between integrated psychotherapies [18]. Although there are many researches for efficacy, current treatments don’t affect on all signs and symptoms and the aim of combined cognitive therapy is decreasing symptoms and planning a new rehabilitation program for schizophrenic patients. This is a rehabilitation program proposed that dysfunctional information processing lead to cognitive disorders and schizophrenic symptoms pulp up. Finally it leads to social dysfunctions. In addition, functional problems and schizophrenic symptoms lead to social rejection and experiencing isolation and alienation. This research combined 2 different approaches in treatment of schizophrenia and designing a new model from combination of GCBT and GCRT for a better clinical treatment.
Design
This was a double-blind, randomized controlled trial of new therapies to improve function in people with schizophrenia with comparing various groups. The first group received 36 sessions of GCRT and then GCBT. The second group received 36 sessions of GCBT and then GCRT, and the third group who received only treatment as usual (TAU). After baseline assessment, participants were randomized to either under treatment or control group and then were assessed at session 8th (middle of the first treatment) and session 16th (after the first treatment), and then at session 24th (middle of the second treatment) and session 32 (after the second treatment).
Participants and recruitment
We selected participants of schizophrenic patients from Razi psychiatric center in Tehran- Iran. Their Sixty men and women were drawn from consecutive recruits in an ongoing randomized controlled trial. A sample size of 60 would demonstrate a significant difference between the 2 treatments with 80% power, 0/05 level of confidence and 0/02 error on the basis of Cohen sample size table. As we considered dropout, we selected 66 sample (22 patients for each group).
Patients were included if they had been:
- diagnosis of schizophrenia based on DSM–IV-TR (American Psychiatric Association, 2000) and psychiatrist diagnostic interview. The schizophrenia diagnosis should confirmed by SCID (Structured clinical interview).
- The age range of 25 up to 50 years old
- at least one year has passed from onset of schizophrenia
- at least educated for 8grade.
- evidence of both negative and positive symptoms defined as a score on the SAPS and SANS Exclusion criteria were:
- not being on acute phase
- no evidence of organic brain disease and no primary diagnosis of substance misuse;
- no evidence of serious side effects of antipsychotic drugs which need extra treatment.
- not received ECT before treatment for 6months or during treatment.
All participants or their family members assigned written consent to take part in this study after explaining the program. The groups did not differ in mean age (First group: μ=35 years; Second group: μ=36 years; control group: μ=36 years)
and there were no differences between groups in the mean number of years of formal education (μ1=13, μ2=12 and μ3=12 years, respectively). The patients were chronic ones with more than two-thirds having been in contact with the psychiatric services.
Intervention
The research conducted in Razi center by 9 therapists have been trained in CBT and CRT for psychotic patients supervised by expert cognitive-behavior and cognitive- remediation therapists. They had M.A or Ph.D in clinical psychology. CBT and CRT were both delivered by the same therapist to control for non-specific factors. An attempt was made to deliver the same amount of face-to-face contact to each group. At the beginning of the study, the therapists have been trained for interventions and throughout the study they had received separate expert supervision on a regular basis for maintaining treatment quality. Standard psychiatric care in the Razi hospital is pharmacotherapy which received by all patients as TAU (Treatment As Usual).
Assessors were not aware of treatment allocation. Frequency of sessions was 2 times in a week and duration of the sessions were flexible from 30 minutes to 45 minutes to accommodate the needs of group. 32 sessions were conducted for each group. During treatment two patients withdrew from the first experimental group, one of them due to death and the other one due to relapse and 1 from the second group due to discharge from hospital and not follow the sessions and 1 patient in control group didn’t continue the treatment.
GCBT
The GCBT approach has been described in manualised form [29]. Early sessions focused on engaging, normalizing and developing explanations for distressing psychotic symptoms. Thereafter vulnerability–stress formulations were jointly constructed. Auditory hallucinations were tackled by developing coping strategies backed up by voice diaries. Paranoid delusions were dealt with using the development of alternative explanations and reality testing homework. Affect and cognition recognition and labeling were worked on in session. Negative attitudes to medication were explored and modified through guided discovery. Very negative personal beliefs (schemas) which often perpetuate voice hearing and underlie delusional systems were collaboratively modified. Lastly a personal relapse prevention plan was agreed [29].
GCRT
This approach has been described in manualised form [25]. Each session involved a number of paper and pencil tasks that provide practice in a variety of cognitive skills that are set out in a manual. The session plan included treatment alliance, introducing the program, Visual-spatial concentration tasks, hyper vigelency, attention retention to auditory stimulants, visual- auditory memory improvement, logical memory, orienting, selective attention, attention processing, digit span and word association, planning, sequencing, time monitoring, vanishing a queue, goal management thinking, problem solving, time- place imagery and organization and chaining categories.
Treatment-as-usual
Patients included in the treatment-as-usual condition met the same criteria as those who received therapy. Treatmentas- usual consists of the spectrum of available services, including medication management, and may have included case management, but not specific psychotherapy.
Assessments
The main outcome assessments were the Cognistat (NCSE), Nurses’ Observation Scale for Inpatient Evaluation (NOSIE), the Scale for Assessment of Negative Symptoms (SANS) and the Scale for Assessment of Positive Symptoms (SAPS). The Cognistat is a standardized neurobehavioral screening test. It describes performance in central areas of brain-behavior relations: level of consciousness, orientation, attention, language, constructional ability, memory, calculations and reasoning (Rabin et al., 2005). Rabin, Barr and Borton reported at least 0.70 reliability for each sub scales. NOSIE developed by Honigfeld & Klett. It is a 30 item scale to assess behavior pathology of patients. It contains 30 designated behaviors. The reliability is 0.73 to 0.74 [23]. SANS and SAPS is designed by Andersen (1983) with24 and 35 items on a Likert scale from 0 to 6. Use of this measurement is common due to high validity and reliability (Hoff, 2002). Internal consistency for SANS is 0.94 and SAPS is 0.83 and pre – post reliability of SANS is 0.92 and for SAPS is 0.88 [35].
Statistical Analysis
Baseline differences in sociodemographics, clinical characteristics and psychosocial functioning between the experimental groups and the TAU group were compared using Kroskal-Wallis test. Group differences in change scores for symptom severity and psychosocial functioning were examined using multivariate repeated measure. It were employed for SANS, SAPS, NCSE and NOISE in session 1, 8, 16, 24 and 32 between experimental groups and control group. Multivariate analysis of Variance (MANOVAs) was used to compare the differences in change between the intervention and control groups. In order to control for the effect of baseline effect, pre test score variable was included in the MANOVAs.
During the study three patients had dropped out, one of them due to death, 2 of them due to relapse to acute phase. Two of them had belonged to CRT-CBT group and one of them in the CBT-CRT group.
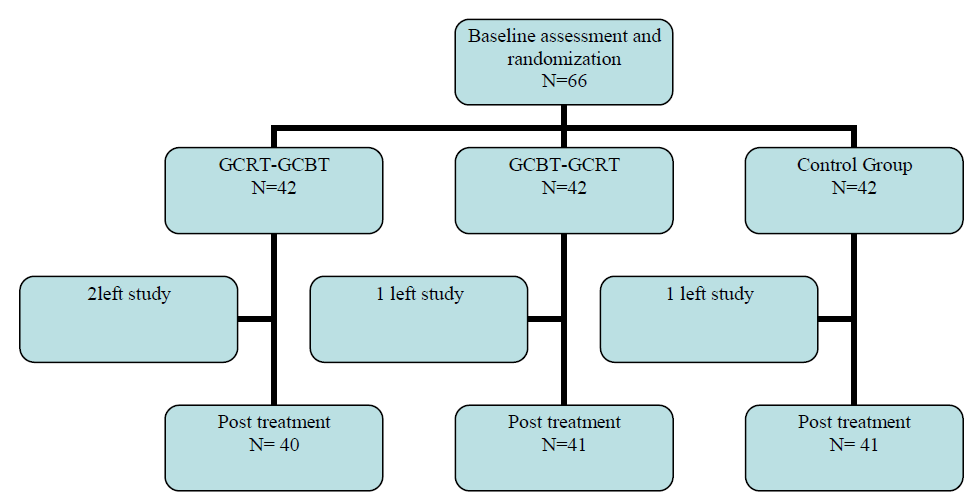
All of 20 patients were enrolled in the GCRT condition and then GCBT. 21 patients were enrolled in the GCBT and then GCRT and 22 schizophrenic patients were selected as control group that received treatment-as-usual .They were matched by age, educational level, duration of illness and type of medication with other groups. There were no significant differences in demographic variables between these three groups (Table 1)
Baseline differences in sociodemographics, clinical characteristics and psychosocial functioning between the experimental groups and the TAU group were compared by using Kroskal-Wallis tests. Group differences in variable scores for symptoms and cognitive and behavioral functioning (i.e. 4-month treatment ratings minus baseline ratings prior to treatment) have been showed in Table 1.
Effects of treatments between three groups on the SAPS, SANS, COGNISTAT and NOSIE scale compared by multivariate repeated measure and MANCOVA with the baseline score as covariate. These data are presented in Table 2. Using 3 first measures (pre test, middle of therapy and post- test) for evaluating efficacy of just CRT and CBT.
In each scale there were a measurement for assessing the relation between levels. Muschley used for normality and then looked for between subjects effects. Bonferroni used when differences were significant. Effect size used for measuring efficacy of treatments.
We can see the changes in groups on profiles 1 to 9.
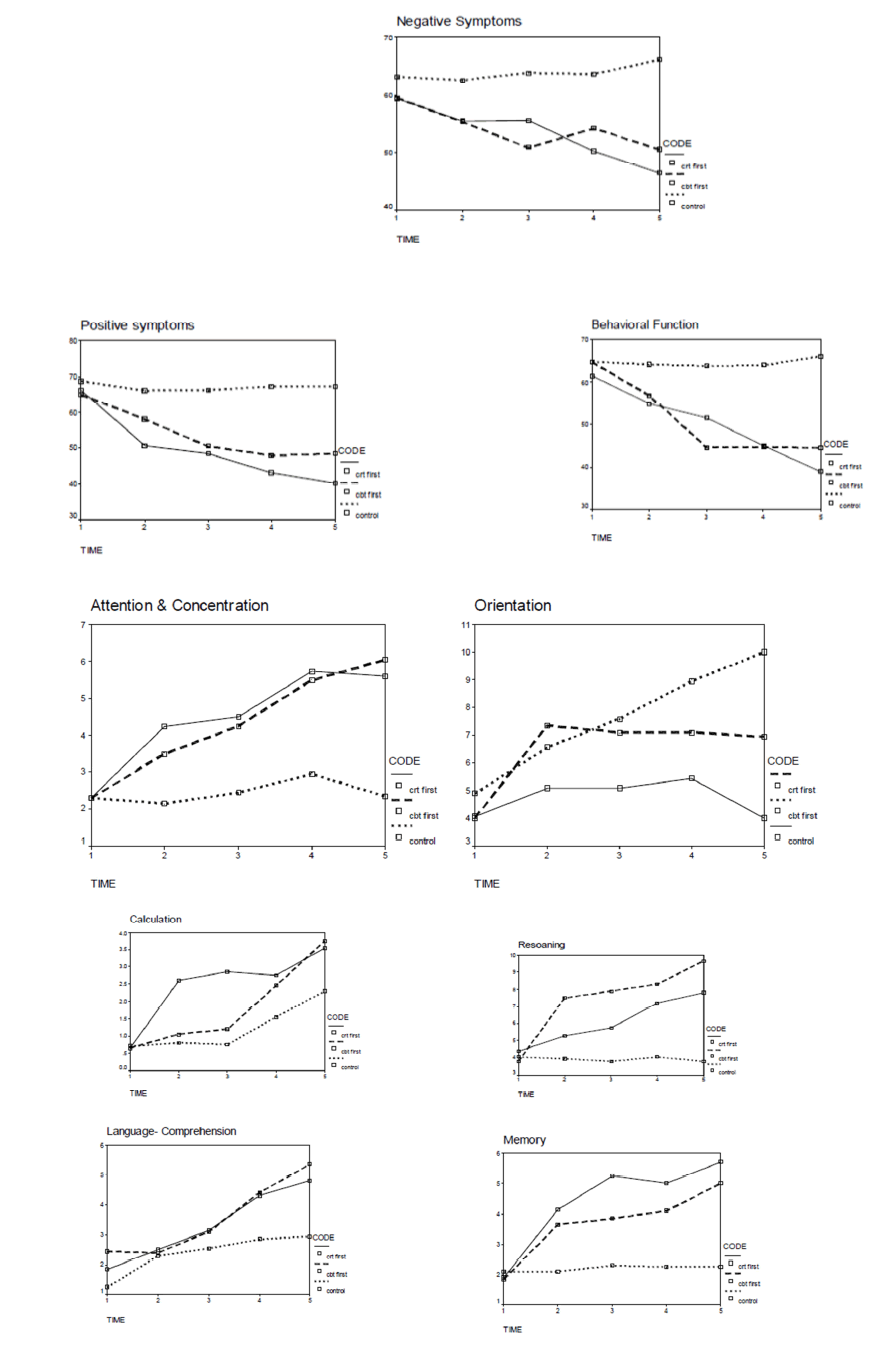
The initial analysis was detected a significant time by group. According to the initial model there was an estimated reduction in the CRT group of all points except behavioral function at the post-therapy time point (95%) which became enlarged to a statistically significant reduction in post test but the conclusions remained the same in control group.
There was a trend towards an interaction between randomization group and time and towards a main effect of randomization after adjusting for baseline differences. For comparing the efficacy of CBT and CRT and Combined cognitive therapy with 2 different type (CRT first- CBT next/ CBT first- CRT next) effect size (es) were compared and results showed in table 3.
Over the past years, evidence for the efficacy of psychological therapies on schizophrenic patients has been summarized in a series of meta-analyses. However, none of the existing meta-analyses summarizing the efficacy of psychological therapies in schizophrenia allows for a comprehensive and comparative review of the effects of psychological interventions [20]. Current research have evaluated four different types of therapy; CBT, CRT, Combined Cognitive Therapy (CRT- CBT), Combined Cognitive Therapy (CBT-CRT). The first central hypothesis of the study was that, group CRT would decrease significant negative psychotic symptom, was supported by these findings. There were significant differences between the experimental and control groups on measures of negative symptoms. Mean at pre test was 66.15 in CRT group and 55.60 at post test. For control group it was 60.55 on pretest and 66.35on post- test. This finding is approved by the key previous researches by Bark and et.al (2002), Bellucci et al. (2002), Doolatshahi et al. (2004), Wykes and Gaag (2001). The second central hypothesis was that GCRT would have significant effect on improvement of cognitive functions that was supported by these findings. There were significant differences between the two groups on measures of orientation, attention, language, memory and calculation. However, there were no significant differences between the two groups on measures of structural ability and reasoning. These findings are approved by previous researches by Bark et al (2002), Seltzler et al (1997), Velligan and Gonzalez (2007), Wykes et al (2005), and Wykes and Gaag (2001). Although this manual focuses on attention, memory and executive functioning but there is a generalized improvement on other areas of cognitions. It could conclude that there is no need for specific interventions for each deficit cognitive functions. The third hypothesis was: CBT can decrease positive symptoms in schizophrenic patients. It was supported by these findings. The effect size for positive symptoms was 0.67. This finding is approved by the previous researches by Addington and Gleeson (2005), Butler at al. (2006), Gaudiano (2006), Lawrence et al (2006), Lecardeur et al (2009), Pfammatter et al. (2006), Wykes et al (2007).
The fourth hypothesis was: CBT can improve behavioral function in schizophrenic patients. It was supported by these findings. The effect size for behavioral function was 0.69. This finding is approved by the previous researches by Wykes at al. (2007), Addington and Gleeson (2005), Lecardeur et.al (2009), and Beck and Rector (2005). On the basis of behavioral models and social learning theory, learning adaptive behavior through treatment sessions and enforcing this new adaptive behavior lead to change past maladaptive learning pattern and by enhancing behavior by psycho education, the patient’s ability for getting enforcements via interpersonal and social relationship will increase. Construct a new behavior resource can help patient to do his needs as well [16].
Does CRT effect on positive symptoms? Like several key previous trials [7,8,11,26] we included psychiatric symptoms especially positive symptoms and cognitive functions have different patterns. There are no significant differences between groups. Bustillo et al. (2001) reported there is no reason for relation between cognitive function and psychiatric symptomatology. Anderson (1993) and Craw (1980) point out that positive and negative symptoms are two different pathologies which appear autonomously or together. By this viewpoint, schizophrenia is the consequence of two different syndrome: Negative syndrome and Positive syndrome [4]. However effect size of positive symptoms is 0/21 which shows effect of CRT although there is no significant difference with control group. Does the CRT protocol effect on behavioral function?
The results showed the efficacy of CRT on behavioral function in our clinical trial. It’s a predictable result because behavior is associated with negative symptoms [4]. So, consequences of improvement on negative symptoms and cognitive function, behavioral function will improve. It’s despite of previous studies. They stated that CRT can not affect on behavioral function. Although they pointed that it need a long time for behavioral modification after CRT and it’s congruent with this research; we can see behavioral modification only in ending sessions and effect size is lower in comparison with other scales (es=0/24). Future studies should focus on longitudinal effects which need long fallow-ups. Does this recovery generalize to social empowerment and better psychosocial function? We need more studies to respond to these questions.
Does CBT affect on negative symptoms and cognitive functions? Multivariate repeated measure showed the efficacy of CBT on negative symptoms and Cognitive functions. In comparison between positive and negative symptoms we can see more change on negative symptoms (α =0/001 versus α =0/05). This is like Wykes et al. (2007); Penades et al (2006); Combz et al. (2006). In cognitive functioning, the improvement on language and calculation is more than other areas; we use Cognistat for cognitive evaluation and previous researches applied specific domain tests. So, more researches need to confirm the effects of program on language abilities. On the other side, the nature of treatment planning with exercises may play roles on all areas of cognition. Does improvement in one cognitive deficit generalize to other area and each cognitive deficits need specific planning? It needs more studies. Efficacy of both CBT and CRT are equal on negative symptoms and are significant, but there aren’t effective enough for positive symptoms. Efficacy of combined cognitive therapy (CBT first- CRT next) is suitable on behavioral functions (es= 0.51) and significantly different from CRT first- CBT next. The most efficacy is seen on cognitive functions in all types of treatments especially in combined cognitive therapy (CBT first- CRT next). In CRT first- CBT next, calculation and language skills have most benefit from treatment and the least is belong to positive symptoms. In CBT first- CRT next, calculation, structural ability and attention have most benefit from treatment and the least is belong to positive symptoms. The most discriminative effect size is about behavioral functions and attention. Although combined cognitive therapy (CBT first- CRT next) was effective for attention and behavioral function, combined therapy CRT first- CBT next is not effective for them. The results of the study reported here are consistent with the recently published randomized controlled trial of group CBT and CRT for schizophrenic patients. Both treatments lonely or combined therapy can improve function and relief symptoms. The idea of short term and compact combined cognitive therapy is a suitable theme to involve more defect dimensions of schizophrenia and lead to better quality of life. Alternatively (or additively), both previous studies on group CBT and CRT are commented for long term intervention while present study showed effectiveness of short term interventions. We proposed that concise interventions could optimally increase learning abilities and dominated on memory weakness. For patients, who might discharge from hospital after a period of time, we can use compact therapy. Most of the studies on cognitive deficits showed that taking clear adaptive information about real life, gradually and with enough frequency can be more helpful [29]. Of course, the socio-cultural adjustment of therapy for Iranian patients is very critical and one of the most important reason for successful intervention.