Original Article - (2021) Volume 22, Issue 1
Johann Faizal Khan1, Suryati Mokhtar1, Krishnan Raman1, Harjit Singh1, Leow Voon Meng2,3, Manisekar K Subramaniam1,2
1Department of Hepatopancreatobiliary Surgery and Liver Transplantation, Selayang Hospital, Selangor, Malaysia
2Department of General Surgery, Division of Hepatopancreatobiliary Surgery, Sultanah Bahiyah Hospital, Kedah, Malaysia
3Advanced Medical and Dental Institute (AMDI), Science University of Malaysia (USM), Penang, Malaysia
Received Date: December 10th, 2020; Accepted Date: January 28th, 2020
Objective To identify trends in management and analyse outcomes of patients undergoing interventions for infected pancreatic necrosis with specific reference to factors predictive of mortality. Method A cross sectional study of patients undergoing intervention for IPN between 2009-2018 were performed at two of the largest hepatopancreatobiliary centres in Malaysia. Final outcome measure of complete resolution was compared against mortality (D). Head to head comparison of percutaneous catheter drainage alone versus Videoscopic Assisted Retroperitoneal Debridement was performed based on final predictive factor on mortality. Results A total number of 65 patients with IPN were identified. Data from 59/65 patients were analysed for final outcome of death (D) versus complete resolution. 6 patients were omitted due to incomplete data precluding proper analysis. Overall mortality rate was 25% (15/59 patients). 8 patients had no interventions performed but were included in the analysis. Percutaneous catheter drainage alone and Videoscopic Assisted Retroperitoneal Debridement were the 2 commonest interventions performed (34/55). Multivariable analysis predictive of mortality included persistent organ failure requiring intensive care unit (ICU) admission (OR= 336.425, CI 95% =3.722-999.999 p value= 0.0113) and when PCD alone was employed compared to VARD (OR = 48.923, CI 95% = 1.888-999.999, p-value = 0.019). Conclusion Our present study shows that both persistent organ failure requiring ICU admission and Percutaneous Catheter Drainage alone when compared to a minimally invasive step up approach (in the form of Video assisted Retroperitoneal Debridement) are predictive factors of mortality in patients undergoing intervention for IPN. A step up approach is necessary to prevent mortality in patients with infected pancreatic necrosis requiring intervention while PCD without debridement results in significant mortality.
Severe Acute Pancreatitis, Infected Pancreatic Necrosis, Step-up approach, Outcome, Videoscopic assisted retroperitoneal debridement, Percutaneous Catheter Drainage
CR complete resolution; IPN infected pancreatic necrosis; PCD percutaneous catheter drainage; VARD videoscopic assisted retroperitoneal debridement
Acute pancreatitis (AP) results in an overall mortality rate of 7.5% in Malaysia [1]. Moderately severe and severe pancreatitis may result in the development of pancreatic and or peripancreatic necrosis [2]. The pancreatic necrosis may be sterile or infected. Patients may be relatively well or may have persistent organ failure. INP in the absence of persistent organ failure results in mortality rates ranging between 6-11% [3, 4]. Risk of mortality doubles with persistant organ failure [5]. Unfortunately organ failure persisting more than 48 hours is present in 50% of patients with NP and approximately two thirds of patients with INP. The crucial determining factor in management should be whether the necrosis is sterile or infected, the patient symptomatic or not, and the nature of the necrosis. In general treatment should be aimed at patients who are symptomatic and with suspected or proven infection. 2 types of necrotic collections are present, notably Acute Necrotic Collections (ANC) and Walled-Off Necrosis (WON). In general ANC require drainage while WON may require a “step-up” to formal debridement. Intervention for NP can be divided broadly into the following: 1. Catheter based therapy 2. Endoscopic management 3. Combination of both-dual modality and 4. Open surgical debridement [6]. Historically, open surgical debridement was considered the goal standard and perhaps the only option of treatment prior to the minimally invasive era of management. Although the landmark PANTER trial paved the way for a more minimally invasive approach towards necrosectomy, there are many studies performed which have questioned the actual need for a formal necrosectomy. A systemic review revealed that Percutaneous Catheter Drainage (PCD) alone was able to obviate the need for further therapy in 56.2% of patients [7, 8]. Successful outcome depends on appropriate type and timing of intervention [9, 10]. Extent of necrosis correlates with probability of infection, organ failure, the need for intervention and overall mortality and morbidity. The main aim of this study was to evaluate the trends in management and outcomes in patients undergoing intervention for infected NP in 2 of the largest HPB centres in Malaysia and to analyse factors predicting mortality in these patients. Our secondary objective was to compare 2 of the commonest procedures performed in these 2 institutions, PCD alone versus VARD.
Study Design
This is a Cross sectional study of patients undergoing intervention for Infected Pancreatic Necrosis in 2 of the largest Hepatobiliary centres in Malaysia.
Data Collection
Data were collected from the institution written admission records and progress notes, outpatient clinic visit notes, operative database and the computer information system database for all patients diagnosed with NP between 2000 to 2018.
Participating Centres
Patients with necrotizing pancreatitis undergoing intervention for Infected Pancreatic Necrosis between January 2009 till December 2018 in Hospital Selayang (HS), Selangor and Hospital Sultanah Bahiyah(HSB),Alor Setar, Kedah were included.
Primary Objective
The main aim of this study was to evaluate the trends in management and outcomes in patients undergoing intervention for infected NP in 2 of the largest HPB centres in Malaysia and to analyse factors predicting mortality in these patients. The factors that were analyzed included the following
Patient demography: Age, gender, race, presence or absence of comorbidities (Hypertension, Diabetis Mellitus, Ischaemic heart disease, Renal impairment, COAD / Asthma, other premorbids), Aetiology (Biliary, Alcohol, ERCP related, idiopathic, hypertriglyceridaemia), admission to ICU, type of primary intervention employed (no intervention, PCD alone, VARD, Endoscopic drainage without necrosectomy, Open drainage/ resection), presence or absence of gas on CT scan, nature of necrosis whether ANC or WON, presence or absence of asscociated pleural effusion, duration of symptoms prior to admission, timing of primary intervention from admission, total number of interventions performed, days of hospitalization, Balthazar CT severity index score (CTSI) score, size of necrosis from cross sectional CT scan, C-reactive protein and Albumin levels prior to intervention.
Secondary objective: Using the variables above our secondary objective was to compare the outcomes of the 2 main interventions VARD and PCD alone.
Inclusion criteria: All patients diagnosed with Infected Pancreatic Necrosis between January 2009 till December 2018 in Hospital Selayang (HS), Selangor and Hospital Sultanah Bahiyah (HSB), Alor Setar, Kedah were included.
Exclusion Criteria: Patients with incomplete data or where outcome measures were not clearly stated were excluded. Traumatic pancreatitis was also excluded.
Statistical Analysis: All statistical analyses were performed using SPSS version 25.0 (SPSS Inc, Chicago, IL) and SAS version 9.4. Descriptive analysis was performed using Pearson Chi-squared test for categorical variables and Fisher exact test when appropriate. Continuous independent variables were analyzed using Mann- Whitney U test. Univariable and multivariable analysis were performed using binary logistic regression and penalized logistic regression where appropriate. Using a confidence interval of 95% a p value < 0.05 was considered statistically significant.
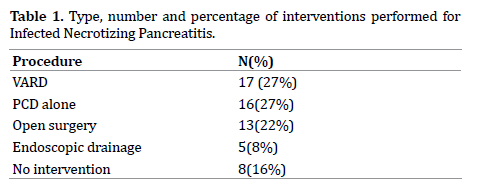
A total number of 65 patients (35 patients from Hospital Sultanah Bahiyah and 30 patients from Hospital Selayang) were included in the study. From this total only data from 61 patients were adequate for final analysis. 17 patients underwent Video Assisted Retroperitoneal Debridement (VARD),16 Percutaneous Catheter Drainage Alone (PCD alone), 13 patients underwent open surgery (open debridement, open resection), 5 were subjected to endoscopic drainage while 8 patients did not undergo any formal procedure (Table 1).
Out of the 61 patients that were included, final analysis were based on the outcomes of 59 patients (6 were lost to follow up). Mortality rate was 25% (15/59 patients).
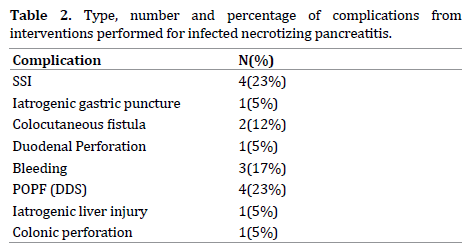
The following complications that developed included surgical site infection, iatrogenic gastric injury during percutaneous catheter drainage with ensuing peritonitis, colocutaneous fistula, bleeding, duodenal perforation, colonic perforation, post-operative pancreatic fistula (POPF) with disrupted duct syndrome (DDF) and iatrogenic liver injury (Table 2).
Positive cultures were obtained in 73% (43/59 patients). 16 patients had no growth from cultures taken. The commonest isolate was E.Coli followed by ESBL Klebsiella. Following are the different isolates obtained along with percentages (Figure 1).
Patient Demography (age, race, gender)
26 male and 18 female patients had complete resolution of necrosis. 11 male patients and 3 female patients died. (p = 0.097). There was no difference in outcome across the 3 races (p = 0.875). The median age for patients with CR was 43.7 +/- 14.45 and 55.13 +/- 12.36 for those patients who died (p=0.008).
Duration of Symptoms Prior to Admission, and Associated Comorbidities
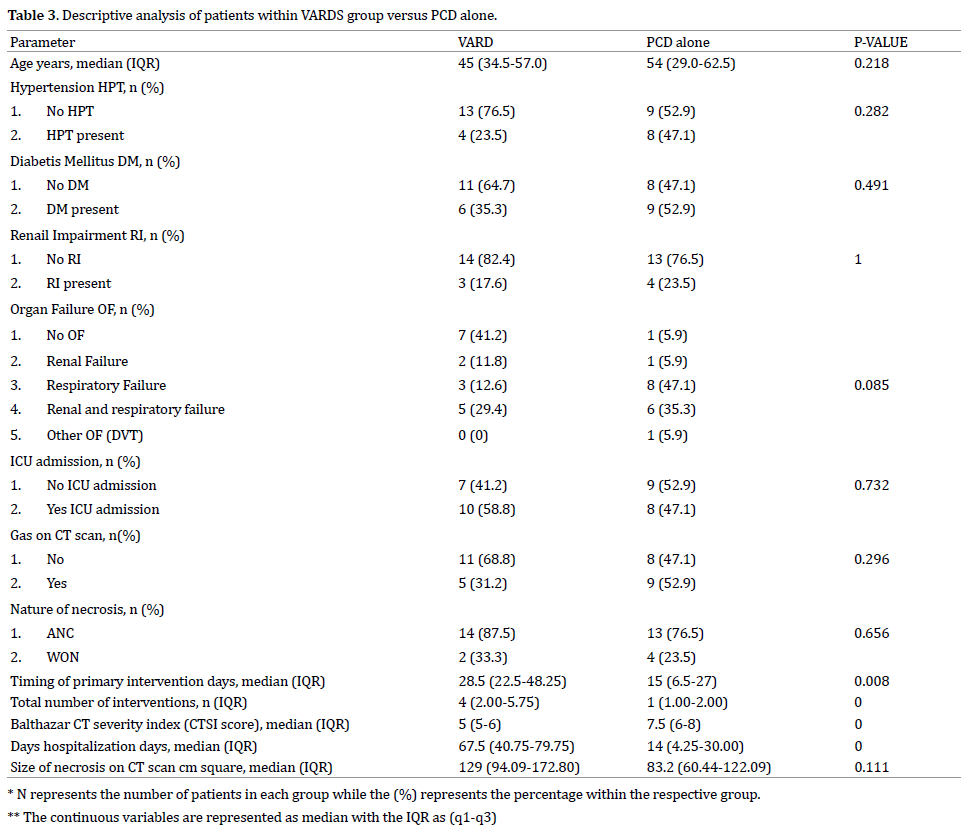
The median duration for patients in the CR group was 1 (1-4 days) while those within the D group was 1.5 (1-3) days (p = 0.690). When comparing comorbidities between the 2 groups, there was a statistical difference in patients who had Renal Impairment (p = 0.006). 41 (93.2%) patients in the CR group had no RI while 3 (6.8%) had RI in this group. In the group who died 9 (60%) patients had no RI while 6 (40%) had RI. No difference exist between the 2 groups in terms of HPT (p = 0.058), IHD (p = 0.593), and COAD/Asthma (p = 0.564). Within the group of patients who died, 66.7% (10/15) patients had DM compared with 36.4% (16/28) patients in the group with CR (p = 0.041) (Table 3, 4).
Aetiology of Pancreatitis
Within the group of patients who had CR 26 patients (59.1%) had biliary aetiology while 3(6.8%), 2(4.5%), 12(27.3%) had alcohol, ERCP and idiopathic aetiology respectively. Within the group of patients who died, 7 patients (46.7%) had biliary aetiology, 1 each (6.7%) were alcohol and ERCP related, while 5 patients (33.3%) were of idiopathic aetiology. There were 2 patients who had hypertriglyceridaemia, 1 had complete resolution while the other patient died. There was no statistical difference between the 2 groups when comparing the different aetiology (p = 0.774) (Table 5, 6).
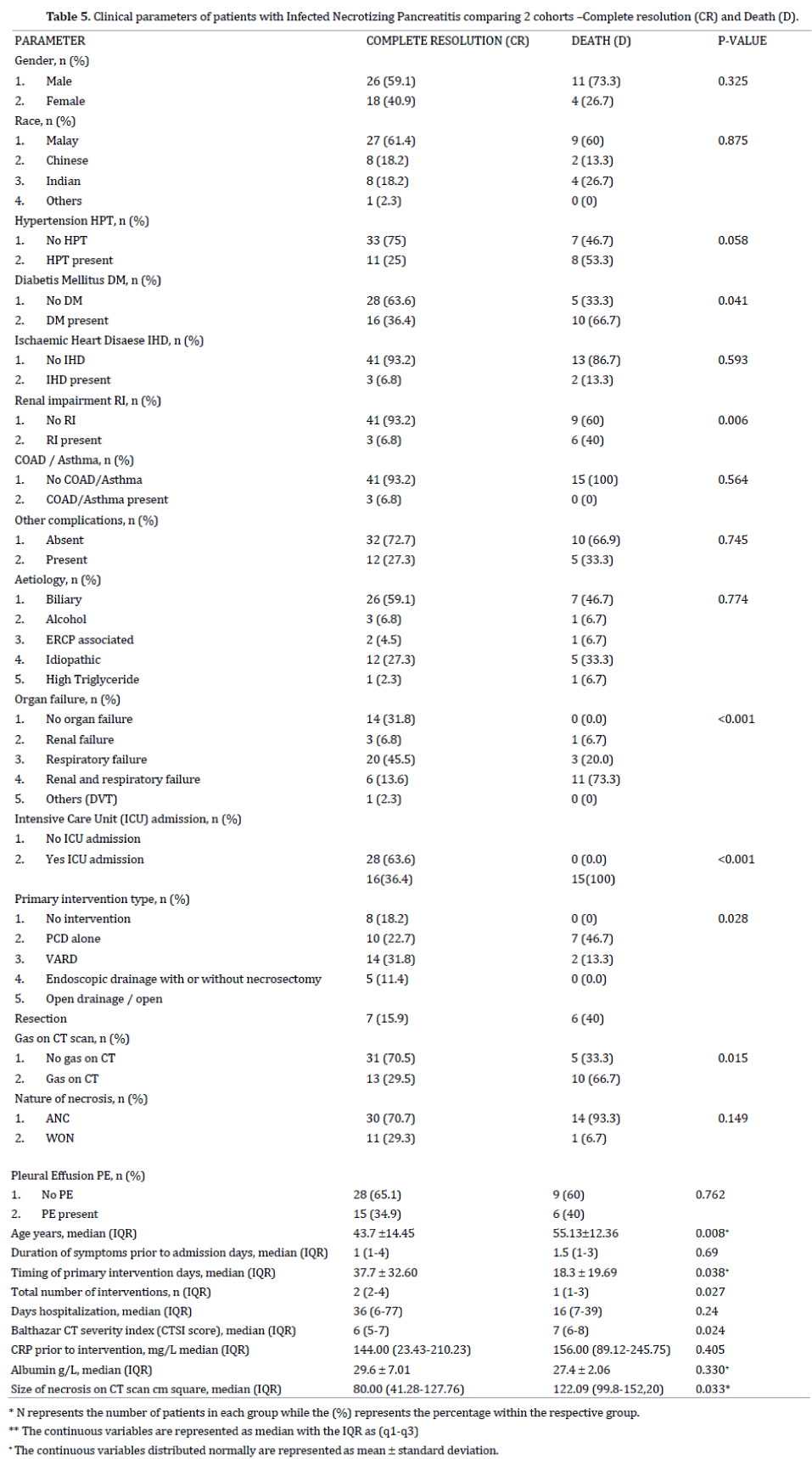
Organ failure (OF) and Intensive Care Unit (ICU) Admission
There was a significant difference between the 2 groups in terms of OF (p < 0.001). 14 patients (31.8%) in the CR group had no OF while there all patients in the D group that had at least one OF. In the CR group, 3 (6.8%) and 20 (45.5%) had renal and respiratory failure respectively. 6 patients (13.6%) in the CR group had a combination of renal and respiratory failure while 11 patients (73.3%) within the D group had a combination of these 2 OF. 1 patient who had DVT had CR. 15 patients (100%) within the D group had ICU admission. Out of the 34 patients with CR 16 patients (36.4%) were admitted to ICU while 28 (63.6%) did not require ICU admission. Overall, a higher percentage of patients within the Death group had 2 OF (renal and respiratory) (73.3% within D group vs. 13.6% within the CR group).
Type and Timing of Primary Intervention and Total Number of Intervention/s Performed
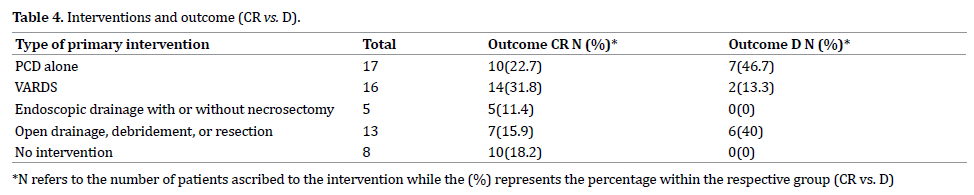
The commonest procedure performed was PCD alone (17) and VARDS (16),followed by open drainage and resection (13) and Endoscopic drainage with or without necrosectomy (5). Table 4 summarizes the interventions performed, number of patients and their outcomes. Of the 15 patients who died, 7 (46.7%) were from the PCD alone group, while 6 (40%) were from the open drainage / open resection group. Timing of primary intervention was 37.7 +/- 32.60 days for patients in the CR group and 18.3 +/- 19.69 days in the D group (p = 0.038). Patients in the D group had fewer number of interventions, 1(1-3) compared to the CR group 2(2-4) (p = 0.0027)
CTSI score, Size of Necrosis, CRP Level Prior to Intervention, Albumin Levels
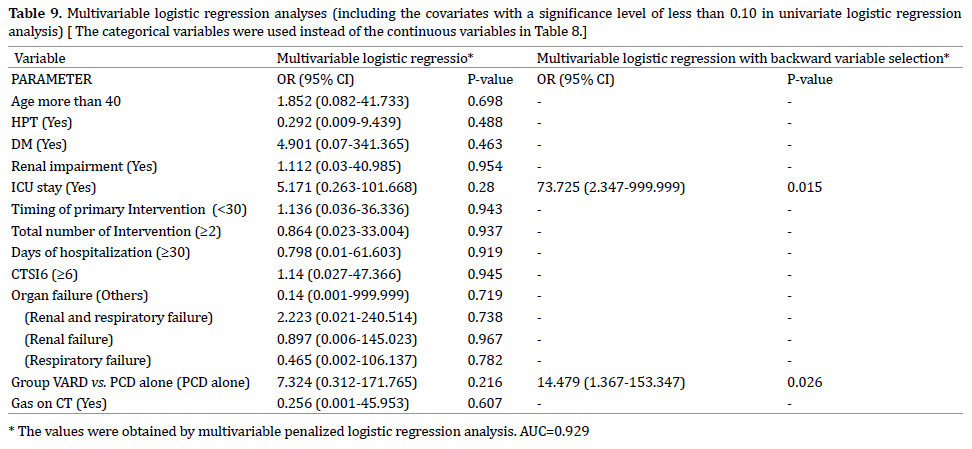
Patients with CR had a lower median CTSI score of 6 (5-7) compared to patients who died 7 (6-8) (p = 0.024). CRP (p = 0.405) and Albumin (p= 0.330) levels prior to intervention were similar in both groups. Size of necrosis on cross sectional imaging was significantly higher in the D group compared to the CR group (p = 0.033). Median size is 80.00 cm sq (41.28 – 127.76) in the CR group and 122.09 cm sq (99.8 – 152.20) in the cohort of patients who died (Table 7, 8, 9).
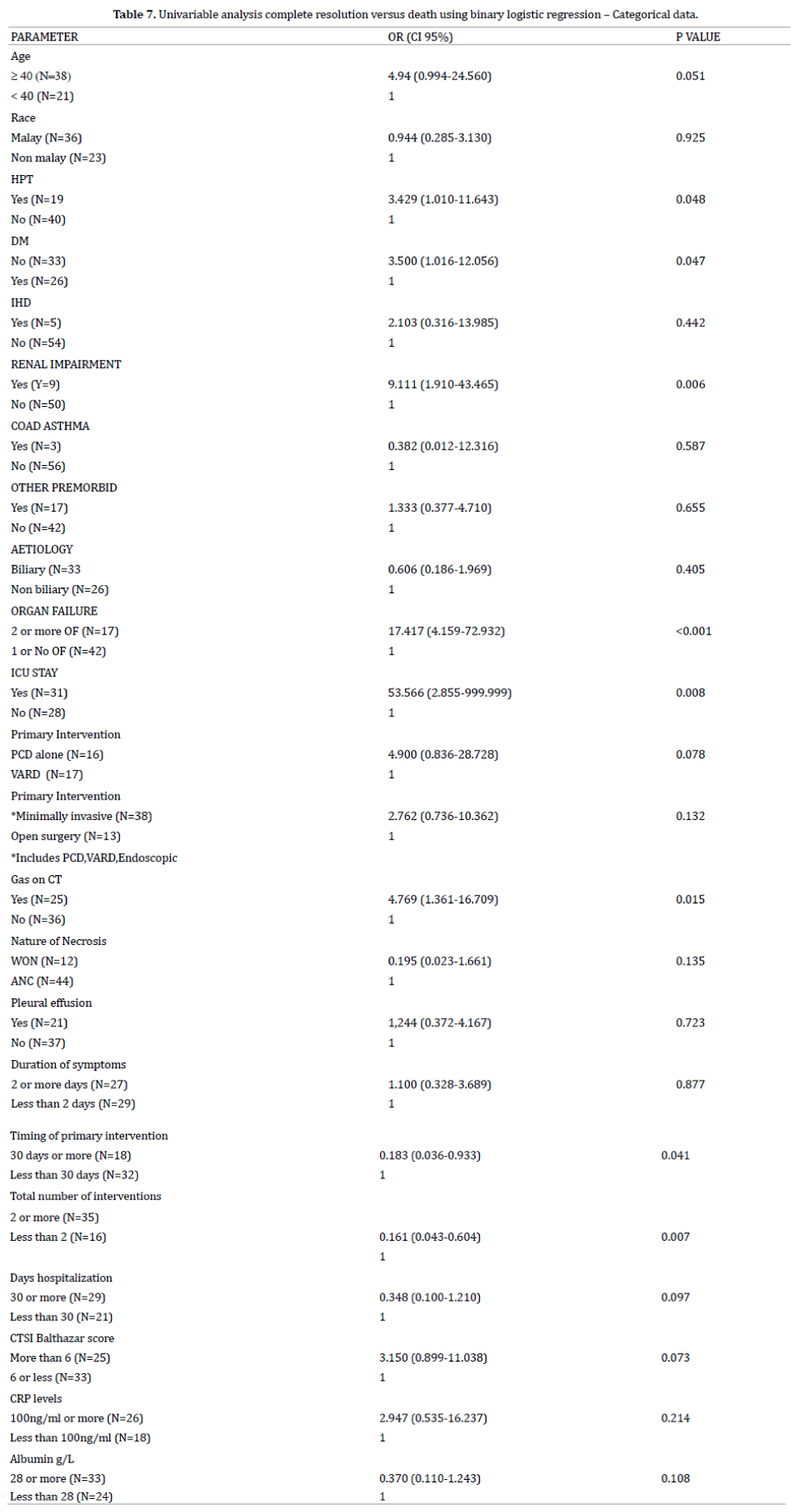
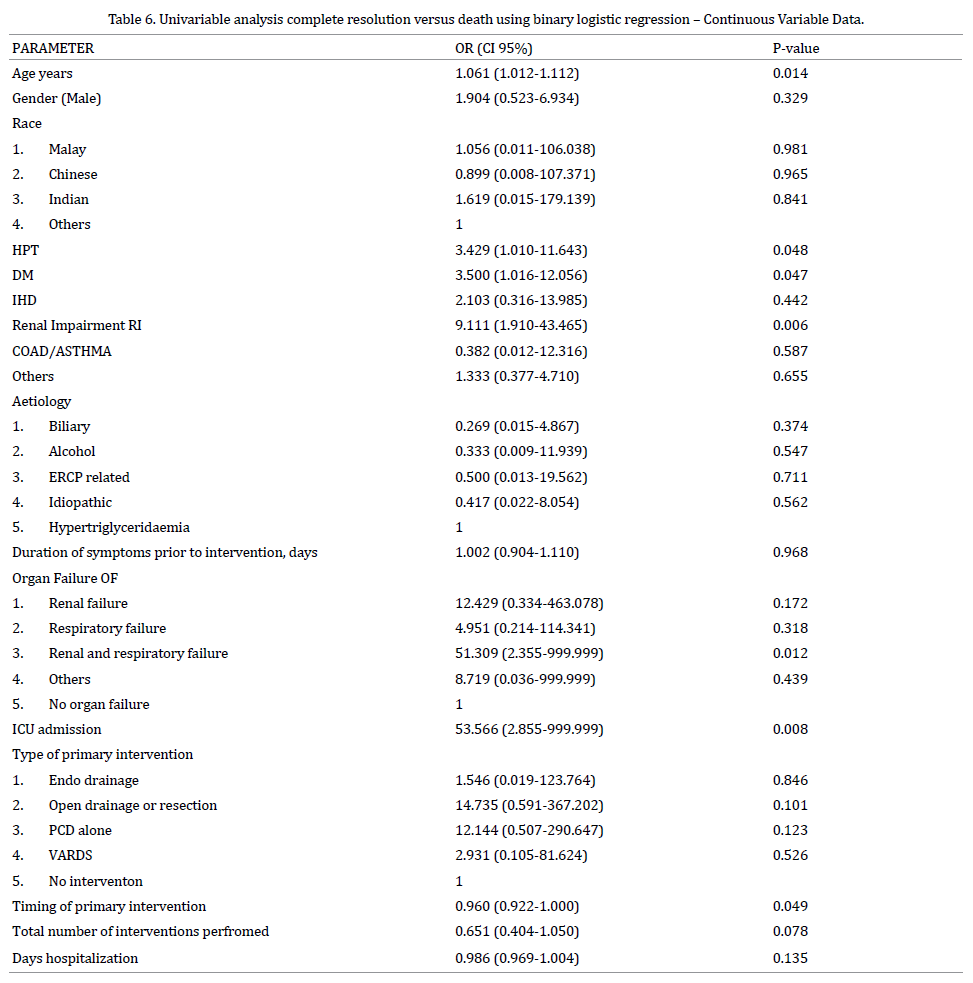
Factors Predicting Mortality
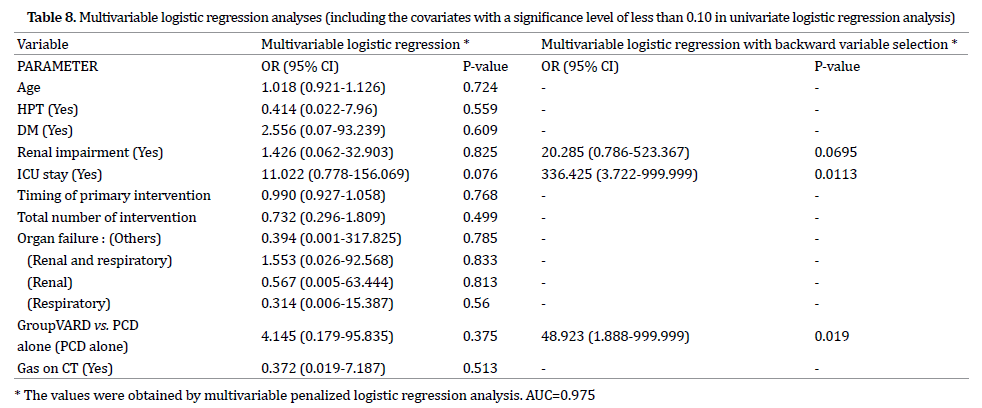
To identify the predictors of mortality, univariable and multivariable logistic regression analyses were performed for Death compared to complete resolution. Univariable analysis indicated that patients Age, presence of Hypertension and Diabetis Mellitus, Renal Impairment, admission to ICU, organ failure, intervention with PCD as oppose to VARDS and presence of Gas on CT scan were significantly associated with mortality. Penalized logistic regression analysis was performed for some variables with one cell having zero frequency in contingency tables.
We fitted two separate multivariable models. The first included the significant continuous variables and categorical variables in univariate analyses. The second model included the categorical variables created by their cut off values instead of continuous variables in the first model.
These values in multivariable analyses were obtained using a multivariable penalized logistic regression model. The final models of these models using a backward variable selection showed an Area under the Curve (AUC) of 0.975 for the first model and 0.929 for the second model. Renal impairment, admission to ICU and intervention by PCD were included in the final model of the first model and only admission to ICU and intervention by PCD were included in the final model of the second.
The present study highlights the different modalities that have been employed in the management of patients with infected NP within 2 of the main Hepatobiliary centres in Malaysia. Over the last decade or so these different modalities ranged from the traditional open drainage and debridement to the less invasive PCD and VARD, to modalities that require only drainage without debridement notably PCD and endoscopic internal drainage. Since the inception of the PANTER trial there has been a paradigm shift towards doing less and “stepping up” when required [5].
As we now understand that the necrosis that develops may be pancreatic as well as extrapancreatic (peripancreatic), there are still many questions to be answered regarding the natural history of these necrosums [11]. There still remains a question mark as to which patients can be managed with drainage alone and which would require additional debridement as well. This is due the heterogenous nature of the necrosis. It may be completely liquified, partially liquefied, softer friable necrosis, more adherent and not easily flushed suggesting that the process is an evolving one [11, 12]. The pragmatic approach would be to assume that all patients with ANC require drainage possibly obviating the need for debridement while those with WON require drainage and debridement. Based on the revised Atlanta Classification describing both ANC and WON, these collections are still heterogenous collections and to ascribe a particular treatment modality in terms of drainage versus drainage and debridement is difficult. However this is too simplistic.
Choosing a treatment modality should be based on many factors not least institutional capabilities, the least invasive route providing maximal clearance and tailored towards the patients outcome rather than the anatomical aspect of the necrosis. The nature of the necrosis has to be taken into consideration as well. It is imperative to have a standardize purpose so that the treatment modality can be tailored to the purpose rather than vice versa. This would include drainage, lavage, fragmentation, debridement, or excision [13, 14]. As a result it would be difficult to compare the outcome of different procedures as some patients who are treated with drainage and debridement may eventually improve even if debridement was not performed. The flip side is patients who are treated with prolonged drainage with multiple insertions and upsizing my have improved if debridement was performed earlier.
From our study the 2 most favoured methods were PCD alone and PCD followed by VARDS. PCD alone was the favoured modality of treatment in one of the institutions while VARDS was favoured more in the other institution. This practice reflects the institutional preference rather than one intervention being superior than the other.
As previously mentioned, there are many factors that predict mortality in patients with Severe Acute Pancreatitis [15]. However not many studies have been performed addressing the factors that predict mortality in patients with infected NP undergoing intervention. A large single centre retrospective study performed in the US revealed the determinants of mortality were increasing age, persistant organ failure and amount of necrosis.. Guo et al in a large prospective study showed that persistant organ failure after one week, age, bacteremia and pancreatic necrosis (as opposed to peripancreatic necrosis) were predictors of mortality [15]. In the present study, age, comorbidities such as Hypertension, Diabetis Mellitus and Renal Impairment, ICU stay, Timing and number of interventions, organ failure, Gas on CT scan, type of intervention (VARDS vs. PCD alone) were factors associated with higher mortality rates. However using multiple penalized logistic regression analysis ICU stay and PCD alone (compared to VARDS) were found to predict mortality in our cohort of patients.
There is compelling evidence that the use of PCD alone without a further “step up” procedure may be successful in managing patients with infected NP with reported success rates ranging from 50-55% and mortality rates harbouring between 15 to 17% [7, 8]. However so, there are many factors that have to be taken into consideration. Most of these studies were retrospective cohorts and included patients with sterile pancreatic necrosis. It is also difficult to ascertain for sure whether these collections warranted drainage to begin with. Also, approximately 10% of patients eventually succumbed to death as they were deemed unfit for further intervention.
Although PCD was found to be an independent predictor of mortality when compared to a VARD ( a “step up” procedure in our case), we cannot conclude for sure that VARD is superior to PCD. PCD was employed in all patients undergoing VARD. The indication for PCD was to drain any infected collection causing symptoms as well as sepsis. There may be an inherent bias in one of the centres to commit to VARD after PCD as part of the “step up approach” even though the amount of debridement may not have been significant, rather as a means for improved lavage. Secondly, patients in the PCD alone group may have been too ill to be subjected to another procedure, for example VARD or open surgery accounting for the higher mortality rate after this procedure.
On a head to head comparison, patients in the PCD alone group had significantly less interventions (median = 1) performed compared to those in the VARD group (median = 4) (p < 0.0001) but significantly higher CTSI score (median score of 5 for VARD group vs. 7.5 for PCD alone group) (p < 0.0001). This difference in the CTSI score could have accounted for the higher mortality rate. The fact that the VARD group had higher number of interventions could account for the fact that these patients were more tolerant to repeated general anaesthesia while the patients in the PCD group could have been more ill. Although not statistically significant (p = 0.086), a higher percentage of patients within the PCD alone group had a higher percentage of organ failure, notably respiratory failure and combination of respiratory and renal failure.
Our study had some noteworthy limitations. Our study did not include the cause of death of the patients and it was difficult to ascribe death due to the severity of pancreatitis or the intervention performed. Secondly, the reason for choosing one procedure over the other was not clearly defined. Whether VARD was actually required as a means of debridement or lavage was not clearly stated. In one of the centres that favour PCD alone, a large number of patients were transferred to other centres for continuation of care and important information with respect to their progress was not clearly documented.
However so, one important aspect that we have understood is that NP is a very heterogenous disease. The natural history of this disease is still not clearly understood. Most of the decisions regarding intervention are based on institution preference and available expertise. Perhaps defining the actual need or purpose of intervention is more important.
Mortality rate still remains high in patients with Infected NP undergoing intervention. Many of the factors associated with mortality are not modifiable. The inherent physiological insult resulting from the early systemic response of SAP coupled by the further deterioration once infection develops sets the tone for further deterioration. The persistent organ failure requiring ICU admission means that patients remain ill despite intervention. There is no doubt that a step up approach is necessary as the use of Percutaneous Catheter Drainage alone may not be sufficient in a selected cohort of patients.
This points to the fact that repeated debridements removing as much necrotic material may be required However much has to be learned regarding the natural history and nature of the infected necrosis so as to choose the appropriate treatment. We welcome further prospective studies evaluating this. Deciding on which patients will recover with drainage alone while deciding on an appropriate step up to further remove all necrotic tissue is paramount.
The authors had no conflicts of interest to declare in relation to this article.