Juhi Taneja1, Agrawal VK2*, Danish Jamal3 and Zafar Abbas4
1Assistant Professor, Department of Microbiology, ESIC Medical College & Hospital, Faridabad, India
2Departmentof Critical Care Medicine, Metro Heart Institute with Multispeciality, Faridabad, Haryana, India
3Senior Consultant Pulmonary Medicine, Metro Heart Institute with Multispeciality, Faridabad, India
4Professor, Department of Radiodiagnosis, ESIC Medical College & Hospital, Faridabad, India
- Corresponding Author:
- Vijay Kumar Agrawal
Department of Critical Care Medicine
Metro Heart Institute with Multispeciality
Sector 16A, Faridabad, Haryana, India
E-mail: vkatbcd@hotmail.com
Received Date: September 22, 2020; Accepted Date: December 25, 2020; Published Date: December 30, 2020
Citation: Taneja J, Agrawal VK, Jamal D, Abbas Z (2020) A Rare Case of Pulmonary Mucormycosis Caused By Rhizopus Homothallicus in Post Heart Transplant Patient. J Intensive Crit Care. Vol. 6 No. 6: 23.
Copyright: © 2020 Taneja J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Rhizopus homothallicus, Mucorales, Pneumonia
Introduction
Mucorales are ubiquitous fungi causing infection in
immunocompromized hosts like carcinomas, immunosuppressive
therapy, uncontrolled diabetes, neutropenia, or patients on
desferroxamine therapy amongst which pulmonary mucormycosis
is the second common [1]. Mucormycosis is characterized by host
tissue infarction and necrosis resulting from vasculature invasion
by hyphae starting with a specific interaction with endothelial
cells [2]. However, infections due to Rhizopus homothallicus appear to be rare compared with those caused by other species
of zygomycetes [3]. Low incidence may be attributed to reduced
pathogenicity or its lower prevalence in the soil compared with
other Mucor species.
Case Report
A 57-year-old male, known case of post cardiac transplant 5
years back (on triple-drug immunosuppression -cyclosporine,
azathioprine, and prednisolone) along with type II diabetes
mellitus for more than 13 years with diabetic triopathy,
hypertension, non-oliguriac end stage renal disease (stage IV)
presented to us with high grade fever with cough, generalized
weakness and loss of appetite of one week duration. He had
history of hospitalization around two months back for acute
gastroenteritis. He was on antihypertensive drugs (β-blockers,
calcium channel blocker and alpha blocker) and insulin for
diabetes mellitus. His chest X-ray revealed focal patch of opacity
in right mid-lower zone suggestive of consolidation. At our
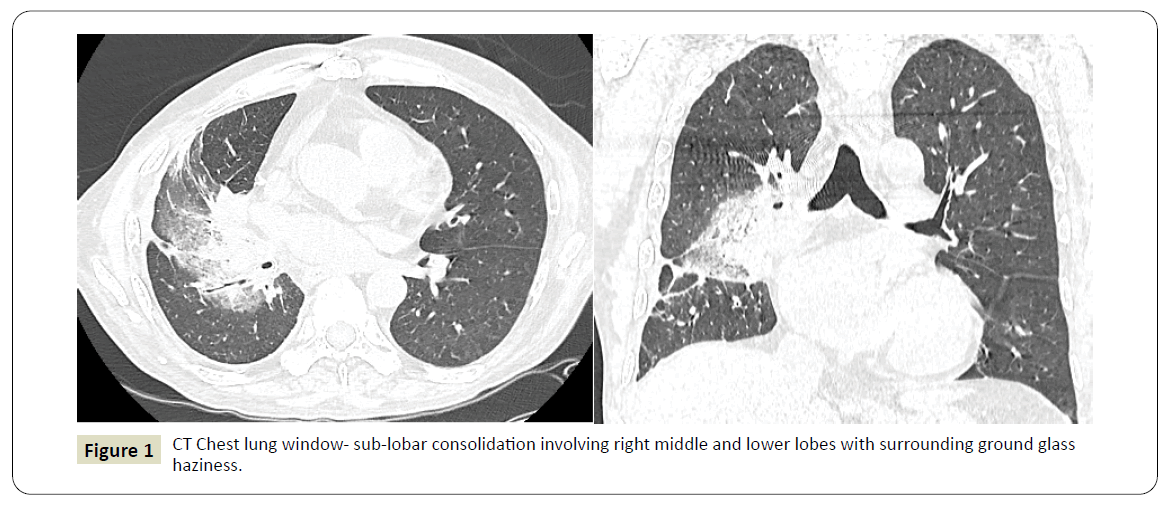
institute, contrast-enhanced computed tomography of the thorax
revealed patchy sub-lobar consolidation in right middle and
lower lobes with surrounding ground glass attenuation with large inhomogeneous area of ground glass attenation in right perihilar
region with small mediastinal and right hilar lymphadenopathy
suggesting possibility of mycoytic pathology (Figure 1). No pleural
effusion was noticed. Echocardiography ruled out endocarditis.
His blood sugar levels ranged from 153 to 226 mg/dl, total
leucocyte counts 14600 per cumm with polymorphs 84%, B. urea
103, S. Creatinine 4.1. His serum procalcitonin levels were raised
along with HbA1c of 12.82, indicating uncontrolled diabetic
status.
Figure 1: CT Chest lung window- sub-lobar consolidation involving right middle and lower lobes with surrounding ground glass
haziness.
Diagnostic bronchoscopy was performed and direct microscopic
examination with 10 % KOH of the bronchoalveolar lavage
specimen revealed ribbon-like broad aseptate hyphae with
branching at right angles. The samples were cultured on
Sabouraud’s dextrose agar (SDA) (HiMedia, Mumbai, India) and
incubated at 25ᵒ and 37 ᵒC. After 4 days of incubation, fast growing, cottony, white colonies were obverse with no pigmentation on
the reverse side of the tubes. The colonies turned grey after
prolonged incubation for 10 days. The colonies were teased
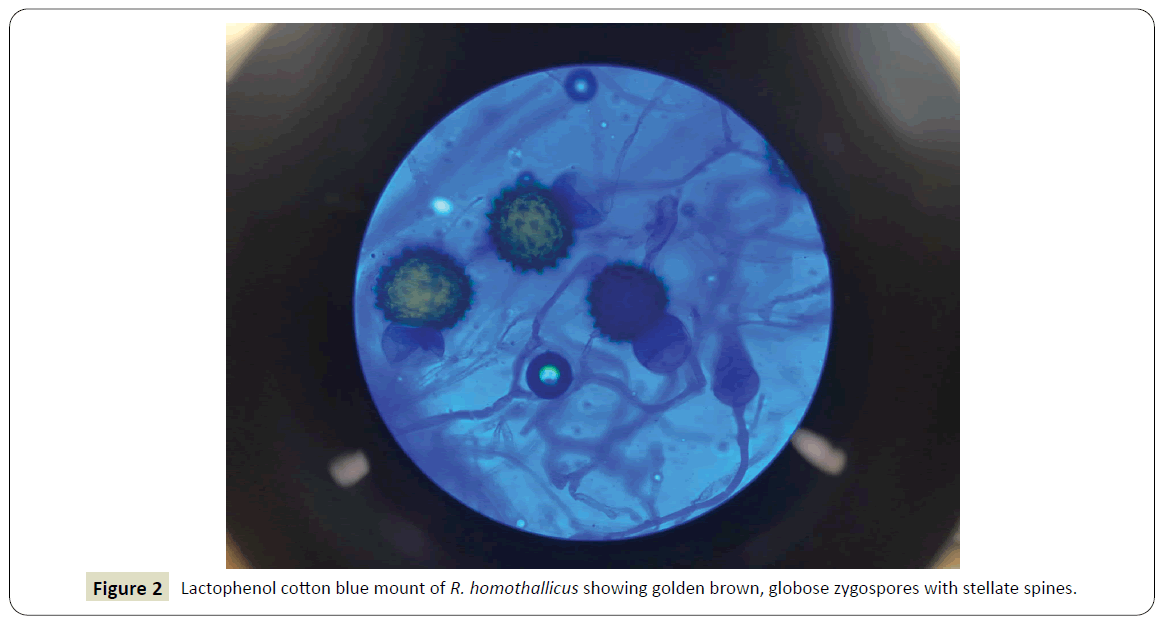
and stained with lactophenol cotton blue. When studied under
microscope, it showed poorly developed rhizoid tufts from
which arose few lateral sporangiophores measuring 100–150
μm in length. These bore a few globose sporangia with scanty
globose sporangiospores. A few globose, hyaline, intercalary
chlamydospores were also present. Sequential microscopic
changes could be observed as a large number of dark brown
zygospores measuring 60–100 μm in diameter with stellate
spines on their walls which developed after prolong incubation.
The suspensor cells were uneven with the zygospores attached
to the larger, globose suspensor cell (Figure 2). The isolates were thermotolerant and were able to grow when incubated up to 48
ᵒC. Based on these characteristics, the isolates was presumptively
identified as Rhizopus homothallicus. The isolate was further
confirmed by nucleotide sequencing of the 28S ribosomal RNA
(rRNA) region. The basic local alignment search tool (BLAST)
was used to compare the sequences obtained with those in the
GenBank database and to see the similarity of the isolate. The
sequences of isolate gave 98% identity with the ex-type strain of
R. homothallicus (CBS 336.62; GenBank: KU926333.1).
Figure 2: Lactophenol cotton blue mount of R. homothallicus showing golden brown, globose zygospores with stellate spines.
The patient was initially treated with broad spectrum antibiotics
along with antifungal voriconazole and echinocandins which
was later changed to intravenous liposomal amphotericin B 3-5
mg/kg IV qDay for 10 days. After a cumulative dose of 750 mg of amphotericin B, thepatient developed acute renal failure
and was managed with hemodialysis at regular intervals. After
showing initial improvement on amphotericin B, deteriorated
subsequently and developed sepsis leading to multi-organ failure
and death.
Discussion
Among the agents of zygomycosis, Rhizopus spp. are the most
commonly implicated agents causing human infection. This
is followed by genera such as Lichtheimia and Mucor. Among
Rhizopus spp., R. oryzae is the predominant species, being
implicated in 90% of the reported cases of invasive zygomycosis [3] R. homothallicus which was earlier considered an environmental
isolate, has been increasingly reported to cause invasive infections.
It has been reported to cause invasive pulmonary mucormycosis,
rhino-orbitocerebral and cutaneous mucormycosisin six patients
in India [4-6]. One case of fatal invasive pulmonary mucormycosis
has also been reported from France [7].
Mucorales gain entry to a susceptible host through inhalation,
ingestion of contaminated food, or through abraded skin. One of
the characteristic features of mucormycosis is its angioinvasive
property, resulting in vascular thromboses and ultimately
tissue necrosis. Angioinvasion was reported to be related to
the interaction between a spore-coating protein family (CotH)
on Rhizopus spp. surface and endothelium glucose regulator
protein 78 (GRP78) expressed at the surface of endothelial cells.
This interaction triggers host cell injury and subsequent fungus
hematogenous dissemination [8]. Elevated levels of serum
glucose, iron, and ketone bodies increase fungal growth and
induce the expression of GRP78 and CotH, resulting in increased
ability of Rhizopus to invade host tissues and explaining the
susceptibility of diabetic and deferoxamine treated patients to
mucormycosis [8].
In India, Chakrabarti et al. have described an overall prevalence
of rhino-orbito-cerebral mucormycosis (48%), followed by
pulmonary mucormycosis (17%), gastrointestinal mucormycosis (13%), cutaneous mucormycosis (11%), renal and disseminated
mucormycosis (5% each) [4]. The MIC patterns observed with
the isolates of R. homothallicus were consistent with those
reported for other Rhizopus species with amphotericin B MIC
of 0.5 μg/ml [4]. This suggests that the first-line recommended
antifungal agent is liposomal Amb (L-Amb) or Amb lipid complex
(ABLC). ECMM/ESCMIDand ECIL-6 guidelines recommend the
use of L-Amb with a daily dosage of at least 5 mg/kg/day for
mucormycosis [9,10]. Recently, isavuconazole has been added to
the armamentarium of antifungal agents, however, its use has not
yet been specified in the most recent guidelines [9]. Management
of Invasive mucormycosis includes comprehensive approach like
antifungal therapy, surgery and control of underlying conditions
like reduction of immunosuppressive therapy in this case.
Conclusion
The purpose of this case report is to emphasise that R.
homothallicus, although a rare fungus, its differentiation is
important as it has major therapeutic implications. Mucormycosis
is a life-threatening fungal infection causing angioinvasion that
occurs mostly in immune-compromised patients and is associated
with an increasing incidence and mortality despite the availability
of therapeutic tools. Earlier diagnosis and optimal medicosurgical
treatment can improve survival and reduce morbidity.
Comparative studies are needed to better optimize induction and
consolidation treatment.
Acknowledgement
Authors thank Dr. Arunaloke Chakrabarti, Professor and In
Charge, Centre of Advance Research in Medical Mycology, WHO
collaborating Centre for Reference and Research of Fungi of
Medical Importance, National Culture Collection of pathogenic
Fungi and Head, Department of Medical Microbiology,
Postgraduate Institute of Medical Education and Research,
Chandigarh, for their kind help in the genomic sequencing of the
organism.
References
- Binder U, Maurer E, Lass-Flörl C (2014) Mucormycosis-from the pathogens to the disease. Clin Microbiol Infect 20: 60‐66.
- Pilmis B, Alanio A, Lortholary O, Lanternier F (2018) Recent advances in the understanding and management of mucormycosis. F1000Res 7: 1429.
- Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, et al. (2005) Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis 41: 634-653.
- Chakrabarti A, Marak RS, Shivaprakash MR, Sunita G, Rajiv G, et al. (2010) Cavitary pulmonary zygomycosis caused by Rhizopus homothallicus. J ClinMicrobiol 48: 1965‐1969.
- Kokkayil P, Pandey M, Agarwal R, Kale P, Singh G, et al. (2017) Rhizopus homothallicus Causing Invasive Infections: Series of Three Cases from a Single Centre in North India. Mycopathologia 182: 921‐926.
- Chander J, Kaur M, Singla N, Punia RS, Singhal SK, et al. (2018) Mucormycosis: Battle with the Deadly Enemy over a Five-Year Period in India. J Fungi (Basel) 4: 46.
- Compain F, Aït-Ammar N, Botterel F, Gibault L, Le Pimpec Barthes F, et al. (2017) Fatal Pulmonary Mucormycosis due to Rhizopus homothallicus. Mycopathologia 182: 907‐913.
- Baldin C, Ibrahim AS (2017) Molecular mechanisms of mucormycosis-The bitter and the sweet. PLoSPathog 13: e1006408.
- Tissot F, Agrawal S, Pagano L, Petrikkos G, Groll AH, et al. (2017) ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica 102: 433-444.
- Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, et al. (2014) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect 3: 5-26.