Keller N1*, Schmid S1, Monod C2 and Haemmerle B1
1Department of Gynaecology and Obstetrics, Spital Grabs Hospital, Switzerland
2Department of Gynaecology and Obstetrics, University Hospital, Basel, Switzerland
*Corresponding Author:
Nicole Keller
Department of Gynaecology and Obstetrics
Spital Grabs Hospital, 9472 Grabs, Switzerland
Tel: +41 81 772 51 11
E-mail: nicole.claudia.keller@gmail.com
Received Date: November 18, 2017 Accepted Date: January 22, 2018 Published Date: January 24, 2018
Citation: Keller N, Schmid S, Monod C, Haemmerle B (2018) Aggressive Angiomyxoma of the perineum in a 50-year-old woman: Case Report and Current Level of Education. Gynecol Obstet Case Rep Vol.4:No.1:58. doi: 10.21767/2471-8165.1000058
Keywords
Aggressive angiomyxoma; Vulvovaginal region; Local recurrence rate
Introduction
Aggressive angiomyxoma is a very rare soft tissue mesenchymal neoplasm (only about 350 cases described in literature) [1], locally infiltrative with a tendency to repeated local recurrence. The first description was in 1983 [2]. It normally occurs in the vulvovaginal region, perineum and pelvis of females in reproductive age. It grows slowly as a painless solid mass with unclear boarders and the aggressive angiomyxoma often infiltrates the deep tissues. The growth can be expansive until the whole pelvic cavity is occupied [3]. Even if the tumor infiltrates the bladder, the rectum, the retroperitoneum, the pelvic bone or the levator ani muscle, the patients are often asymptomatic [4,5]. There are rare cases of aggressive angiomyxoma in the inguinoscrotal region of males and usually appear in older age [6]. This difference between males and females cannot be explained [7]. Other rare cases are described in children and perimenopausal women [5]. The female-to-male ratio is about 6:1 [8]. Metastases have been described in three cases. These distant metastases were all found in the mediastinum or lungs [9-11]. This suggests that aggressive angiomyxoma is not only a local disease. Wide local excision of the tumor is the primary management. The local recurrence rate is 25% to 47% after surgical excision [12]. The expression of estrogen and progesterone receptors in aggressive angiomyxoma and the growth of the tumor during pregnancy suggest a hormone dependency of the tumor [13]. Descriptions of drug treatment exist with gonadotropin-releasing hormone (GnRH) agonists in premenopausal women [14-17]. This locally aggressive tumor is a rare disease, therefore the state of knowledge how to treat patients with this soft tissue mesenchymal neoplasm is low.
Case Report
A 50-year-old woman reported first in 2013 with a painless swelling of 1.2 × 0.8 inches at the perineum. She underwent surgical excision. Pathologic findings reported the tumor as an aggressive angiomyxoma. The margins were not tumor-free. The patient did not appear to the follow-up examinations. In 2016 she reported again with a painless swelling of 0.8 × 0.8 inches at the perineum (Figure 1) and underwent a wide local excision. The tumor infiltrated the perineal tissue deeply and for the complete resection it was necessary to resect a part of the bulbocavernosus muscle and the soft tissue of the perineum above the rectum. Then the perineal body had to be reconstructed by the urogynecologist. To stabilize the distal part of the rectum a plication of the rectovaginal fascia, after preparing both sides, was necessary, followed by closing the posterior vaginal wall. The rebuilding of the perineal body consisted in mobilization of fatty tissue laterally from both sides. This tissue was used as an interposition layer to the perineal space. Finally, the perineal skin was closed.

Figure 1: Situation 3 years after the first operation.
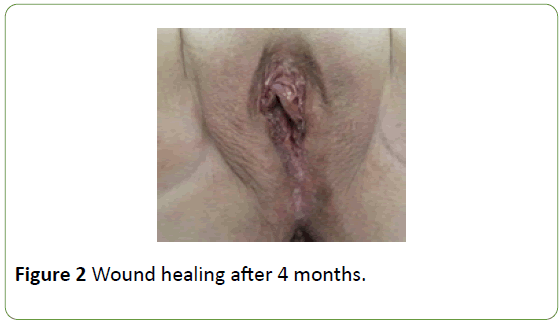
The wound healing was uneventful, resection margins were tumor-free and the immunohistochemical examination showed a hormonal receptor positivity of estrogen and progesterone and expression of CD31 and desmin. There was no expression of CD 34. For the result after 4 weeks (Figure 2). At follow-ups after 3 and 6 months there was no recurrence.
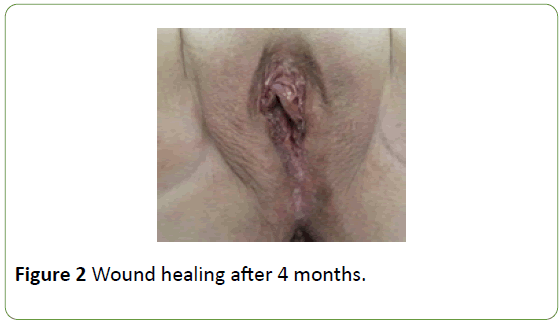
Figure 2: Wound healing after 4 months.
Discussion
Aggressive angiomyxoma is a very rare disease, which occurs primarily in young women in reproductive age. The initial presentation is often a painless, asymptomatic perineal or vulval nodule. Therefore, a clinical misdiagnosis is not unusual. The nodule can be mistaken as a lipoma, Bartholin’s or Gartner’s duct cyst, abscess or even as a malignant pelvic floor tumor. Because of the rarity of the aggressive angiomyxoma pre-operative diagnosis is difficult and a lot of cases are diagnosed on histological findings after the surgical excision [6,18].
Macroscopically the surface of the tumor is smooth and partially or completely encapsulated [6].
Microscopically the aggressive angiomyxoma is composed of many thick-walled vessels of varying size in a loose collagenous and myxoid stroma with spindle and stellate like cells [15]. Generally, the lesions show no cytologic atypia, no cell necrosis and a low mitotic activity [6].
There is no specific immunohistochemical marker for aggressive angiomyxoma and the most markers overlap with other mesenchymal lesions. Except for estrogen and progesterone receptors, there are other immunohistochemical markers, such as vimentin, desmin, SMA (smooth muscle actin), CD 34. But not all the cases are positive for these markers [7,19-21]. Genetic findings show a chromosomal abnormity involving chromosome 12, associated with rearrangement of the high mobility group A (HMGA2) gene. HMGA2 is an architectural transcription factor, which is important during embryogenesis. In adult tissues it is not usually detected. The pathogenesis of aggressive angiomyxoma is poorly understood [6,7,21-24]. Other benign mesenchymal lesions like uterine leiomyomas, endometrial polyps and other mesenchymal neoplasms have the same rearrangement of HMGA2 [19].
As diagnostics ultrasound and computerized tomography are nonspecific. In the ultrasound the neoplasm is usually a hypo echoic soft tissue mass and it could also appear as a cystic lesion [6]. In the computerized tomography the aggressive angiomyxoma appears variably as a homogenous hypo dense mass, cystic or even as a swirling solid mass. In magnetic resonance imaging the aggressive angiomyxoma is distinctive. On T1-weighted scans the mass is iso intense or hypo intense like muscle. On T2-weighted scans the tumors are characteristically hyper intense, except for their lower signal internal structure which looks swirled or layered. Magnetic resonance imaging is also helpful in planning the surgical excision with the aim of tumor-free margins [6,17,25,26].
All over the world the published number of cases is very small (about 350 cases) and so the interpretation of the data is often difficult. The first therapy is a wide local excision with the aim of tumor-free margins. But in the published data the influence of tumor-free margins is not clear. Complete resection is important, but when the operative morbidity is too high or the preservation of the fertility is necessary incomplete resection seems to be acceptable [8,18]. It is recommended to treat the tumor at an initial stage, when complete resection is possible. Wide surgical margins have the same influence on prognosis as narrow margins [8,17,27,28].
For a successful therapeutic concept, it is important to know if the tumor has positive estrogen and/or progesterone receptors. If both are negative, a hormonal treatment will not be successful and the surgical excision with, if necessary, preoperative arterial embolization is the best option. The tumors often have multiple feeding vessels, so it is difficult to succeed in embolization alone [8,17,29].
When the receptors are positive and the tumor is limited, the best therapeutic option is the surgical excision. If there is a residual disease after surgery, a hormonal treatment can be recommended. If the morbidity of the tumor resection is not tolerable, a neoadjuvant hormonal therapy is a feasible alternative with following surgical excision [17]. Descriptions of only drug treatment without surgery and with complete radiologic remission exist [16].
In the literature gonadotropin-releasing hormone (GnRH) agonists is the recommended hormonal treatment in premenopausal women. The response to gonadotropinreleasing hormone (GnRH) agonists varies, because the estrogen and progesterone receptors are not always strongly positive in aggressive angiomyxoma [15-18]. There exist no data of the optimal duration of the therapy [27]. A long-term therapy is not recommended because of the adverse effects like menopausal symptoms and bone loss. Often there is a recurrence of the tumor after discontinuing therapy. [17]. But until now it has not been shown that a long-term adjuvant therapy prevents the recurrence of the tumor [1].
In postmenopausal women aromatase inhibitors are preferred in estrogen positive aggressive angiomyxoma [30]. Hormone replacement therapy should be stopped [17].
In the exceptional situation of non-operable tumor without response to embolization or hormonal treatment radiation therapy can be considered [27].
The low mitotic activity of the tumor is the reason why radiation therapy or chemotherapy are not really successful [19,23].
A deep infiltration of the perineal tissue requires a resection of a part of the bulbocavernosus muscle and the soft tissue of the perineum above the rectum to get a complete resection of the tumor, followed by reconstruction of the perineal body. To get an acceptable functional result the pelvic floor reconstructive surgery is to be done by a urogynecologist. Knowledge of gynaecologic oncology is also useful in the management of aggressive angiomyxoma. A multimodal, interdisciplinary approach is pivotal to minimize the recurrence rate in combination with a low morbidity. This concerns clinical examination, imaging, surgery, adjuvant treatment and follow-up.
Conclusion
Aggressive angiomyxoma is a rare disease, but when treating women with a painless swelling in the vulvovaginal region, perineum or pelvis aggressive angiomyxoma should be considered as a differential diagnosis. There is no standardised surgical or pharmacologic procedure described, but complete resection seems to be crucial. A multimodal approach is important. Even tumor-free margins do not prevent a recurrence [5,19,31]. There is no established relation between the size of the tumor, the patient’s age and the risk of recurrence [8].
Long-term follow-up is important because of repeated local recurrence. Clinical examination and radiological imaging, especially magnetic resonance imaging is recommended [13,25].
Disclosure and Conflict of Interest
• All authors of this paper have directly participated in the planning, execution analysis of the study. They have read and approved the final version submitted.
• The contents of the manuscript have not been copyrighted or published previously and are not now under consideration for publication elsewhere. There are no directly related manuscripts or abstracts, published or unpublished, by any author(s) of this paper.
• There was no financial support for our research.
References
- Im SW, Han SS (2016) Treatment of aggressive angiomyxoma of the female perineum: Combined operative and hormonal therapy. J Obstet Gynaecol 36: 819-821.
- Steeper TA, Rosai J (1983) Aggressive angiomyxoma of the female pelvis and perineum. Report of nine cases of a distinctive type of gynecologic softtissue neoplasm. Am J Surg Pathol 7: 463-475.
- Chen LM, Schink JC, Panares BN, Barbuto D, Lagasse LD (1998) Resection of a giant aggressive angiomyxoma in the Philippines. Gynecol Oncol 70: 435- 439.
- Sun Y, Zhu L, Chang X, Chen J, Lang J (2017) Clinicopathological features and treatment analysis of rare aggressive angiomyxoma of the female pelvis and perineum - a retrospective study. Pathol Oncol Res 23: 131-136.
- Ribaldone R, Piantanida P, Surico D, Boldorini R, Colombo N, et al. (2004) Aggressive angiomyxoma of the vulva. Gynecol Oncol 95: 724-728.
- Haldar K, Martinek IE, Kehoe S (2010) Aggressive angiomyxoma: A case series and literature review. Eur J Surg Oncol 36: 335-359
- Nucci MR, Fletscher CDM (2000) Vulvovaginal soft tissue tumours: Update and review. Histopathology 36: 97-108
- Chan IM, Hon E, Ngai SW, Ng TY, Wong LC, et al. (2000) Aggressive angiomyxoma in females: Is radical resection the only option? Acta Obstet Gynecol Scand 79: 216-220.
- Siassi RM, Papadopoulos T, Matzel KE (1999) Metastasizing aggressive angiomyxoma. N Engl J Med 341: 1772-1773.
- Blandamura S, Cruz J, Faure Vergara L, Machado Puerto I, Ninfo V (2003) Aggressive angiomyxoma: a second case of metastasis with patient‘s death. Hum Pathol 34: 1072-1074.
- Geng J, Cao B, Wang L (2012) Aggressive angiomyxoma: An unusual presentation. Korean J Radiol 13: 90-93.
- Sutton B J, Laudadio J (2012) Aggressive angiomyxoma. Arch Pathol Lab Med 136: 217-221.
- Orfanelli T, Kim CS, Vitez SF, Van Gurp J, Misra NA (2016) Case report of aggressive angiomyxoma in pregnancy: Do hormones play a role? Case Rep Obstet Gynecol.
- Palomba S, Oppedisano R, Annunziata G, Zullo F, Amorosi A (2011) Leuprolide acetate depot plus high-dose raloxifene hydrochloride before and after surgery for reccurent vaginal aggressive angiomyxoma: A case report. Gynecol Oncol 123: 172-173.
- McCluggage WG, Jamieson T, Dobbs SP, Grey A (2006) Aggressive angiomyxoma of the vulva: Dramatic response to gonadotropin-releasing hormone agonist therapy. Gynecol Oncol 100: 623-625.
- Fine BA, Munoz AK, Litz CE, Gershenson DM (2001) Primary medical management of recurrent aggressive angiomyxoma of the vulva with a gonadotropin-releasing hormone agonist. Gynecologic Oncology 81: 120-122.
- Schwartz PE, Hui P, Mc Carthy S (2014) Hormonal therapy for aggressive angiomyxoma: A case report and proposed management algorithm. J Low Genit Tract Dis 18: E55-E61.
- Pereira P, Melo Abreu E, Cunha TM, Rolim I (2017) Transperineal aggressive angiomyxoma. BMJ Case Rep.
- Magtibay PM, Salmon Z, Keeney GL, Podratz KC (2006) Aggressiv angiomyxoma of the female pelvis and perineum: A case series. Int Gynecol Cancer 16: 396-401.
- Sengupta SK, Bhattacharyya SK, Saha SP, Roy H, Sarkar AN (2014) Recurrent aggressive angiomyxoma of the vulva- A rare presentation. J Clin Diagn Res 8: OD01-OD02.
- McGluggage WG (2009) Recent developments in vulvovaginal pathology. Histopathology 54: 156-173.
- Nucci MR, Weremowicz S, Neskey DM, Sornberger K, Tallini G, et al. (2001) Chromosomal translocation t (8; 12) induces aberrant HMGIC expression in aggressive angiomyxoma of the vulva. Genes Chrom Cancer 32: 172-176.
- Choi H, Park C, Ji YI (2015) Alternative surgical approaches for aggressive angiomyxoma at different sites in the pelvic cavity. Obstet Gynecol Sci 58: 525-529.
- Rabban JT, Dal Cin P, Oliva E (2006) HMGA2 rearrangement in a case of vulvar aggressive angiomyxoma. Int J Gynecol Pathol 25: 403-407.
- Jayadevan NN, Shoaib SAA (2002) Imaging features of aggressive angiomyxoma. Clinical Radiol 58: 157-162.
- Li X, Ye Z (2011) Aggressive angiomyxoma of the pelvis and perineum: A case report and review of the literature. Abdom Imaging 36: 739-741.
- Han-Geurts IJ, van Geel AN, van Doorn L, den Bakker M, Eggermont AM (1995) Aggressive angiomyxoma: multimodality treatments can avoid mutilating surgery. Eur J Surg Oncol 32: 1217-1221.
- Jineping Z, Chunfu Z (2010) Clinical experience on aggressive angiomyxoma in China (report of 93 cases). Int J Gynecol Cancer 20: 303-307.
- Nyam DCK, Pemberton J (1998) Large aggressive angiomyxoma of the perineum and pelvis: An alternative approach. Disease of the Colon and Rectum 41: 514-516.
- Chen H, Zhao H, Xie Y, Jin M (2017) Clinicopathological features and differential diagnosis of aggressive angiomyxoma of the female pelvis: 5 case reports and literature review. Medicine (Baltimore) 96: e6820.
- Poirier R, Fraser R, Meterissian S (2003) Unusual abdominal and pelvic tumor: Case 1. Aggressive angiomyxoma of the pelvis: Response to luteinizing hormone-releasing hormone agonist. J Clin Oncol 21: 3535-3536.