Keywords
Oncology; QOL in special populations; Elderly;
Clinical guidelines; Meaningfulness; Guided decision-making
Introduction
Oncological guidelines are references for diagnostic and
treatment procedures based on the available scientific
knowledge and intended to assist physicians in treatment
decision-making, enabling them to provide the best possible
medical care to their patients. However, these recommendations
are not always followed, especially in the case of older patients,
although modern guidelines have been adapted to the needs of
aging cancer patients [1-3]. It has been reported, for instance,
that elderly patients with colorectal carcinoma were less
frequently treated in accordance with guidelines than younger
patients [4,5]. Except for adherence to aromatase inhibitors [6],
studies have shown that elderly patients with breast cancer were
less likely to receive guideline therapy; these included breastconserving
therapy, radiation therapy, axillary dissection, as
well as adjuvant and systemic treatment, such as chemotherapy
or anti-hormone therapy [7-10].
From the point of view of the physician, deviating from standard
therapy recommendations by dropping some components of
guideline-based therapeutic regimens might be well justified in
the presence of factors such as comorbidities or other medical
limitations. In this study, we present the patients’ perspective
on deviations from the therapy recommended by their treating
oncologist by exploring factors behind acceptance or rejection
of all or some components of recommended treatment.
Although there are earlier studies on this topic, the conditions of
oncological patient care have changed substantially in the last
few years, and we believe that a re-examination of decisionmaking
based on informed consent in oncology is warranted in
the view of these new findings. We focused on older (>69 y) breast cancer patients, since several recent publications reported
that, in this age group, guideline-based therapy was more often
lacking in breast cancer patients than in those with other cancers
[7,9,10]. One of the objectives of this qualitative study with the
selected population of female patients with breast cancer after
their initial treatment was to provide a basis for the development
of survey instruments used in the assessment of PROM/PREM
(patient-reported outcome measures, patient reported experience
measures). Also, the findings might help build a structured and
focused patient-doctor conversation with the integration of the
topics that are decisive for the patients’ decision making.
Methods and Materials
Design of the qualitative study
The study was approved by the Ethics Committee of the
University. We conducted qualitative interviews with breast
cancer patients in a one-on-one setting. We followed most of the
published criteria for reporting qualitative research (COREQ)
[11]. The development of relevant questions (interview guides)
was based on a comprehensive review of the literature and
extensive experience in the field of oncological treatment of the
clinical authors. Questions that referred to plain facts, those that
reflected too closely the interviewer’s expectations as well as
those that might be too abstract from the patients’ point of view
were dropped. Subsequently, the questions were sorted, and
as many questions as possible were subsumed under a single
open question. With this method, as described by Helfferich,
we identified certain topics of interest, but did not have a formal
guide, which allows the patient to co-determine the direction of
the interviews [12].
All interviews were conducted by a medical student who
received extensive training from the qualitative research
group of the university. An oncologist was not involved in
the interviewing process to avoid bias resulting from previous
professional experiences with older patients. As compared to
interviews conducted by doctors, this has the advantage that the
student has no preconceived opinion regarding the therapy. No
relationship with the participants was established prior to the
interviews.
Patient approval was obtained prior to starting the interviews.
All interviews were recorded as audio files with a portable audio
device. The clinical authors took information such as the date of
primary diagnosis, stage, comorbidities and treatments carried
out from the medical documents and compared them with the
current guidelines. We defined the following topics in relation
to decision-making: (1) conversation with doctors, (2) role of
family, friends and family doctor, (3) impact of age, (4) future
expectations and (5) satisfaction with conversations with the
treating oncologists and the treatment received. Typically, we
started a conversation with an open question such as: “After
you received your cancer diagnosis, what happened next?”
Later we asked more specific questions: for example, “what are
your expectations for the future?” Although the topics were the
same in all interviews, the exact formulation of the questions
was adapted to the participant and conversation atmosphere.
Also, the interviewer was allowed to raise additional questions
at certain points if necessary.
Selection of patients
Study participants were recruited from an oncological
rehabilitation clinic and the gynecological department of the
university hospital. Patients were given an information flyer
describing the goal of the study (to find out personal factors
for accepting or rejecting the doctors' recommendations, from
the viewpoint of the patients) and asked if they are willing to
be interviewed by the student. The patients were also asked
if they agreed with the merging of the clinical data from the
medical files before anonymizing the records. Approximately
one-half of the patients who were invited to participate refused,
the reasons given being lack of time or lack of interest.
Theoretical Sampling, which involves the researcher collecting
and analyzing the first data while planning the interviews with
the next group of patients [13], was the methodological approach
employed in this study. Initially, similar cases were investigated to
form first categories, followed by cases, which allowed reflecting
on the largest possible variation in age, and severity of disease.
Following these rules, a total of 17 patients were interviewed to
reach saturation. Most of the interviews took place in the rooms
of the patients at the rehabilitation center or hospitals; one patient
was interviewed at home and one patient had a telephone-based
interview. At the beginning of the interview, the reasons for
conducting the research project were explained to the participants.
Patients being of advanced age and liable to tire easily, interviews
lasted 10-30 minutes each, which is shorter than interviews in
qualitative studies in general.
Data analysis
The recorded audio files were transcribed verbatim to text files. Evaluation of data was based on the concept of Grounded
Theory, using the procedures of open coding, axial coding,
and selective coding according to Glaser and Strauss [14].
First, open coding was done: relevant texts were marked, and
these were classified under the first set of descriptive concepts.
Further ideas, associations or questions were noted in the
form of memos. The second step involved axial coding, with
subcategories and the relationships between the categories being
worked out. Categories central to the theories, the so-called axis categories, were defined. In the third step of the selective
coding, the axis categories were again revised using the original
data with the aim of describing as many variations as possible
by key categories. As a result, a network of aspects that play
a role in the decision-making process emerged. In addition,
a summary was compiled for each interview to describe the
individual experiences of the patients as well as the individual
core statements. For the coding process, the computer program
MAXQDA 12 was used (VERBI Software GmbH, Berlin,
Germany). To avoid distortion of results by the interviewer's
sole interpretation, the reflections and results were discussed
several times with members of the qualitative research grou
at the university. Since the first results were considered as
plausible, it was decided to include additional patients outside
the oncological rehabilitation clinic and to include at least one
patient in a palliative situation.
Results
According to the medical records of the interviewed patients,
11 patients were treated in line with the guidelines. Six patients
(35%) rejected one or more components of the recommended
therapies: axillary dissection (1), chemotherapy (1), radiation
(2), and/or adjuvant treatment with aromatase inhibitors (3), tamoxifen (1) or herceptin (1) Table 1.
| Number |
17 |
| Age |
70-79 y; median 73 y |
| Tumor Stage |
T1, n=7; T2, n=8; T3, n=1; M1, n=1 |
| Deviation from guidelines* |
6/17 (35%) |
*Guidelines (Deutsche_Krebsgesellschaft, 2017)
Table 1: Patients characteristics.
Factors that influenced patients’ decisions
Following the concept of Grounded Theory, in the first step of open coding, descriptive codes were identified. These were, for
instance, aspects mentioned by patients when they described
the conversations they had with their doctors, such as taking
time, explanations, whole truth, objectivity, calmness, personal
situation, optimism, changing contact persons etc. Further ideas
were noted in the form of memos.
In the second step, the axial coding, the first set of relations
between categories were defined. We identified aspects that
led to patient acceptance of the recommended therapy and
aspects that resulted in a rejection of the recommended
therapy Table 2.
| Acceptance of therapy |
| • Trust in doctor |
| • Comprehensive information and explanation from the doctor |
| • Doctor addressing the living conditions of the patient |
| • Lack of alternatives |
| • Desire to spend some more time with the family |
| Rejection of therapy |
| A feeling that therapy-associated impairments outweighed or would outweigh the advantages of therapy |
| • Quality of life interpreted as negative in the context of age |
| • Inadequate information from the doctor |
| • Influence of the family doctor towards therapy rejection |
Table 2: Axial coding categories: Acceptance and rejection of recommended therapies.
Reasons for therapy acceptance
Trust in the doctor: Nine patients underlined their trust in
their physicians as a major reason for following the doctor’s
recommendations.
"The doctor assured me she would tell me (about all the
treatment possibilities). And I should think about them. I had
a lot of confidence in the doctor. She is a consultant. She was
always there with me in the operating theater. She was always
there for me and I could also have a good conversation with
her. And she said, <This is the advice I would give my own
mother>".
Trust was promoted by a good relationship with the doctors.
Many patients said that it was important for them that the
doctors were friendly, sympathetic and sensitive. They wanted
the doctors to give them a feeling that their concerns were
taken seriously and that they were really interested in them as
individual human beings. In this context, personal relationship
with the doctor was of importance.
"I must say it is not nice to be just a number, but to be considered
as an individual. And I think that's good. And this is not always
the case, this (situation of) being looked upon as an individual.
And that's exactly what a cancer patient needs".
Comprehensive information and explanation: Fifteen patients
expressed a desire to be fully informed about their disease. Trust
was also promoted when physicians provided relevant medical
information in an understandable way. Most of the patients
said that it was of the utmost importance for them to know
the full truth about their disease, they wanted to be fully and
comprehensively informed both about their illness and available
treatment.
“Yes, for me it is always important that I know everything
exactly. Then I am satisfied, then I can adjust to it. But when
I'm unsure and do not know what to expect - that makes me a
bit nervous".
Addressing the living conditions of the patient: A patient in a
palliative situation with a chest wall recurrence initially wanted
to refuse additional therapy. During treatment for her first cancer,
she had experienced the therapeutic procedures, especially
chemotherapy, as very stressful. However, her doctor convinced
her of the usefulness of undergoing therapy by explaining that
there were still various other treatment options available. In
addition, he had taken into consideration her personal situation. "And so, I wanted to say to myself: now let us drop the whole
thing, if that does not have any effect any more, you don’t need
to trouble yourself any further, then we shall just drop the whole
thing. And then the doctor said: No. I would advise you very
much (to continue with the therapy), you have grandchildren
and you still enjoy your garden very much and so on and so
forth. (If you continue the therapy), you would continue to
participate in life and that is something that is always worth
doing". In retrospect, the patient was very grateful to have
continued with the therapy and underlined the fact that she was
also having a good quality of life.
"And I live here alone, but honestly I do not see myself as
suffering under limitations. I like to play bridge. (...) And yes,
I cannot even imagine a better life than I actually have at this
age. I even go with friends on a one-week bridge holiday. And
I can do all these. I am not confined to bed. I will not let things
come to this point. (Laughs)".
Lack of alternatives to treatment: One reason given by seven
of the patients who followed the recommendations was that they
felt there were simply no alternatives to the treatment proposed
by the doctor.
“If one has to do something, then one must do it. If one wants to
have a chance (to survive)”.
Desire to spend some more time with the family: Ten patients
explained that the family played an important role in their
treatment decisions. Family support helped patients make
decisions and enabled them to deal with the illness. Frequently,
patients discussed therapy decisions with family members. The
desire to spend as much time as possible with their families
motivated the patients in some cases to accept even unpleasant
therapies.
"... and I will be a great grandmother. And that is something
again I'm looking forward to. I want to be a great grandmother
now, so I need to be healthy. I want to live long enough to
experience that".
Reasons for rejection of therapy
Therapy-associated impairments outweighing advantages
of therapy: Five of the patients who declined guideline-based
treatment did so despite the doctor's recommendation; they
rejected therapy components after weighing the advantages
and disadvantages. In particular, adjuvant systemic therapy was rejected with the argument that the benefits would not be
justified by the expected adverse side effects and reduced the
quality of life.
"And I had noticed this and then I was told: the chances, that
is, only the statistical chances, it is always only a matter of
statistics, but well, the chances were only 1 percent in my case.
And that would be reason enough for me to consider whether
the benefits would well outweigh these side effects. And then I
said: no, then I shall do without this treatment".
In this context, infrastructure and difficulties in getting to the
treatment centers also played a role in therapy rejection. This is
a patient-based reason but also a structural one.
"And I have no desire to go for breast radiotherapy for 52 weeks.
I want to be quite honest with you. Then I would put myself
again under a lot of stress. You must consider that I have to
travel to the clinic and back. It always takes 45 minutes (to get
to the clinic). Then the taxi driver is waiting for me and it takes
another 45 minutes to get back home. And this every day for 5
weeks, no 52 weeks. No, I am not going to do this to myself".
Quality of life interpreted in the context of advanced age: Five
patients rejected parts of the therapy because they expected a
reduction of life quality associated with the suggested treatment
in the context of their age. The majority of patients considered
cancer in advanced age as less worrisome than in younger years.
Nine women said they would have been more worried about
the future if they had become ill when they were young. In
old age, illness would be a part of life and would be easier to
accept. They felt that it would be a more difficult situation for
younger women with cancer because they would be needed to
look after their children. Some women also said that they would
have fought more against the disease and would have accepted
a reduction of life quality as a necessary price to pay in younger
years. In the context of their age, three patients said that they
wanted to have as high a quality of life as possible, so that they
would even be willing to accept the risk of recurrence and the
uncertainty about disease progression as a result of rejection of
therapy if this was associated with reduced quality of life.
"And then I said to the doctor: dear lady, I am 75 and I have a
pacemaker, and I have to go back to the hospital for 8 days, the
pacemaker has to be re-implanted and I do not want to add any
more stress with (cancer) therapy".
Another patient said:
"You need not answer me, but (she laughed), I guess ….well, I'll
be 80 next month. Do I really have to do these things to myself?
I don’t believe so. So, I have now made this decision for myself
(….)”.
One patient who rejected therapy because of age and fear of
adverse side effects, mentioned faith in God as an important
factor in coping with the disease. She hoped that her life would
be extended and that she would be able to spend some more
time with her family. However, she accepted death as part of
life and believed that there was something more than just this
life on earth.
Inadequate information from the doctor: Two of the patients
who rejected anti-hormonal therapy said that they had not been adequately informed about possible side effects. When asked
if there had been any conversation about side effects at all, one
patient answered:
"Yes, but not much. She only said: you must take it, because
you cannot rule out that the disease has spread. This medicine
is to support the therapy so that there is no recurrence of the
disease".
Influence of the family doctor: For most of the patients, while
the gynecologist was the most important medical contact, the
family doctor who often regularly checked blood values was
also very important. Eleven patients said that it was very
important to them to have a GP they could consult. Two of the
patients who had refused parts of the recommended treatment
regimen said that that they did so in agreement with the opinion
of their family doctors in whom they had complete trust.
“I called my family doctor and I explained to him (my situation
and decision). He said: you can stop taking these pills with a
good conscience”.
Although patients consulted their family doctors, for additional
help in decision-making, most patients reported that it was
their own decision to reject parts of therapy recommended and
offered by the doctors. For example, one patient said:
"I'm not like that. I never want to give up my independence. I
always want to decide for myself because I know my body. I
always want to have a doctor who accepts my decision, but one
who at the same time empowers me to make my decision".
Only one patient said that therapy decisions were made by the
doctors without consulting and discussing therapy-associated
issues with her.
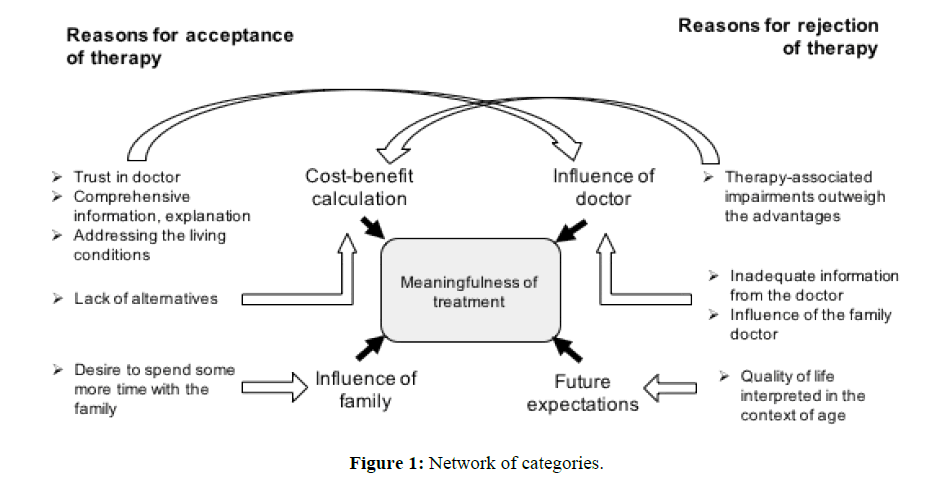
Selective coding categories and core category
In the step of selective coding, we defined more abstract
categories to summarize the factors that influenced the decision
by using the original data again. We identified the key categories
as follows: “Cost-benefit calculation”, “Influence of doctor”,
“Influence of family” and “future expectations”. The final core
category that emerged was "meaningfulness of the treatment in
the particular situation" (Figure 1).
Figure 1: Network of categories.
Finally, meaningfulness of treatment in the context of the
individual living situation with advanced age playing a
predominant role could be isolated as the core category as well
for acceptance as for rejection of therapy recommendations.
Discussion
Theoretically, the reasons for non-adherence to therapy
guidelines can be divided into two different categories:
Deviation from the recommendations of the medical society
guidelines by the oncologist
Rejection of the physician-recommended treatment by the
patients themselves.
In this project, we looked for category B reasons for nonadherence,
and asked the patients why they rejected or
partially rejected a therapy recommended by their treating
oncologist. These reasons cannot be covered by medical society guidelines as they lie in the personal situation of the patients.
We performed qualitative interviews with older breast cancer
(>69 y, patient characteristics are shown in Table 1), as recent
studies have reported that, in this age group, guideline-based
therapy was more often lacking than in those with other cancers
[7,9,10]. Also, it has been shown that reduced therapy intensity
potentially reduces life expectancy of these older patients [15].
As compared to older studies on the same topic, where patient
satisfaction was the most recognized outcome measure [16],
we identified meaningfulness as the central category as well
for acceptance, as for rejection of therapy recommendations,
using the concept of Grounded Theory for the analysis of
the interviews with patients (Figure 1). Meaningfulness is a
central philosophical concept of solving problems, especially
under life-threatening conditions such as being ill with cancer.
In modern models, it can be seen as an ongoing process of
composing and recomposing one's life story through sharable
values [17], which might describe the patient's situation after
receiving the diagnosis of cancer. One of the major differences
between young and elderly cancer patients is that older people
can look back on their life stories. Thus, meaningfulness is a
guiding structure for making decisions about treatment and
is closely rooted in the personal life history of the patient.
Meaningfulness is not a static but a dynamic process defined
by a constant redefining of risks and benefits, which has also
been described as a process for decision making of women to
undergo prophylactic contralateral mastectomy [18].
In this concept, meaning and identity, or self, are closely
linked. Cancer diagnosis is a (potentially) destructive element
in patients' life stories. Agreement between doctor and patient
regarding treatment can only be expected if the patient not only
understands the treatment concept and its consequences but
is also able to integrate it into his/her personal life story. This
guiding structure for decision making can also be understood
as a method of preserving the self, that has been also found as
a process of decision making about hereditary breast cancer
and ovarian cancer risk reduction [19]. Some cancer survivors even report positive subjective changes they describe as "life
transforming" within the scenario of cancer diagnosis and
treatment [20].
Interestingly, three of the five axial coding categories underlying
patient decisions to accept or reject recommended therapies,
namely trust in doctor, comprehensive information and
explanation from the doctor, and addressing the living conditions
of the patient are within the doctor's sphere of influence (Table
1). The oncologist can establish a trustful relation with patients
by providing adequate information and answering questions
about disease and available treatments in terms intelligible to
them and by addressing their personal life situation. However, it
needs to be noted that despite such efforts to establish a trustful
relationship, patients might still decline recommended therapy.
On the one hand, whereas the gynecologist was the key medical
advisor for most patients, in two cases, the family doctor played
a decisive role in the rejection of gynecologist-recommended
therapy. These patients declined therapy when assured by the
family doctor that in rejecting the therapy, they were doing
the right thing. These conclusions are in agreement with the
findings of other studies. On the other hand, as pointed out by
Puts and colleagues, patients wanted as much information as
possible so that they can make therapy decisions that fitted into
their personal and unique life situation [21]. Thus, oncologists
need to accept the fact that their expertise, although taken into
account, is not the only source of information used by patients
in making therapy-related decisions: besides the internet, which
is being increasingly used also by patients of advanced age, our
interviews showed that information from the family doctor was
also taken into consideration [22].
These new perceptions again lead us back to the old knowledge
that the style of physician communication is a major factor in
treatment adherence [23]. Although it is known that patient
adherence to therapy is lower than suggested by oncologists
[24], the number of published studies evaluating the possible
reasons for this phenomenon is surprisingly low. Nevertheless,
it has been shown that physician communication is significantly positively correlated with patient adherence; a meta-analysis
has shown that there is a 19% higher risk of nonadherence
among patients whose physician communicates poorly than
among patients whose physician communicates well; training
physicians in communication skills results in substantial and
significant improvements in patient adherence [23]. We suggest
that future physician communication training should include the
factors that we analyzed in this project.
Further investigation of non-acceptance of treatment decisions
is needed. Even though the study reveals some reasons for nonacceptance,
no quantitative statements can be made based on
our findings. One factor that has been found in previous studies
was the wish to act independently especially in cancer patients
that are living alone, which is often the case in older patients in
the western countries [25]. The approach to integrate PROM/
PREM (patient-reported outcome and experience measures) into
clinical documentations, as cancer registries, is relatively new
and requires the development of relevant and focused survey
instruments. Studies like ours can help to include factors that are
relevant for the patients’ decision-making and experience before
and during therapy and hopefully overcome barriers to better
adherence to guideline-based treatment in elderly patients [26].
Strengths and limitations of the study
This study using the Grounded Theory approach addresses
the concept of meaningfulness of therapy in a population of
elderly breast cancer patients in the context of the individual
life situation of each patient. The strength of the study lies in its
qualitative approach. In contrast to quantitative studies, where
the possibilities of response are limited, open questions were
asked, which allowed patients to decide which aspects of the
issue were of importance to them. We reached a theoretical
saturation, which explains the small sample size. One limitation
is the focus on a selected group of patients with breast cancer
after their initial therapy; however, the overall message is
such that further work in this area is warranted. Furthermore,
the study might be a supplement to work addressing patientreported
outcomes (PRO).
Conclusion
We focused on a group of older cancer patients with breast
cancer, a group where treatment non-adherence is especially
high, and asked them what their reasons were for accepting
or rejecting the cancer therapy recommended by their treating
gynecologists. We found that advanced age played a decisive
role in patients' decisions: cancer and expectations from therapy
(negative as well as positive) were interpreted in the context of
their life stories, thus contributing significantly to the building
of an individual concept of meaningfulness. Awareness of
factors that are pivotal in the patients' decisions regarding
treatment can help doctors understand and respect refusal
of specific therapies or therapy components by patients and
might help in subsequent therapy planning. We suggest that
more studies on this subject are warranted and that physician
communication training should include the factors that have
emerged from this study, factors that are currently not part of
such training in medical curriculum. Awareness of the reasons
why patients reject the recommended therapy helps to reduce physician stress. In addition, these findings should be integrated
into the development of PRE/PRO as an integral part of clinical
documentation systems such as cancer registries.
Acknowledgement
The study was approved by the Ethics Committee of the
University of Luebeck (AZ 15-203). The project was funded
in part by the Gemeinsamer Bundesausschuss Germany,
Innovationsfond, DELIVER project. The original interviews
are stored on a password-protected disk. The hard disk is kept
by the project manager Frank Gieseler.
References
- Giordano SH, Hortobagyi GN, Kau SW, Theriault RL, Bondy ML (2005) Breast cancer treatment guidelines in older women. J Clin Oncol 23: 783-791.
- Salloch S, Ritter P, Wascher S, Vollmann J, Schildmann J (2014) Medical expertise and patient involvement: A multiperspective qualitative observation study of the patient's role in oncological decision making. Oncologist 19: 654-660.
- Sarrió RG, Rebollo MA, Garrido MM, Guillén-Ponce C, Blanco R, et al. (2018) General recommendations paper on the management of older patients with cancer: The SEOM geriatric oncology task force’s position statement. Clin Transl Oncol 20: 1246-1251.
- Chagpar R, Xing Y, Chiang YJ, Feig BW, Chang GJ, et al. (2012) Adherence to stage-specific treatment guidelines for patients with colon cancer. J Clin Oncol 30: 972-979.
- Schiphorst AH, Verweij NM, Pronk A, Hamaker ME (2014) Age-related guideline adherence and outcome in low rectal cancer. Dis Colon Rectum 57: 967-975.
- Sedjo RL, Devine S (2011) Predictors of non-adherence to aromatase inhibitors among commercially insured women with breast cancer. Breast Cancer Res Treat 125: 191-200.
- Baban CK, Devane L, Geraghty J (2018) Change of paradigm in treating elderly with breast cancer: Are we undertreating elderly patients? Ir J Med Sci Pp: 1-10.
- Barcenas CH, Zhang N, Zhao H, Duan Z, Buchholz TA, et al. (2012) Anthracycline regimen adherence in older patients with early breast cancer. Oncologist 17: 303-311.
- Derks MG, Bastiaannet E, Kiderlen M, Hilling DE, Boelens PG, et al. (2018) Variation in treatment and survival of older patients with non-metastatic breast cancer in five European countries: A population-based cohort study from the EURECCA Breast Cancer Group. Br J Cancer.
- Mislang AR, Biganzoli L, Brain E (2018) Systemic treatment of metastatic breast cancer in older adults. Geriat Oncol: 1-12.
- Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349-357.
- Helfferich C (2005) Die Qualität qualitativer Daten. Manual für die Durchführung qualitativer Interviews 2: 152-153.
- Coyne IT (1997) Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs 26: 623-630.
- Strauss AL (1987) Qualitative analysis for social scientists. Cambridge University Press.
- Wallwiener C, Hartkopf A, Grabe E, Wallwiener M, Taran FA, et al. (2016) Adjuvant chemotherapy in elderly patients with primary breast cancer: are women ≥65 undertreated? J Cancer Res Clin Oncol 142: 1847-1853.
- Ong LM, de Haes JC, Hoos AM, Lammes FB (1995) Doctor-patient communication: A review of the literature. Soc Sci Med 40: 903-918.
- Arciero G, Guidano VF (2000) Experience, explanation, and the quest for coherence. American Psychological Association, Constructions of disorder: Meaning-making frameworks for psychotherapy 13: 373.
- Rendle KA, Halley MC, May SG, Frosch DL (2015) Redefining risk and benefit: Understanding the decision to undergo contralateral prophylactic mastectomy. Qual Health Res 25: 1251-1259.
- Howard AF, Balneaves LG, Bottorff JL, Rodney P (2011) Preserving the self: The process of decision making about hereditary breast cancer and ovarian cancer risk reduction. Qual Health Res 21: 502-519.
- Skeath P, Norris S, Katheria V, White J, Baker K, et al. (2013) The nature of life-transforming changes among cancer survivors. Qual Health Res 23:1155-1167.
- Puts MT, Tapscott B, Fitch M, Howell D, Monette J, et al. (2015) A systematic review of factors influencing older adults' decision to accept or decline cancer treatment. Cancer Treat Rev 41: 197-215.
- Smith A (2014) Older adults and technology use. Pew Research Center.
- Zolnierek KB, Dimatteo MR (2009) Physician communication and patient adherence to treatment: A meta-analysis. Med Care 47: 826-834.
- Kirk, MC, Hudis CA (2008) Insight into barriers against optimal adherence to oral hormonal therapy in women with breast cancer. Clin Breas Can 8: 155-161.
- Benoot C, Deschepper R, Grypdonck M, Saelaert M, Bilsen J (2015) Acting independently while living alone: The strategies and struggles of cancer patients. Qual Health Res 25: 1033-1043.
- Wilson MK, Friedlander ML, Joly F, Oza AM (2018) A Systematic review of health-related quality of life reporting in ovarian cancer phase III clinical trials: Room to improve. Oncologist 23: 203-213.