Keywords
Compliance; Surviving sepsis campaign guideline; Intensive care unit
Introduction
Sepsis is defined as a systemic, deleterious host response to infection leading to organ dysfunction and shock [1]. It can occur in the community and also in the health care setting. Around half of the cases of sepsis are due to pneumonia, followed by intraabdominal and urinary tract infections [2].
It is estimated that sepsis accounts for 2% of all hospitalizations in the United States (US) and it accounts for around 10% of all intensive care unit (ICU) admissions [2]. The incidence was estimated to be around 3 cases per 1000 population in the US [3]. Incidence increased >100 times with age (0.2/1000 in children to 26.2/1 000 in those above 85 years old) [3]. Incidence has been projected to rise 1.5% per year. Mortality rate was 28.6% and increased with age (10% in children to 38.4% in those above 85 years old) [3]. Therefore, sepsis places a significant burden on health care utilization and costs associated with hospitalization.
To overcome the high mortality associated with sepsis and the high burden on healthcare utilization and therefore, healthcare costs, the Surviving Sepsis Campaign, a collaboration between the European Society of Intensive Care Medicine, the Society of Critical Care Medicine and the International Sepsis Forum was formed in October 2002. The Campaign aimed to decrease the relative mortality of sepsis by 25% in the next five years and issued a consensus statement in 2004, the first Surviving Sepsis Campaign guideline [4]. Over the years, modifications have taken place which culminated in the third consensus statement published in 2012.
The concept of care bundles was developed [5] so as to improve the compliance to guidelines. Each care bundle consists of a few elements, in which each element is a specific intervention to patient care. The advantage of a care bundle is that all elements must be performed in all indicated patients, using the all-or-none approach. The third consensus statement is a protocol that guides the resuscitation of patients with sepsis induced tissue hypoperfusion. It should be initiated once hypoperfusion is identified and should not be delayed whilst awaiting ICU admission. It is divided into 2 sets of bundles of management. The first set aims to be completed within 3 h from the time of diagnosis of sepsis whilst the second set aims to be completed within 6 h [1].
Data on the local compliance rate to the Surviving Sepsis Campaign guideline are lacking. Since the nature of sepsis is reversible and is associated with a high mortality rate, a retrospective study was carried out to look at the epidemiology of local ICU patients diagnosed to have sepsis and the compliance rate with the bundles of management as set out in the Surviving Sepsis Campaign 2012 guideline.
Definitions
Patient’s demographics were defined as: Age and sex
Sepsis [6]: Life threatening organ dysfunction caused by a dysregulated host response to infection.
Organ dysfunction: An acute change in total Sequential Organ Failure Assessment (SOFA) scores ≥ 2 points consequent to the infection.
Septic shock: A subset of sepsis in which underlying circulatory and cellular metabolism abnormalities are profound enough to substantially increase mortality.
Clinical criteria to identify septic shock: Sepsis with persisting hypotension requiring vasopressors to maintain MAP ≥ 65 mm Hg and having a serum lactate >2 mmol/L despite adequate volume resuscitation.
Time zero: the time of diagnosis of sepsis. This is the time from which 3 h and 6 h will be counted to see whether the management of sepsis within this period was done according to the guideline. SOFA score at the time of diagnosis was measured.
Methodology
Study design
A retrospective study was done in the intensive care unit of Tseung Kwan O Hospital (TKOH), a secondary level care regional hospital in the New Territories of Hong Kong. The study was approved by the Research Ethics Committee of the Kowloon East Clusters of the Hospital Authority.
The ICU consists of 10 beds and there were 654 admissions in 2014. It admits patients from the following specialties: Medicine, surgery, orthopaedics and gynaecology.
All patients admitted to the ICU from 1st January, 2014 to 30th June, 2014 were identified through the ICU admissions records. Electronic records and handwritten records of all those patients were retrieved from the medical records department and were reviewed.
Inclusion criteria were: 1. Patients with SOFA score ≥ 2 points consequent to infection. Baseline SOFA score is assumed to be zero. 2. Eighteen years or older.
Those fulfilled inclusion criteria were then recruited into the study. All adult patients with sepsis (including those transferred from ICUs or hospitals and readmissions to the ICU during the current hospital stay) were included.
Data collection
Data on demographics; underlying medical conditions; principal diagnosis; clinical characteristics such as: SOFA score at the time of diagnosis of sepsis; source of infection; antibiotics used; whether blood culture was taken prior to antibiotic administration; type of intravenous fluids used; volume of intravenous fluids given within 3 h of diagnosis of sepsis; use of vasopressor if indicated; mortality of current hospital admission; time of attendance at the Accident & Emergency department; time of admission; time of diagnosis of sepsis; patients’ location upon diagnosis of sepsis, time of antibiotic administration; choices of antibiotics; time of ICU admission were gathered.
Measurement of outcomes
The primary outcome measures were the compliance with the 2 bundles of care in the Surviving Sepsis Campaign 2012 guideline. The secondary outcome measure was all cause mortality of the current hospitalization. Descriptive statistics were used and information was expressed in percentages in the form of pie charts or bar charts.
Results
Patient demographics
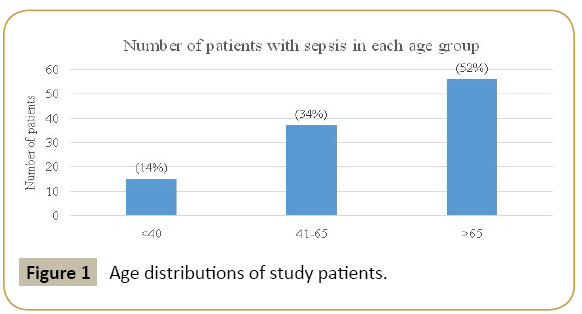
There were a total of 336 ICU admissions from 1st January, 2014 to 30th June, 2014, of which 108 (32.1%) patients were recruited into the study. In the study, 67 were male (62%) and 41 were female (38%). The mean age was 63.6 years. The youngest age group only accounted for 14% of those in the study and the percentage increased to 52% in oldest age group (Figure 1). The length of stay for all our patients was greater than 24 h.
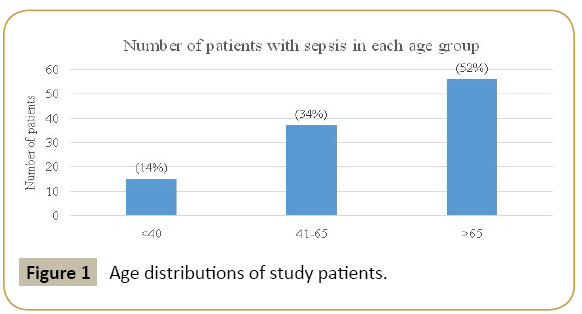
Figure 1: Age distributions of study patients.
Diagnosis of sepsis
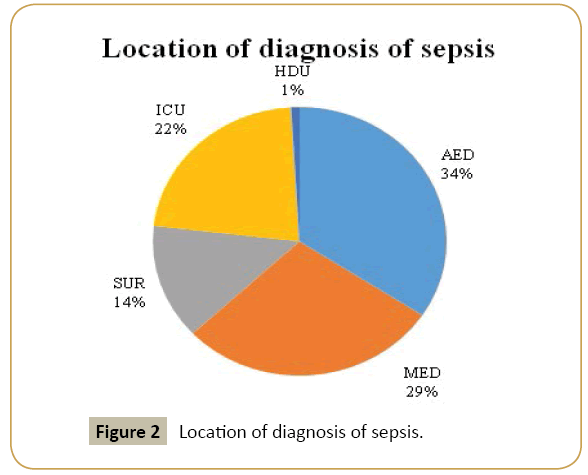
The majority (34%) of cases of sepsis was diagnosed at the Accident and Emergency department (AED), followed by 29% in medical ward (MED), 22% in ICU, 14% in surgical ward (SUR) and 1% in the high dependency unit (HDU) (Figure 2).
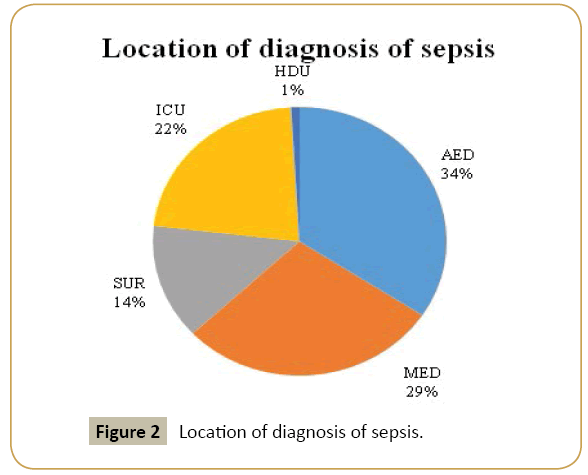
Figure 2: Location of diagnosis of sepsis.
There were 50/108 (46%) patients admitted to ICU<3 h after diagnosis of sepsis, 11/108 (10%) within 3-6 h after diagnosis of sepsis and 47/108 (44%) after 6 h of diagnosis.
Underlying medical conditions & source of infection
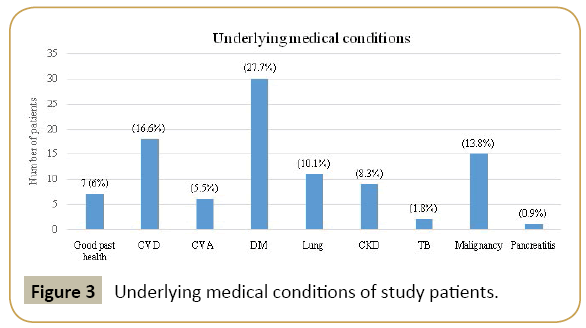
The most common medical condition was diabetes mellitus (DM) at 27.7%, followed by cardiovascular disease (CVD) at 16% and malignancy at 13.8%. Chronic kidney disease (CKD) made up of 8.3% whilst cerebrovascular accidents made up of 5.5% (Figure 3).
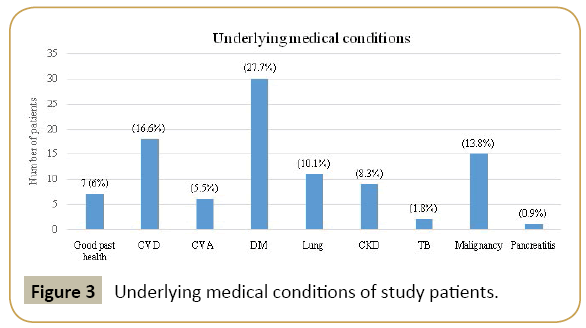
Figure 3: Underlying medical conditions of study patients.
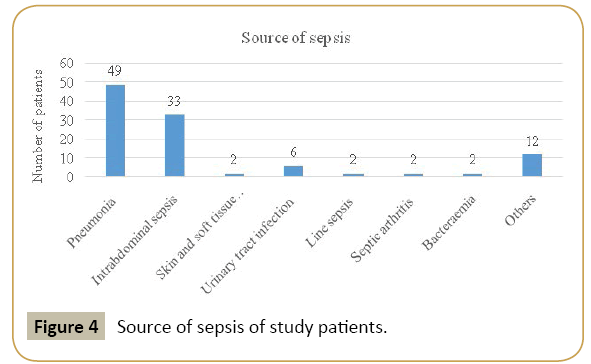
The majority (45%) of patients was diagnosed with pneumonia as the cause of sepsis with ICU admission. It was followed by intraabdominal sepsis (biliary sepsis, perforated viscus, peritonitis and acute appendicitis) at 31% and urinary tract infection at 6% (Figure 4)
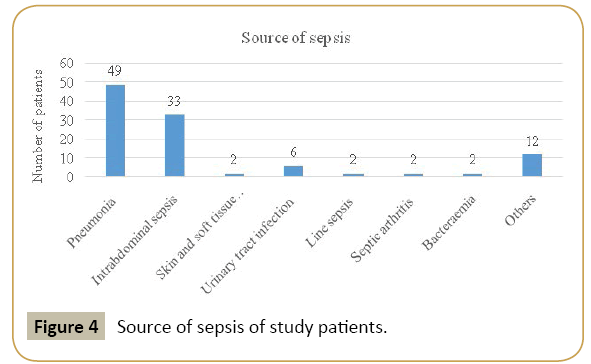
Figure 4: Source of sepsis of study patients.
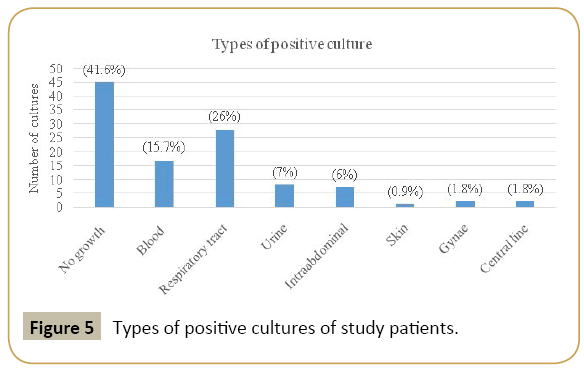
Most patients (41.6%) did not have any positive cultures. The commonest type of positive culture was from respiratory tract at 26% of patients which included sputum, nasopharyngeal aspirates and endotracheal aspirates. The second most common source of positive culture was blood at 15.7%, followed by intraabdominal (from bile or peritoneum) at 6% (Figure 5).
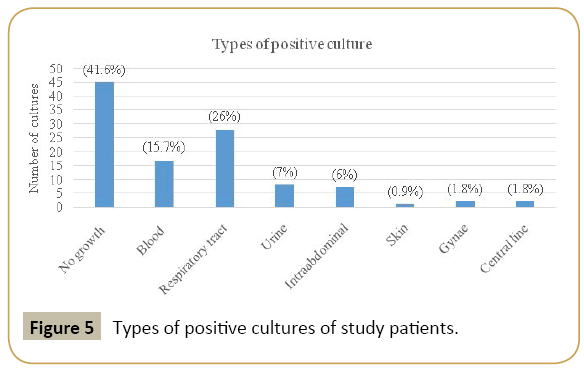
Figure 5: Types of positive cultures of study patients.
SOFA scores
SOFA scores at the time of diagnosis of infection ranged from 2 to 13. The average score was 7.67, median score was 8 and mode was also 8. Male patients had a SOFA score of 7.88 on average, whilst female patients had an average of 7.32. The youngest patients (<40 years old) had an average of 7.8, patients between 41 to 65 years old had an average of 7.51 whereas the oldest patient (>65 years old) had an average of 7.74. Patients who eventually died had an average SOFA score of 9.16 whilst those who survived had an average score of 7.05.
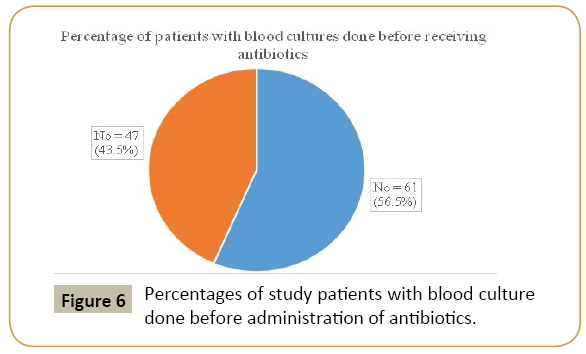
Three hour bundle
Compliance rate of lactate measurement was 0%. The compliance rate for blood cultures done before administering antibiotics was 56%. All patients had been administered antibiotics within the first 3 h and the compliance was 100% (Figure 6).
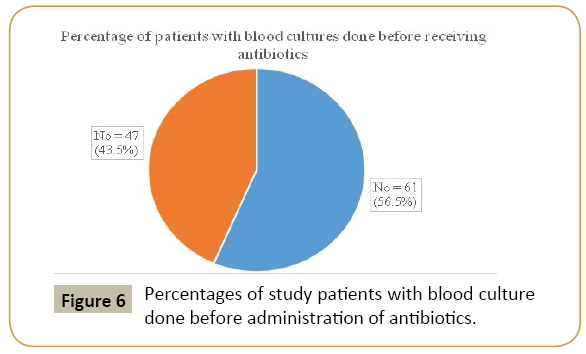
Figure 6: Percentages of study patients with blood culture done before administration of antibiotics.
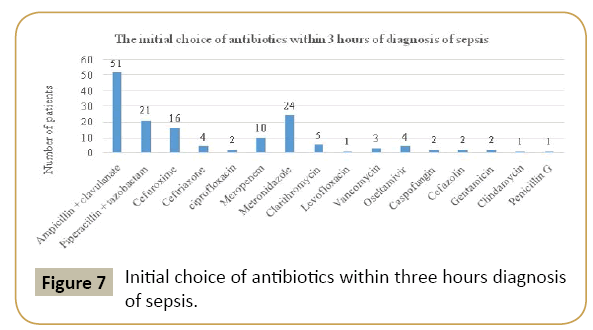
The initial antibiotic most commonly given on diagnosis of sepsis was amoxicillin & clavulanate to cover respiratory, urinary tract and intraabdominal infections. In case of intraabdominal infections, it was paired with metronidazole, which was the second most commonly used antibiotic. The third most common was piperacillin & tazobactam to cover suspected hospital acquired infections (Figure 7).
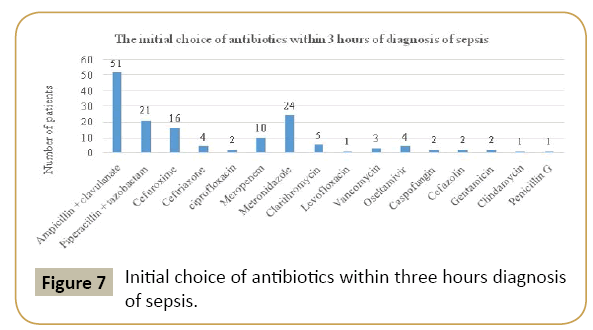
Figure 7: Initial choice of antibiotics within three hours diagnosis of sepsis.
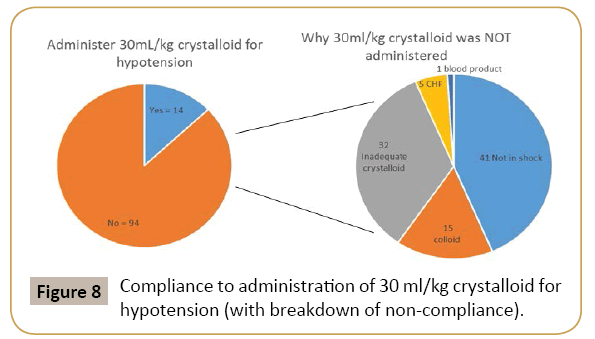
The three hour bundle advises to administer 30 mL/kg crystalloid for hypotension, to meet the therapeutic goal of MAP ≥ 65 mm Hg. There were 14/108 (12%) patients given adequate crystalloid fluid challenge, whilst 94/108 (87%) were not (Figure 8). Of those 94 not given adequate fluid challenge, 41/94 (43.6%) were not in shock and therefore by definition, not required fluid challenge. There were 15/94 (15.9%) given colloid instead of crystalloid, 32/94 (34%) given inadequate crystalloid, 5/94 (5.3%) with heart failure and therefore the volume of fluid given was decreased and 1/94 (1%) patient was given large volume blood product instead. Therefore, the compliance rate to 30 mL/kg crystalloid for hypotension was 14/(108-41)=14/67=21%.
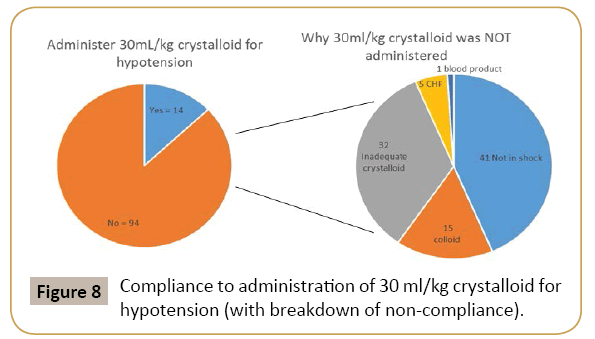
Figure 8: Compliance to administration of 30 ml/kg crystalloid for hypotension (with breakdown of non-compliance).
Six hour bundle
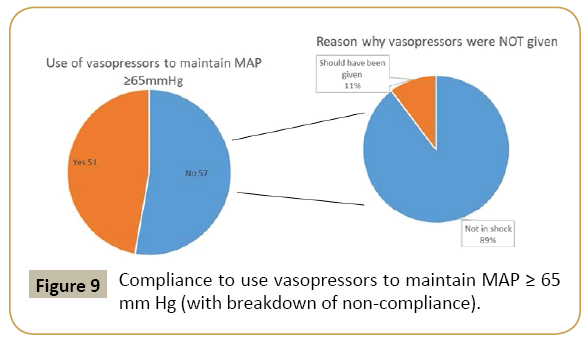
There were 51/108 (47%) of patients given vasopressors, whilst 57/108 (53%) were not. Of the 57 patients who were not given vasopressors, 51 (89%) were not in shock and 6 (11%) should have been given (Figure 9). Therefore, the compliance rate to the use of vasopressor was 51/(108-51)=51/57=89%.
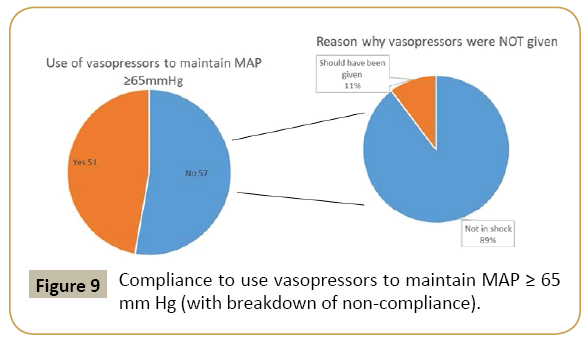
Figure 9: Compliance to use vasopressors to maintain MAP ≥ 65 mm Hg (with breakdown of non-compliance).
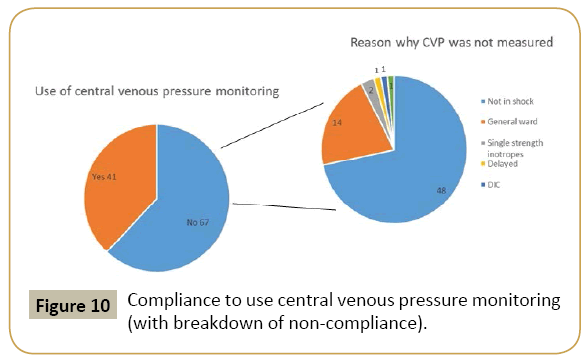
There were a total of 67/108 (62%) patients not given central venous pressure (CVP) monitoring. Of those 67 patients, 48 (71.6%) were not in shock, 14 (20.8%) were in the general wards, 2 (2.9%) were using single strength inotrope, 1 (1.4%) was delayed to have central line inserted, 1 (1.4%) had coagulopathy pending correction and 1 (1.4%) should have been monitored (Figure 10). Therefore, the compliance rate of CVP monitoring is 41/(108-48)=68%.
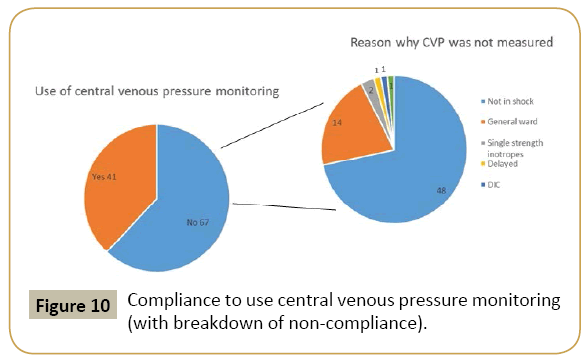
Figure 10: Compliance to use central venous pressure monitoring (with breakdown of non-compliance).
There were no measurement of central venous oxygen saturation and the compliance rate was 0%.
Comparison with other countries
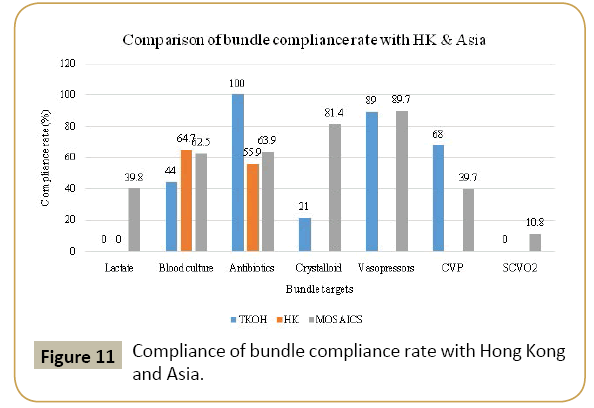
Our centre’s compliance rates are comparable or even exceed that of other Asian centres (MOSAICS trial) in antibiotic use, vasopressor use and CVP use. However, they fall below the level of other Asian centres regarding blood culture before antibiotics administration and crystalloid use (Figure 11).
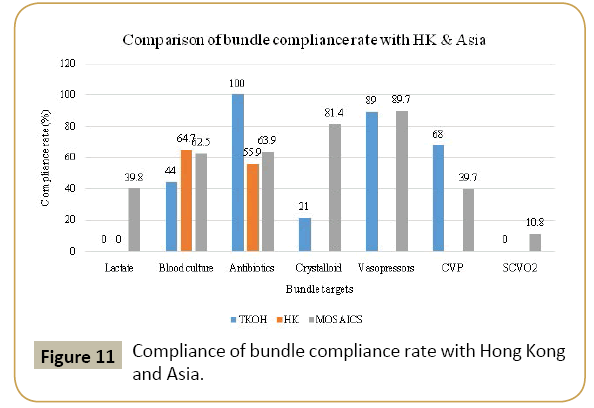
Figure 11: Compliance of bundle compliance rate with Hong Kong and Asia.
Mortality
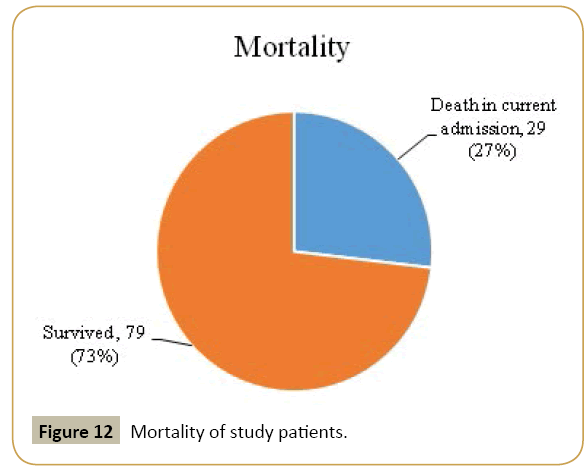
There were 29 patients who died in the current hospitalization of this study, which accounted for a 26.8% hospital mortality rate (Figure 12).
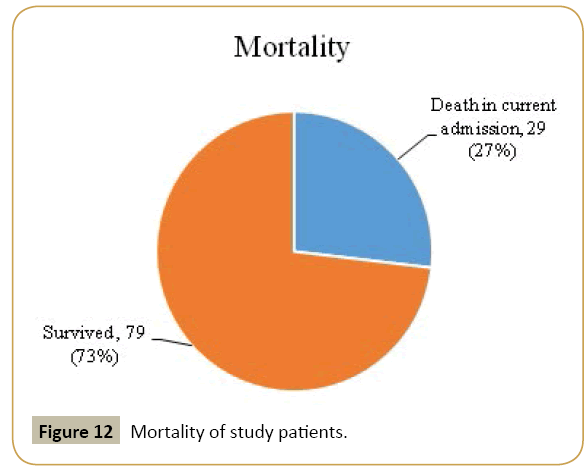
Figure 12: Mortality of study patients.
Discussion
Patient demographics
This study showed that the incidence of sepsis in ICU admissions was around 32% which was comparable to an international multicentre cohort study, with an incidence of sepsis of 32.3% in their long stay (greater than 24 h in ICU) group [7]. However, in a local, Hong Kong study, the incidence was 17.5% only [8]. In the United States [3] and also in Australia and New Zealand [9], the incidence was around 11%. This difference in incidence might be due to the different population and ICU admission criteria. Most of the patients in our study were male (62%), which was also comparable as the International cohort study had 61.6% male patients [7], whilst an Asian cohort study the MOSAICS trial had 61.7% males [10]. This observed male predominance can be explained because male sex is a risk factor for sepsis, probably related to differences in sex hormones [3,11]. In this study, the mean age of our patients was 63.6 years, which was slightly older than the MOSAICS cohort of 59.2 years [10] and was similar to the international cohort with a mean age of 64 years [7]. In this study, the number of patients in the >65years age group was about 3 times more than that in the <40 years age group. This is because old age is a risk factor and sepsis is more prevalent in the elderly [2].
Underlying medical conditions & source of infection
Risk of developing sepsis is dependent on both the patient’s underlying predisposition for infection and on the likelihood of developing acute organ dysfunction [2]. Hence, those who have an underlying immunocompromised state, such as: diabetes mellitus, long term immunosuppressants use or malignancy, are at an increased risk of sepsis, as are those with an underlying chronic organ failure [3]. Other risk factors include: low socioeconomic status, living in long term care facilities, malnutrition and use of prosthetic devices.
The five most common underlying medical conditions in this study were (in descending order): diabetes mellitus (27.7%), cardiovascular disease (16.6%), malignancy (13.8%), chronic lung disease (10.1%) and chronic kidney disease (8.3%). These findings are expected as sepsis is more likely to occur in the presence of chronic obstructive pulmonary disease (COPD), cancer, chronic kidney disease, chronic liver disease and diabetes mellitus [2].
The top three commonest causes of infection in this study are: pneumonia (45%), intraabdominal sepsis (31%) and urinary tract infection (6%), which are similar to the MOSAICS cohort at 37.4%, 21.1% and 8.5%, respectively [10]. These findings are also supported by a multicentre study (PROWESS-SHOCK) [12].
Sepsis and SOFA score
The clinical features of sepsis are a result of the host response to infection. The host response has two components: the proinflammatory and anti-inflammatory mechanisms that help to clear up the infection and lead to tissue recovery, but on the other hand, it can also cause organ damage and secondary infection [2] (Tables 1 and 2).
|
To be completed within 3 h:
1. Measure lactate level
2. Obtain blood cultures prior to administration of antibiotics
3. Administer broad spectrum antibiotics
4. Administer 30 ml/kg crystalloid for hypotension or lactate ≥ 4 mmol/L
To be completed within 6 h:
5. Apply vasopressors (for hypotension that does not respond to initial fluid resuscitation) to maintain a mean arterial pressure (MAP) ≥ 65 mm Hg.
6. In the event of persistent arterial hypotension despite volume resuscitation (septic shock) or initial lactate ≥ 4 mmol/L:
-Measure central venous pressure (CVP)*
-Measure central venous oxygen saturation (ScvO2)*
7. Remeasure lactate if initial lactate was elevated*
* Targets for quantitative resuscitation included in the guidelines are CVP of ≥ 8 mm Hg, ScvO2 of ≥ 70% and normalization of lactate.
|
Table 1: 2012 surviving sepsis campaign bundles [1].
1 Cardiovascular disease: Ischaemic heart disease, heart failure, atrial fibrillation.
2 Diabetes mellitus: Fasting blood glucose >7 mmol/L, 2 h OGTT value or random glucose >11.1 mmol/L or HbA1c>6.5.
3 Chronic lung disease: Asthma, chronic obstructive pulmonary disease.
4 Chronic kidney disease: Stage 5 chronic kidney disease (GFR<15 ml/min/1.73 m2) or requiring dialysis. |
Table 2: Definitions of different underlying medical conditions.
The clinical features of sepsis vary and depend on the underlying source of sepsis, presence of acute organ failure, underlying health condition of the patient and the time to initiation of treatment. The most commonly affected organ systems in sepsis leading to acute organ dysfunction or failure are cardiovascular and respiratory systems. To assess the degree of organ dysfunction, sequential organ failure assessment (SOFA) score, which is based on 6 organ systems (cardiovascular, respiratory, renal, liver, neurological and haematological), should be employed. This score can predict mortality risk of ICU patients as well. Furthermore, lactate is a useful indicator of tissue hypoperfusion as it becomes elevated when the circulatory system is compromised.
The acute change of SOFA scores for patients in our study ranged from 2 to 13, indicating a wide spectrum of the severity of organ dysfunction. It is reasonable to observe that those who died of sepsis had greater change of SOFA score (9.16 versus 7.05), signifying more severe organ dysfunction was related to mortality. There were no significant difference in acute change of SOFA score between different sex and age. The time of transition from clinical stability to organ dysfunction, the ‘golden hours’, can be in the emergency department [13], general ward [14] or ICU [15] and requires early recognition and active intervention to prevent sepsis related mortality. ‘Golden hours’ may be picked up outside intensive care unit with the use of quick-SOFA score, which identifies patients with suspected sepsis who are at greater risk for a poor outcome. It consists of three criteria, assigning one point for low blood pressure (SBP ≤ 100 mm Hg), high respiratory rate (≥ 22 breaths/min) or altered mental state (Glasgow coma scale <15). This score can be incorporated into the patient observation chart in general wards. Critical care physicians will be alerted to promptly assess septic patients when quick-SOFA score is two points or more. Recommendations on clinical management can be made and early transfer to intensive care unit may also be initiated.
One crucial factor in the treatment of sepsis is the administration of antibiotics to target the underlying cause of infection. The choice of antibiotics depends on the source of infection, local antibiotic resistance patterns and most importantly, the organism itself. Hence, cultures of the involved infected organ system as well as blood culture should be taken before antibiotic administration. This is why blood culture taken before antibiotic administration within 3 h of diagnosis of sepsis is included in the Surviving Sepsis Campaign guideline. However, it is known that blood cultures are only positive in around one third of samples [13] and that up to one third of all patients will have cultures from all sites to be negative [16]. This is reflected in our study by the finding of 41% of patients having no growth from all culture sites. Of all the positive culture samples, the respiratory tract was the most common source at 26%, followed by blood at 15.7%, urine at 7% and intraabdominal at 6%.
Three hour bundle
In times of poor perfusion such as septic shock, anaerobic respiration occurs which would lead to lactate production [17,18]. The use of lactate can aid in the diagnosis of septic shock, as an elevated lactate level in blood can be an indication of sepsis induced tissue hypoperfusion or organ dysfunction. One study showed that lactate >4 mmol/L was related to higher mortality [19]. Therefore, serum lactate is a universal measurement of tissue perfusion for patients with sepsis and is useful for estimation of prognosis. Elevated lactate in blood would warrant aggressive resuscitation to improve survival. The compliance with lactate measurement in our study was 0% whereas the compliance rate was 39.8% in MOSAICS [10]. Hence there is immediate need to promulgate the use of serum lactate in the management of patients with sepsis through various means such as training, education and simulation workshops. Currently, serum lactate is increasingly measured and utilized in our centre and other intensive care units in Hong Kong.
The compliance rate for blood cultures done before administering antibiotics was 56% in this study, which is similar to the MOSAICS cohort of 62.5% [10]. The importance of timely blood culture taking prior to antibiotic administration needs to be stressed to ensure early and correct identification of the organism causing infection, as well as improving the yield since only one third of blood cultures will be positive [13].
The compliance rate to broad spectrum antibiotics administration within 3 h of diagnosis of sepsis was 100% in this study as compared to 63.9% in MOSAICS [10]. Broad spectrum antibiotics usage is necessary to cover both gram positive and gram negative bacteria. The most common gram positive culture isolates are Staphylococcus aureus and Streptococcus pneumoniae, whereas the gram negative culture isolates are Escherichia coli, Klebsiella species and Pseudomonas aeruginosa [13,16]. In an international study involving ICU centres in 75 countries, around 62% of patients had gram negative bacteria isolated from their cultures. In this study, 78% of the patients were diagnosed to have sepsis outside ICU and the majority was in the emergency department (34%). Since pneumonia is the most common cause of sepsis, their underlying source of infection is likely to be community acquired pneumonia. Therefore, amoxicillin & clavulanate as an initial choice of antibiotic is appropriate as it has strength in covering both gram positive and gram negative bacteria.
Many barriers exist in ensuring timely ordering of blood culture and early initiation of antibiotics. Firstly, clinicians’ awareness and familiarity of the guidelines will affect the compliance [20]. Secondly, in our centre, antibiotics are not readily available in the wards, as they are kept in the pharmacy and there is a lag time from ordering the antibiotic to availability to the patient. The time may also be lengthened during non-office hours.
One way to combat these barriers is through collaboration between the emergency department and ICU by the use of early goal directed therapy (EGDT) protocol. EGDT has been shown to decrease mortality in patients with sepsis and septic shock [21]. EGDT is a protocol that consists of interventions very similar to those found in the 3rd Surviving Sepsis Campaign guideline and comprises of CVP monitoring, crystalloid fluid challenge, vasopressor use, ScvO2 monitoring and transfusion of red cells. Through collaboration between the emergency department and ICU, the targets of EGDT were achieved within a median time of less than 6 h from diagnosis of sepsis [22].
Fluid challenge with crystalloid to 30 ml/kg to reach a target of MAP ≥ 65mm Hg is recommended [1]. The compliance to adequate fluid challenge with crystalloid was 21% in our study. In those indicated for fluid challenge (as they were in shock) but were not given to the target of 30 ml/kg was due to: crystalloids not given sufficiently according to 30 ml/kg (in fact, most patients only received about 20 ml/kg), giving colloid instead of crystalloid, underlying heart failure and giving blood products. The compliance rate in MOSAICS was 81.4% [10]. One of the difficulties of achieving this target requires early identification of hypotension to initiate fluid challenge. Most patients in our study were diagnosed in the acute general medical wards, surgical wards or emergency department, where the intensive monitoring of hourly blood pressure was unfeasible. Secondly, vasopressors tend to be started before adequate fluid resuscitation had been achieved, especially in those with a history of heart failure or those with high CVP (>8 cm H2O).
Close monitoring of response to fluid challenge as well as end organ perfusion are important. Even if vasopressors had been started, further fluid challenge could be given to decrease the amount of vasopressor used.
Six hour bundle
The 6 h bundle involves application of vasopressor if persistent hypotension despite adequate crystalloid fluid challenge to a target of MAP ≥ 65mm Hg. In case of persistent hypotension or the presence of elevated lactate (found in the 3 h bundle), then CVP measurement and also central venous oxygen saturation (ScvO2) should be measured.
The compliance rate in our study to the use of vasopressor was 89%, which is similar to MOSAICS of 89.7% [10]. There were 6 patients indicated to have vasopressors, but were not given. Again, the timely recognition of hypotension with intensive monitoring of blood pressure is advisable.
The most commonly used vasopressor was dopamine, as compared with the recommended first line use of noradrenaline in the Surviving Sepsis Campaign guideline [1]. This might be due to the lower cost of dopamine and does not require administration through a central venous catheter. Therefore, dopamine was usually initiated in the general wards and then switched to noradrenaline after transfer to ICU when a central line had been inserted for CVP monitoring as well as for noradrenaline infusion. The dosage of vasopressor used was titrated individually, as the optimal mean arterial pressure would be higher in those with underlying hypertension than in the young without cardiovascular risk factors or comorbidities [23].
The compliance rate of CVP monitoring was 68% in this study and was 39.7% in MOSAICS [10]. The majority of the patients did not have CVP monitoring even when indicated because they were in the general wards. In the general ward setting, CVP measurement and monitoring is not commonly done as greater manpower is required for insertion and caring. Secondly, setting up central venous catheter during emergency or sepsis could be difficult due to collapsed veins. Thirdly, CVP is not associated with circulating blood volume, nor does it predict fluid responsiveness in a wide variety of clinical conditions [24]. Also, the CVP is not an accurate reflection of the preload, as it is affected by intrathoracic pressure and cardiac conditions. The CVP becomes persistently high in those with elevated intrathoracic pressure such as with the use of high positive end expiratory pressure in mechanical ventilation [23]. Also, the CVP would be raised when there is increased intraabdominal pressure [23]. Therefore, newer parameters such as the stroke volume variation [25] and the pulse pressure variation [26] are now considered a more accurate reflection of the fluid responsiveness in mechanically ventilated patients as compared to CVP monitoring.
ScvO2 measurement was not done in our study. The compliance rate of MOSAICS was 10.8% [10]. The ScvO2 is a measurement of the saturation of the venous blood, done by fiber-optic central venous catheter inserted into the superior vena cava. It is used to indicate oxygenation at a cellular level [27]. A saturation of 60-80% suggests adequate perfusion. ScvO2 was first found to have a survival benefit as one of the end points in early goal directed therapy [21]. Mortality was lowered only in the patients with normal value of maximal ScvO2 (70-89%) within the first 6 h of initial resuscitation [28]. However, treatment to normalize lactate was non-inferior to the treatment to normalize ScvO2 in a randomized control trial [29]. Currently, there is insufficient evidence to show improved outcomes over good clinical judgment and therefore, ScvO2 measurement is not widely practiced in intensive care units in Hong Kong.
Mortality
The hospital mortality rate of the study was 26.8%, which is lower than 44.5% in MOSAICS [10]. However, the causes of this difference in mortality rate are multi-factorial, such as differences in the underlying co-morbidities of ICU patients, demographics, ICU resources and physicians’ compliance to the guideline, etc. There are still many confounding factors which warrant further research.
Studies have shown that there are multiple factors associated with improved survival such as compliance with the bundle target of blood culture before antibiotics [10] and early administration of broad spectrum antibiotics [10]. Factors found to have greater compliance to the bundles and therefore, indirectly decreased mortality included high income countries, university hospitals, ICUs with an accredited fellowship programme and surgical ICUs [10].
A French study which followed an older Surviving Sepsis Campaign guideline showed that by improving the compliance to 100% in 9 out of 10 interventions in the bundles, the 28 day mortality rate decreased from 40% to 27% [30]. An international survey done by the Surviving Sepsis Campaign showed a reduction in mortality from 37% to 30.5% when compliance with the bundles increased [31]. A third study in England showed that compliance with the 6 h bundle reduced mortality from 49% to 23% [32].
A Croatian study showed that the following risk factors increased mortality in ICU: Sepsis acquired at another department, winter season, limited mobility, ICU length of stay, SOFA score on day 1, history of heart failure, chronic obstructive pulmonary disease, septic shock during ICU treatment and negative blood culture on admission [33]. It also found that those treated with adequate empirical antibiotics improved survival.
Revised sepsis care bundle
Minor change in the 6 h bundle was adopted in 2015 by Surviving Sepsis Campaign Executive Committee. In the 2012 bundle, measurements of central venous pressure (CVP) and central venous oxygen saturation (ScvO2) are advocated in the event of persistent arterial hypotension despite volume resuscitation. Now either repeated focused examination including vital signs, cardiopulmonary status, capillary refill, pulse and skin findings or two of the following (CVP measurement, ScvO2 measurement, bedside echocardiogram & dynamic assessment of fluid responsiveness with passive leg raise or fluid challenge) is recommended in the latest care bundle.
Limitations and Strengths
This study is a retrospective study looking into a highly selected group of critically ill patients admitted to the ICU. Study patients were restricted to one local hospital, which would not be a true reflection of territory wide practice and therefore the generalizability of study is limited.
One of the strengths of this study was the first epidemiological study on patients with sepsis admitted to ICU that was done in Hong Kong using Surviving Sepsis Campaign guideline.
Implications
This study showed that compliances with lactate measurement and early blood culture prior to initiation of antibiotics were suboptimal. More than half of the patients in our study were not diagnosed in ICU, where there would be more barriers to the adherence of the guideline.
Firstly, what are the reasons of poor adherence? There are many factors, such as: failure to recognize sepsis, lack of awareness or familiarity towards the sepsis guideline, lack of agreement to a specific item in the guideline or to the guideline in general as well as lack of motivation [34] and lack of time and staff in resource tight areas. Two audit reports were done in England to assess the effectiveness of the interventions aiming to improve sepsis guideline adherence in the acute medical unit.
The first audit report [35] identified two problems: 1) healthcare professionals had a lack of understanding towards sepsis and its management and 2) the time taken to collect all the equipments required to complete the Sepsis 6 bundle was long. Sepsis 6 involves: 1) deliver high flow oxygen, 2) take cultures from blood and other sites, 3) administer empirical intravenous (IV) antibiotics, 4) measure serum lactate, 5) start IV fluid resuscitation using crystalloid and 6) start urine output monitoring. The recommended interventions included setting up sepsis boxes containing all the equipments to manage a septic patient (including intravenous fluids, devices for blood taking and intravenous medication, etc.), teaching sessions for nurses, posters in the wards, straightforward guidelines to follow Sepsis 6 [36] and informing the doctors about the sepsis pathway.
The second audit report [37] focused more heavily on the education of junior doctors and the creation of work group. The belief was that junior doctors tend to work across wards and specialties and so they could help spread the message of the early recognition and management of sepsis. Again, the Sepsis 6 was used instead of the Surviving Sepsis Campaign guideline.
Secondly, can it be done? Both audit results had shown improvement in the uptake of the guideline in the acute medical ward. Furthermore, collaboration with the emergency department by the immediate implementation of EGDT once sepsis was diagnosed has been shown possible [22].
After this study was completed, a journal club in the Department of Medicine of TKOH was held to discuss on the findings and to educate all doctors in the department about the early recognition and timely management of sepsis. Other areas of improvement could be collaboration with the emergency department, providing prompt measurement of serum lactate level and easier access to antibiotics especially in non-office hours.
Future study to look into the clinical outcomes and compliance with revised sepsis care bundle of septic patient will be performed after the implementation of these measures. Results of this retrospective study undoubtedly serve a baseline to demonstrate the effectiveness of these measures, adherence to the bundle and possible improvement in the survival of patients with sepsis.
Conclusion
Sepsis accounts for high mortality and morbidity, especially in the critically ill. Early recognition is of utmost importance, as it is a highly reversible and treatable condition when treatment is commenced early. Compliance to the Surviving Sepsis Campaign guideline has been shown to improve survival.
This study is the first in Hong Kong to look at compliance with the Surviving Sepsis Campaign guidelines. Relentless effort should be paid to update our knowledge on sepsis and more needs to be done to improve adherence to latest guidelines, particularly to the measurement of serum lactate level, prompt administration of antibiotic and source control, so that the mortality and morbidity of patients with sepsis can be reduced.
References
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, et al. (2013) Surviving sepsis campaign guidelines committee including the pediatric subgroup. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41: 2.
- Angus DC, van der PT (2013) Severe sepsis and septic shock. N Engl J Med 369: 840-851.
- Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, et al. (2001) Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome and associated costs of care. Crit Care Med 29: 1303-1310.
- Elizabeth S, Pritpal ST, Jean-Louis V (2003) The surviving sepsis campaign: Raising awareness to reduce mortality. Crit Care 7: 1-2.
- Resar R, Griffin FA, Haraden C, Nolan TW (2012) Using care bundles to improve health care quality. IHI Innovation Series White Paper.
- Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, et al. (2016) The third international consensus definitions for sepsis and septic shock (Sepsis 3). JAMA 315: 801-810.
- Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, et al. (2002) Epidemiology of sepsis and infection in ICU patients from an international multi-centre cohort study. Intensive Care Med 28: 108-121.
- Lam KN (2012) Management of severe sepsis in patients admitted to intensive care units in Hong Kong, focus on early blood culture taking and starting of antibiotics.
- Finfer S, Bellomo R, Lipman J, French C, Dobb G, et al. (2004) Adult population incidence of severe sepsis in Australian and New Zealand intensive care units. Intensive Care Med 30: 586-596.
- Phua J, Koh Y, Du B, Tang YQ, Divatia JV, et al. (2011) MOSAICS Study Group. Management of severe sepsis in patients admitted to Asian intensive care units: Prospective cohort study. BMJ 342: d3245.
- Mayr FB, Yende S, Linde-Zwirble WT, Peck-Palmer OM, Barnato AE, et al. (2010) Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA 303: 2495-2503.
- Ranieri VM, Thompson BT, Barie PS, Dhainaut JF, Douglas IS, et al. (2012) Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med 366: 2055-2064.
- Nguyen HB, Rivers EP, Havstad S, Knoblich B, Ressler JA, et al. (2000) Critical care in the emergency department: A physiological assessment and outcome evaluation. Acad Emerg Med 7: 354-361.
- Lundberg JS, Perl TM, Wiblin T, Costigan MD, Dawson J, et al. (1998) Septic shock: An analysis of outcomes for patients with onset on hospital wards versus intensive care units. Crit Care Med 26: 1020-1024.
- Lefrant JY, Muller L, Bruelle P, Pandolfi JL, L'Hermite J, et al. (2000) Insertion time of the pulmonary artery catheter in critically ill patients. Crit Care Med 28: 355-359.
- Opal SM, Garber GE, LaRosa SP, Maki DG, Freebairn RC, et al. (2003) Systemic host responses in severe sepsis analyzed by causative microorganism and treatment effects of drotrecogin alfa (activated). Clin Infect Dis 37: 50-58.
- Peretz DI, Mcgregor M, Dossetor JB (1964) Lactic acidosis: A clinically significant aspect of shock. CMAJ 90: 11.
- Broder G, Weil MH (1964) Excess lactate: An index of reversibility of shock in human patients. Science 143: 1457-1459.
- Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, et al. (2009) Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med 37: 1670-1677.
- Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, et al. (1999) Why don't physicians follow clinical practice guidelines? JAMA 282: 1458-1465.
- Emanuel R, Bryant N, Suzanne H, Julie R, Alexandria M, et al. (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345: 1368-1377.
- Trzeciak S, Dellinger RP, Abate NL, Cowan RM, Stauss M, et al. (2006) A 1 year experience with implementing early goal directed therapy for septic shock in the emergency department. Chest 129: 225-232.
- Vandervelden S, Malbrain ML (2015) Initial resuscitation from severe sepsis: One size does not fit all. Anaesthesiol Intensive Ther 47: s44-s55.
- Marik PE, Baram M, Vahid B (2008) Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the take of seven mares. Chest 134: 172-178.
- Zhang Z, Lu B, Sheng X, Jin N (2011) Accuracy of stroke volume variation in predicting fluid responsiveness: A systematic review and meta-analysis. J Anesth 25: 904-916.
- Yang X, Du B (2014) Does pulse pressure variation predict fluid responsiveness in critically ill patients? A systematic review and meta-analysis. Crit Care 18: 650.
- Wittayachamnankul B, Chentanakij B, Sruamsiri K, Chattipakorn N (2016) The role of central venous oxygen saturation, blood lactate and central venous-to-arterial carbon dioxide partial pressure difference as a goal and prognosis of sepsis treatment. J Crit Care. 36: 223-229.
- Pope JV, Jones AE, Gaieski DF, Arnold RC, Trzeciak S, et al. (2010) Emergency medicine shock research network (EMShockNet) investigators. Multicenter study of central venous oxygen saturation (SCVO2) as a predictor of mortality in patients with sepsis. Ann Emerg Med 55: 40-46.
- Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, et al. (2010) Emergency medicine shock research network (EMShockNet) investigators. Lactate clearance vs. central venous oxygen saturation as goals of early sepsis therapy: A randomized clinical trial. JAMA 303: 739-746.
- Lefrant JY, Muller L, Raillard A, Jung B, Beaudroit L, et al. (2010) Reduction of the severe sepsis or septic shock associated mortality by reinforcement of the recommendations bundle: A multicenter study. Ann Fr Anesth Reanim 29: 621-628.
- Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, et al. (2010) The surviving sepsis campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med 38: 367-374.
- Fang G, Teresa M, Darren FD, Simon G, Samantha F (2005) The impact of compliance with 6 h and 24 h sepsis bundles on hospital mortality in patients with severe sepsis: A prospective observational study. Crit Care 9: R764-R770.
- Degoricija V, Sharma M, Legac A, Gradiser M, Sefer S, et al. (2006) Survival analysis of 314 episodes of sepsis in medical intensive care unit in university hospital: Impact of intensive care unit performance and antimicrobial therapy. Croat Med J 47: 385-397.
- Niranjan K (2014) Sepsis guideline implementation: Benefits, pitfalls and possible solutions. Crit Care 18: 207.
- Sumitra K, Navdeep N (2014) Improving management of severe sepsis and uptake of sepsis resuscitation bundle in an acute setting. BMJ Qual Improv Rep.
- Daniels R, Nutbeam T, McNamara G, Galvin C (2011) The sepsis six and the severe sepsis resuscitation bundle: A prospective observational cohort study. Emer Med J 28: 507-512.
- Adcroft L (2014) Improving sepsis management in the acute admissions unit. BMJ Qual Improv Rep.