Commentary - (2023) Volume 7, Issue 2
A Survey of Nutrition Governance
Leila Aweis*
Department of Oncology, Kampala International University, Uganda
*Correspondence:
Leila Aweis,
Department of Oncology, Kampala International University,
Uganda,
Email:
Received: 30-May-2023, Manuscript No. ipjfnph-23-16807;
Editor assigned: 01-Jun-2023, Pre QC No. ipjfnph-23-16807 (PQ);
Reviewed: 15-Jun-2023, QC No. ipjfnph-23-16807;
Revised: 20-Jun-2023, Manuscript No. ipjfnph-23-16807 (R);
Published:
27-Jun-2023, DOI: 10.21767/2577-0586.7.02.16
Description
Hunger remains a common problem for individuals with malignant
growth and generally has poor clinical outcomes. Hunger
due to malignant growth is associated with decreased treatment
resistance, increased fatigue and mortality, decreased
stamina, and increased health care costs. Related to A set of evidence-
based and documented rules has evolved outlining the
best possible nutritional care for sick patients. The rule points
to the importance of screening for hunger risk, early assessment,
and treatment with clinical nutritional interventions to
prevent under nutrition and improve personal well-being and
outcomes for individuals with malignant growth. Current regulations
focus primarily on nutritional care provided in critical
care hospital settings, with little mention of systems for monitoring
ailing health in the survival stage of malignant growth.
Evidence suggests that the cost of caring for malnourished patients
in the field is more than double the cost of caring for fully
fed patients, and management of malignant growth disease
beyond the walls of the emergency department.
Evidence-based rules for monitoring under nutrition across
patient populations should be identified during recovery, key
considerations, and local settings to identify hunger risks and
work to enable appropriate nutritional care. It suggests that
regular fault screening should be done at Some of these regulations
focus on characterizing the profession of health care professionals,
such as general practitioners (GPs), and important
considerations for health care workers and nutritionists when
monitoring health deficiencies in the community. They emphasized
the critical role of primary care physicians, primary health
care providers, and community well-being partner clinicians in
assessing hunger risk and referencing dieticians for patients at
risk of health food shortages. The Canadian inventory of equipment
to detect, screen and treat malnutrition in critical care
settings also relates to discharge from clinics, the importance
of discharging and referring malnourished patients to local physicians. The number of individuals developing the disease
is increasing, making it increasingly difficult for intensive oncology
management to provide comprehensive follow-up care
to all malignant growth survivors. This has increased the need
to address patient survival care needs in the field. Sharing key
considerations and nutritional care with local governments is a
fundamental step to improve coordination and collaboration of
care after disease treatment is completed. The use of survivor
or shared care plans has been suggested to achieve this sharing
of care. Survivor care plans have been shown to work by acknowledging
information about the survivor’s medical history,
suggested findings, and possible late and long-term sequelae
as important professional considerations. Work related to the
exchange of nutritional care from clinical malignant growth
management to critical considerations and local management
should be fully consolidated to aid in the elucidation of specific
management improvements, in addition to further research.
In Australia, the administration of primary care and community
nutrition is intertwined with five public quality standards covering
different parts of the sector. The recently published Public
Welfare and Health Care Quality Principles support routine
gambling testing requirements in both key regions and regions,
but contain specific nutritional standards for public safety and
health care quality (NSQHS) criteria only. The NSQHS Nutrition
and Fluids Standards describe the importance of routine health
risk assessment, nutritional assessment, and management of
at-risk individuals, and serve as a coordinated regional recreational
focal point within health care.
Acknowledgement
Authors do not have acknowledgment currently.
Conflict Of Interest
There are no conflicts of interest.
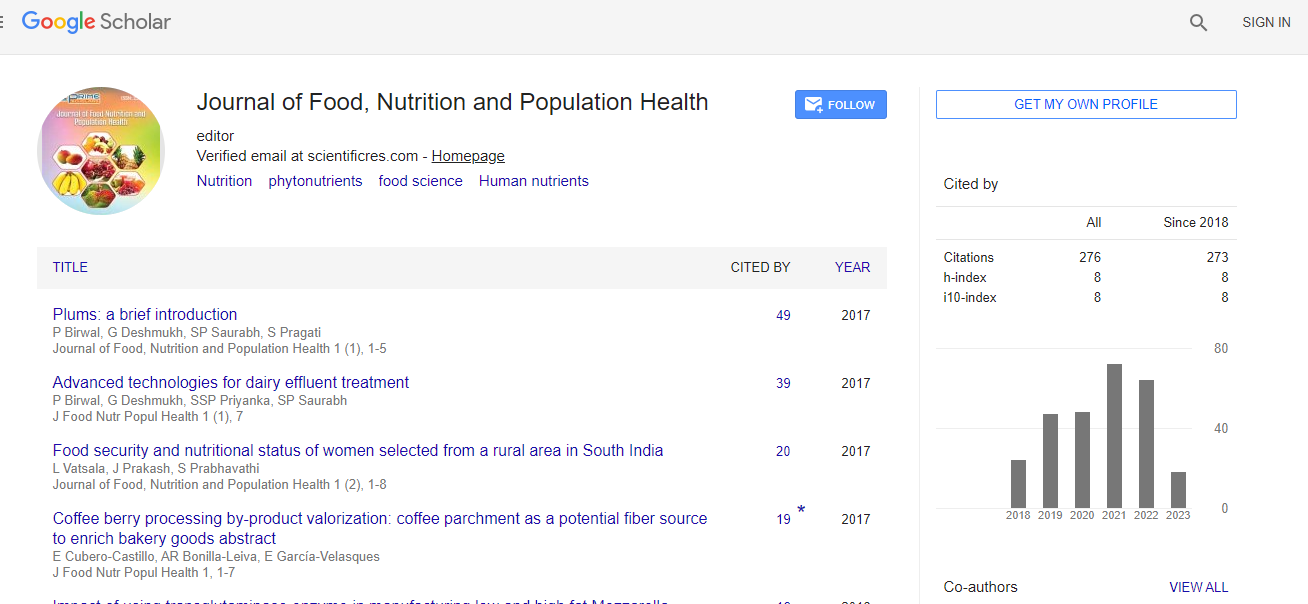
Citation: Aweis L (2023) A Survey of Nutrition Governance. J Food Nutr Popul Health. 7:16
Copyright: © 2023 Aweis L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.