Keywords
Acute renal failure; Colon; CT scan; Constipation
Introduction
Diverticula in the colon are very common, but only 10-20% of the diverticulum carriers develop a diverticulitis [1]. The inflammation can lead in 15% of the patients to a free perforation [2]. In this case report, an unusual localization of the diverticulum appears which leads to an acute renal insufficiency.
Case Report
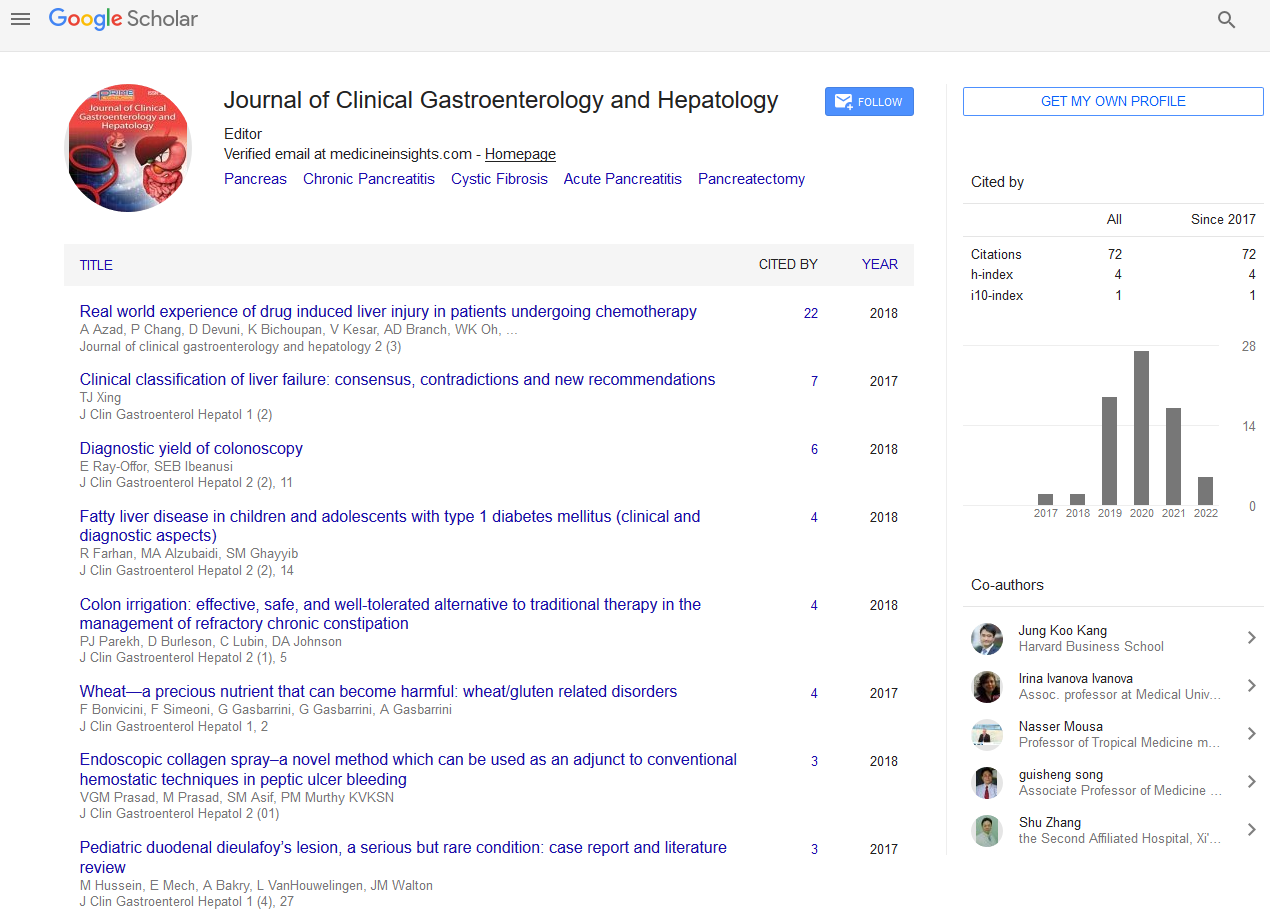
A 75-year-old female patient was transferred to the central hospital in Bern after a CT scan was made in the peripheral hospital which showed free infraperitoneal air of unclear aetiology..
At the hospitalization the patient was cardiopulmonary stable and afebril (pulse 78, 98% oxygen saturation, blood pressure 111/61, temperature 37.2°C). The clinical exam reported pain in the lower abdomen, without signs of peritonism. The digital rectal examination showed a slight anal prolapse and an emphysema was palpated pararectal. The blood control showed elevated leukocytes (21.8 G/L (neutrophils of 20.31 G/L)), CRP (261 mg/L) and creatinine (234 micromol/L).
The patient reported a general weakness for approximatively 2 weeks with reduced appetite and a single episode of vomiting. In the same time she noticed constipation. The last bowel movement was two days ago, since then she had pain in the abdomen, in the back and the renal flanks on both sides. The patient history showed an appendectomy in childhood and a hysterectomy due to menorrhagia at the age of 41 (1982) (Figures 1-3).

Figure 1 Initial CT abdomen in the external hospital with free infraperitoneal air.

Figure 2 Initial CT abdomen in the external hospital with compression of the rectum (a). Emptied urinary bladder with inserted catheter. The urinary bladder is displaced to the right due to the high pressure (b).

Figure 3 Initial CT abdomen in the external hospital. Dilated renal pelvis by postrenal obstruction due to the high pressure with compression of the ureters.
An empirical antibiotic therapy was started with rocephin and metronidazole on suspicion of a rectosigmoid perforation. On the same day a rigid rectoscopy and a gynecological examination have been performed which showed no perforation.
Due to the compression induced postrenal renal insufficiency the decision was made to aspirate the free air pararectal to reduce the infraperitoneal pressure. After previous endosonographic presentation of the rectum, 500 ml air and 1 ml bloody secretion was drained, which was used for microbiological examination with no bacterial growth after a few days. For follow-up control a CT scan was made after the decompression (Figure 4).

Figure 4 After decompression with expansion of the rectum.
The day after, blood samples showed decreasing infection values (CRP 220 mg/L, leukocytes 14 G/L) and creatinine (172 micromol/L). On the same day a flexible rectosigmoidoscopy was performed, which showed a small ostium in the rectum at about 6-7 cm from ano, compatible with the perforation site. This ostium was supplied with an OTS (over the scope)-clip (Figure 5).

Figure 5 Rectosigmoidoscopy with possible perforation site.
Due to a rising CRP value of 293 mg/L two days later a CT scan was made. A new fluid collection was found and drained on the same day CT scan controlled. The drainage extracts turbid brown secretion, so the rectosigmoid perforation was confirmed (Figure 6).

Figure 6 Insertion of a pigtail-drainage into the fluid collection.
In the liquid taken from the drainage, intestinal flora was detected in the microbial culture.
Following blood samples showed decreasing the infection values and the kidneys recovered completely. In the follow up CT scan five days after hospitalization, the fluid collection was decreasing with pigtail catheter positioned correctly. The patient was discharged home on the same day with antibiotics and drainage daily flushed by the home care.
Ambulant follow up showed decreasing infection values under antibiotical treatment, with a CRP value of 7 mg/L directly after antibiotics stop. Unfortunately the drainage produced continuously purulent fluid. In the next control the patient had fever and the infection values increased again. After one month a diagnostic laparoscopy was made which showed several inflammatory visceral adhesions. Due to this situs, with active inflammation, a recto-sigmoid resection with descendostoma (Hartmann situation) was performed by a lower median laparotomy. The histopathology showed a purulent- abscessing diverticulitis with granulation tissue without malignancy.
Discussion
Diverticulosis is very common, up to 50% of all individuals older than 60 years have colonic diverticula. About 10-20% develop a diverticulitis [1]. Herniation of the colonic mucosa through the circular muscle layers of the colonic wall leads to diverticula. Mostly the herniation is at the site of penetrating blood vessels through the colon wall [3]. The prevalence increases with age. Risk factors for diverticulitis are obesity and smoking [4].
Diverticulitis can lead to a free perforation in to the peritoneal cavity or generate an abscess. Differential diagnoses of a free colon perforation include tumor, IBD, treatment with NSAIDS and stercoral perforation. Approximately 16% of the patients with acute diverticulitis develop an abscess [5]. Which leads to an operative therapy or a percutaneous drainage is then required. A systematic review has shown that 50% of the abscesses (Hinchey stages IB and II) were successfully drained by radiology [6]. The drainage could eliminate the two-step procedure with a temporary colostomy and lead to an operation with a primary anastomosis [7].
In this case, the perforation was below the peritoneal fold and formed a valve mechanism that resulted in a massively increased infraperitoneal pressure. According to the literature research, no similar case has been published in which a tension pneumopelvis has led to a displacement of the urinary tract with an acute postrenal renal insufficiency and an ascending urinary tract infection.
The pararectal puncture with the release of free air rapidly improved kidney function and minimized the risk of urosepsis. No perforation was detected in the rectoscopy, so a flexible sigmoidoscopy was made. There, the perforation site was located and sealed with an OTSC. However, in the follow up rectosigmoid perforation occurred in the infraperitoneal space.
Retrospectively, it has to be discussed whether the flexible sigmoidoscopy and the forced search for the perforation site was necessary. Although an OTSC could be placed on the possible perforation site, it is questionable whether the infraperitoneal space was contaminated by sigmoidoscopy or not. A percutaneous drainage in the infraperitoneal space, after exclusion of a large perforation by the rectoscopy, would have been debatable. Thus, the pressure in the pelvis would have been minimized and the perforation site might have healed under antibiotic therapy.
Conclusion
Although diverticula in the rectosigmoidal transition are rare, it must be considered when infraperitoneal air is visible. Pressure decrease is recommended to prevent secondary urinary retention.
Competing Interests
The author declares that she has no competing interests (political, personal, religious, ideological, academic, intellectual, commercial or any other) in relation to this manuscript.
References
- Weizman AV, Nguyen GC (2011) Diverticular disease: Epidemiology and management. Can J Gastroenterol 25: 385–389.
- Vermeulen J (2010) Treatment of perforated diverticulitis with generalized peritonitis: Past, present, and future. World J Surg 34: 587–593.
- Hobson KG (2004) Etiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg 17: 147-153.
- Feuerstein JD, Falchuk KR (2016) Diverticulosis and diverticulitis. Mayo Clin Proc 91: 1094-1104.
- Bahadursingh AM, Virgo KS, Kaminski DL, Longo WE (2003) Spectrum of disease and outcome of complicated diverticular disease. Am J Surg 186: 696-701.
- Lamb MN, Kaiser AM (2014) Elective resection versus observation after nonoperative management of complicated diverticulitis with abscess: A systematic review and meta-analysis. Dis Colon Rectum 57: 1430-1440.
- Stollman N, Raskin BJ (2004) Diverticular disease of the colon. The Lancet 363: 631–39.