- (2015) Volume 16, Issue 2
Animesh A Singla1, Francis Ting2, Apresh Singla3
1University of New South Wales, Kensington NSW, Australia
2Prince of Wales Hospital, Randwick, NSW, Australia, 3St Vincent’s Hospital, Darlinghurst, NSW, Australia
Received January 10th, 2015 – Accepted February 20th, 2015
Context The triad of acute pancreatitis, hypertriglyceridemia and diabetes is a rare occurrence. Case report A previously well 19-year-old male presented to the emergency department with 24-hour history of epigastric pain, associated with polyuria and nausea. Biochemical markers showed the presence of hyperglycemia (blood sugar level 15 mmol/L) and ketonemia (5.3 mmol/L). Further investigation revealed severe hypertriglyceridemia (4009 mg/dL) and elevated lipase (1,714 U/L). Abdominal ultrasound confirmed the diagnosis of acute pancreatitis. He was transferred to intensive care, where he received i.v. hydration, insulin and dextrose infusion. His metabolic derangements gradually resolved. His glycosylated hemoglobin was 13%, indicating the presence of chronically elevated blood sugars. Conclusion The possible pathophysiology and management of this unusual triad: diabetic ketoacidosis, hypertriglyceridemia and acute pancreatitis, are explored in this paper.
Diabetic Ketoacidosis; Hypertriglyceridemia; Pancreatitis
Diabetic ketoacidosis (DKA) is an acute metabolic derangement characterized by ketoacidosis, ketonuria and hyperglycemia [1]. It is the leading cause of mortality amongst children with type 1 diabetes mellitus (T1DM) [2]. Causative factors for DKA are varied including trauma, infection and insulin omission [3, 4]. Several complications of DKA have been documented, particularly cerebral edema, venous thrombosis, hypertriglyceridemia (HTG) and acute pancreatitis (AP) [5].
Recent papers have attempted to further elucidate the link between DKA and acute pancreatitis (AP). Hypertriglyceridemia is not uncommon sequelae in DKA and has been hypothesized as the most common inciting link triggering AP [5]. Hypertriglyceridemia accounts for a minority of AP (2-7%) cases overall, however the risk increases significantly when HTG levels rise above 1,000 mg/dL. The “enigmatic triangle” of DKA, HTG and AP has since been described in only a handful of case-reports. Majority implicate DKA as the preliminary insult, leading to HTG and subsequently AP.
We present the first known Australian case in literature of a 19-year-old male who presented with diabetic ketoacidosis, hypertriglyceridemia and acute pancreatitis with previously undiagnosed type 2 diabetes. We subsequently provide a review on this topic and discuss the relevance of screening via lipid panels and abdominal ultrasound in such presentations to ED.
Presentation
Mr. W is a 19-year-old obese male who presented to the emergency with a one-day history of sharp, nonradiating sudden onset epigastric abdominal pain. This was associated with nausea and polyuria but no vomiting. Mr. W initially presented to his general practitioner who had diagnosed him with gastroenteritis and prescribed simple analgesia. The pain however did not abate and Mr. W subsequently presented to the emergency department. He did have a maternal family history of type 2 diabetes mellitus. He did not have any significant history of alcohol, drugs, narcotics and was a non-smoker.
Physical examination revealed an obese male who was alert (Glasgow Coma Scale: 15/15) but distressed. He was noted to have Kussmal acidotic breathing with a respiratory rate of 24, tachycardic (HR: 115 bpm), normotensive (BP: 115/64 mmHg), and febrile with a temperature of 38.3. Further examination revealed a soft, distended and mildly tender abdomen on palpation, particularly over the epigastrium. Bowel sounds were normal. There were no other remarkable examination findings.
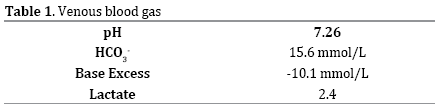
Initial laboratory parameters on his venous blood gas demonstrated a high anion gap metabolic acidosis with a pH of 7.22 (Table 1). Further testing, revealed ketonaemia (5.3 mmol/L), hyperglycaemia (15 mmol/L), hypertriglyceridemia (4, 009 mg/dL) and hypercholesterolemia (619 mg/dL). He had elevated lipase (1,714 U/L) and amylase (408 U/L) with mild neutrophilic leukocytosis. His liver function tests (LFTs) and renal function were within normal limits, although laboratory results were inconclusive due to the high level of lipaemia. Serum electrolytes were not significantly altered (Table 2).
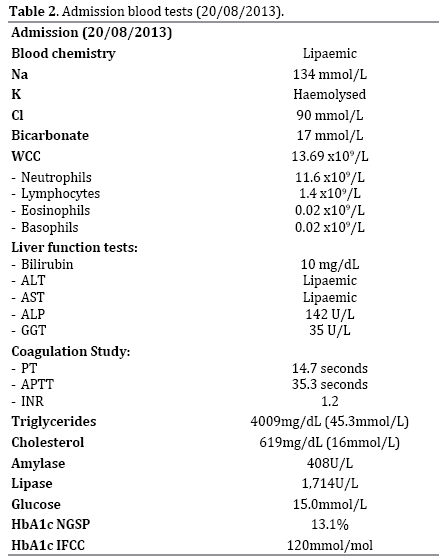
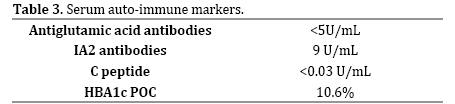
An ultrasound was performed in the emergency which revealed a thickened pancreas and 140 mL of peripancreatic fluid collection at the pancreatic tail. There was fatty infiltration of liver but no gallbladder involvement (Figure 1a). Antibody testing for autoimmune pancreatic insulin insufficiency did not show any abnormalities except a low C-peptide (Table 3). HbA1C was 13.1%. The septic screen performed at initial presentation was normal.
Management
Mr. W was kept nil by mouth and aggressively rehydrated with intravenous fluids (IVF) and commenced on intravenous infusion of insulin, with appropriate analgesia for pain relief. He was transferred to the high dependency unit for closer monitoring. He was initially commenced on 6 Units/hour insulin infusions with 5% dextrose at 100 mL/hour and normal saline at 250 mL/hour. This was titrated daily to his blood sugar level (BSL). This lowered his BSL and blood ketones progressively over the next five days. He was also commenced on 145 mg fenofibrate orally, with his triglyceride and cholesterol levels normalizing the following day (Figure 2). He was commenced on fentanyl patient controlled analgesia.
He was commenced on a normal diet day 3 of his admission. Repeat ultrasound showed resolution of pancreatic inflammation and a well-defined hypoechoic region adjacent to the pancreatic tail consistent with a pseduocyst (Figure 1b). He had an additional hypoechoic region in the body of the pancreas suggestive of residual edema.
On discharge his medications were: fenofibrate 145 mg daily, insulin glargine 25 units pre-dinner and insulin aspart 6units three times a day pre-meals.
The literature on combined presentations of diabetic ketoacidosis, hypertriglyceridemia and acute pancreatitis are sparse [6-11]. Only two such cases have been described in the pediatric literature [6-8]. All previous cases cite DKA as the initial factor, contributing to subsequent hypertriglyceridemia and pancreatitis. The underlying pathophysiology of DKA is related to an absolute or relative insulin deficiency [12]. The termination of the TCA cycle causes an accumulation of acetyl-CoA down the ketogenesis pathway to provide energy for essential organs including the brain and heart. In addition, lipolysis increases free fatty acids which are used to synthesize VLDLs in the liver. Subsequently a reduced peripheral tissue lipoprotein lipase results in a build-up of VLDLs in serum, causing lipaemia and hypertriglyceridemia [6, 12]. Acute pancreatitis results from inappropriate activation of pancreatic enzymes and auto-digestion.
In acute pancreatitis alone, raised lipase or amylase, greater than three times upper limit is accepted as diagnostic [13]. However in 16-25% of DKA, non-specific hyperamylasemia and hyperlipasemia (including greater than 3-time reference normal) have been reported, without clinical or imaging evidence for acute pancreatitis [14]. In addition, acute pancreatitis in the setting of DKA with normal lipase levels has also been previously described [15]. The relevance of amylase becomes even less specific when we consider up to 50% of AP secondary to triglyceridemia has no raised values, relating to lipaemic content of the blood and disturbance in calorimetric measurement [14].
In our case, aggressive hydration, insulin/dextrose infusion and initiation of a fibrate resulted in correction of acidosis and concurrent resolution of hypertriglyceridemia. However, in other instances, the severity of triglycerdemia has necessitated urgent plasmapheresis [9, 10]. In nearly all cases, HTG levels >1, 000 mg/dL were present. This highlights the importance of initial lipid profiling in this cohort of patients, as it provides a trigger for early abdominal imaging for potential pancreatitis in these patients. In addition, abdominal pain is a common feature in both AP and DKA processes. Nearly 50% of DKA cases may present with abdominal pain relating to several gastrointestinal manifestations [16]. Given the not insignificant co-existence of acute pancreatitis, we suggest screening for severe hypertriglyceridemia induced pancreatitis is warranted. Lipase and amylase alone do not appear to be accurate markers of pancreatitis in this cohort of patients [14]. Thus we suggest the introduction of routine lipid profiling in addition to enzyme markers to minimize delay in diagnosis of this potentially fatal triad. Acute pancreatitis can worsen hypovolemic shock and metabolic derangement in DKA. Furthermore, initiating oral intake too early in context of unknown pancreatitis can be devastating.
Whilst previous studies mention a role of imaging in patients with persistent abdominal pain despite correction of acidosis, we believe early abdominal screening has a potential role in DKA in the setting of detected raised serum markers. We believe ultrasound is a cheap, effective and safe option in the initial instance.
Authors declare to have no conflict of interest.