- (2013) Volume 14, Issue 2
Vassilis S Ramfidis1, Konstantinos N Syrigos2, Muhammad Wasif Saif3
1Oncology Unit, 251 General Hospital of Airforce. Athens, Greece.
2Oncology Unit, Third Department of Medicine, University of Athens, Sotiria General Hospital. Athens, Greece.
3Department of Medicine and Cancer Center, Tufts Medical Center. Boston, MA, USA
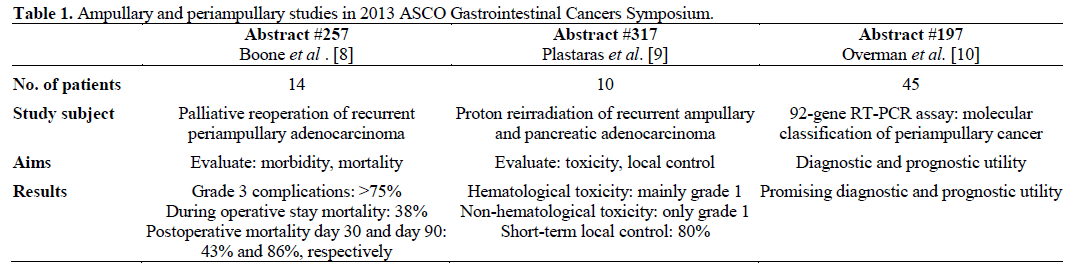
The mainstay treatment of ampullary and periampullary adenocarcinoma is pancreaticoduodenectomy. Unfortunately, there are no standard options available in the postoperative management due to the rarity of the malignancy and the absence of prospective trials. In this year ASCO Gastrointestinal Cancers Symposium three remarkable abstracts regarding the management of recurrent or metastatic ampullary and periampullary carcinoma were presented. The first study (Abstract #257) demonstrates that palliative reoperation should not be an option, because of its severe morbidity and high mortality. The second study (Abstract #317) supports that reirradiation is well tolerated and it could be used for palliative reasons and local control. The last study (Abstract #197) reveals the prognostic value of 92-gene RT-PCR assay and the authors support the use of this method for the management of metastatic periampullary adenocarcinoma when the primary pathological sample cannot be helpful.
Adenocarcinoma; Ampulla of Vater; Bile Duct Neoplasms; Pancreatic Neoplasms; Radiotherapy
Ampullary carcinoma is a malignant tumor arising from the ampulla of Vater representing 2% of all gastrointestinal malignancies and 20% of all tumors of the extrahepatic biliary tree and it can be difficult to be distinguished from other periampullary tumors preoperatively [1]. Periampullary cancer may originate from the pancreas, duodenum, distal common bile duct, or the structures of the ampullary complex and it seems to have a worst prognosis than primary ampullary malignancies [2, 3, 4].
The mainstay treatment of ampullary carcinoma is pancreaticoduodenectomy. Unfortunately, there are no standard options available in the postoperative management due to the rarity of the malignancy and the absence of prospective trials. The therapeutic array in the adjuvant setting includes adjuvant chemotherapy or chemo-radiation therapy based largely on the data extrapolated from pancreas clinical trials and retrospective data [5, 6]. In case of recurrence or metastatic disease the data are even more limited and debatable. In recurrent disease, first-line chemotherapy with gemcitabine and cisplatin is widely accepted but with no strong level of evidence [7]. Moreover, there are no studies with evaluated outcomes concerning palliative approach and local control.
In this year’s ASCO GI Cancers Symposium three remarkable abstracts regarding the management of recurrent or metastatic ampullary and periampullary carcinoma were presented. The purpose of this paper is to present the data and the main findings of these studies as shown collectively in Table 1. The incorporation of the new data on a patient approach algorithm is illustrated in Figure 1.
Palliative Reoperation and Its Role in Recurrent Periampullary Carcinoma (Abstract #257) [8].
Boone et al. conducted a retrospective study to evaluate the role of reoperation in patients with recurrent periampullary carcinoma. A total of 14 patients who have undergone prior resection were recruited and underwent palliative reoperation because of symptomatic recurrence. The morbidity and mortality were examined during a period of 90 days. The postoperative morbidity was remarkable high. Complications (mainly grade 3) occurred to 8 patients and intraoperative mortality was 21.4%. Postoperative mortality reached 86% with median survival 45 days. Bigger interval between prior resection and reoperation seemed to be correlated with improved median survival.
The study therefore demonstrates that reoperation for palliative reasons are not recommended for these patients due to the severe morbidity and high percentage of lethal outcomes.
Proton Reirradiation as a Local Control Treatment of Recurrent Ampullary Adenocarcinomas (Abstract #317) [9].
Proton reirradiation seems to have a role in the management of locally recurrent ampullary or pancreatic adenocarcinoma after resection and chemoradiation according to a study by Plastaras et al. The eligible patients with locally recurrent disease were 10 and underwent proton reirradiation (median total dose 50.4 Gy). Among them, a total of 9 patients also received concurrent chemotherapy with 5- fluororacil or capecitabine-based chemotherapy. The aim of the study was to examine the toxicity and the ability of local control. The follow up lasted 8.2 months. The toxicity profile was manageable with grade 1 or less non-hematological RT-related toxicity and mainly grade 1 hematological toxicity. Furthermore, the majority of the patients (80%) did not develop progressive disease within the retreated fields, revealing the potential role of reirradiation concerning the local control. Half of the patients developed metastatic disease with a median progression free survival of 7.4 months after starting radiotherapy and only one patient died during the period of the follow up.
This study supports that reirradiation is well tolerated and it could be used for palliative reasons and local control.
92-Gene RT-PCR: Its Role in Molecular Classification of Periampullary Adenocarcinomas and Its Prognostic Significance (Abstract #197) [10].
One worth mentioning abstract, investigating the efficacy of 92-gene RT-PCR assay to categorize periampullary adenocarcinomas and its prognostic significance, was selected for publication at the 2013 ASCO Gastrointestinal Cancers Symposium. In this study, a total of 45 patients who underwent complete resection of the primary tumor were recruited. Histopathological determination was verified and at the same time, tumor sections were molecularly classified by using a 92-gene RT-PCR assay. The samples that were molecularly classified were compared with histopathological types showing 91% concordance. Moreover, the evaluation of all periampullary samples revealed the prognostic value of the 92-gene assay by showing a median overall survival of 70 months for intestinal and gastroesophageal cases versus 32 months for pancreaticobiliary cases (P=0.05). Furthermore, and more specifically for the ampullary samples, the better prognosis of intestinal subgroup vs. the pancreaticobiliary subgroup was also verified by the 92-gene assay showing a median overall survival of 63 months versus 24, months respectively (P=0.07).
The study reveals the prognostic value of 92-gene PCR assay and the authors support the use of this method for the management of metastatic periampullary adenocarcinoma when the primary pathological sample cannot be helpful.
Despite the enormous advances in clinical research in oncology, the data of therapeutic approach of recurrent ampullary and periampullary adenocarcinomas remains limited. The rarity of this type of malignancy and the fact that patients with ampullary carcinoma quite often participate in clinical trials for pancreas or biliary tract cancers, explain the scarce knowledge.
In this year’s ASCO Gastrointestinal Cancers Symposium the role of palliative reoperation for recurrent periampullary adenocarcinoma were examined and, according to the authors of the study, palliative surgery should not be considered as a potential option, due to its severe morbidity and mortality. On the other hand, the Plastaras et al. study showed promising results about the role of radiotherapy. Irradiation of locally recurrent ampullary cancer is well tolerated and it seems that it could control local disease. Finally, molecular approach of periampullary cancer by using a 92-gene PCR assay could be used for categorization of this type of cancer and prognostic stratification.
In conclusion, the main findings of ampullary and periampullary adenocarcinoma management from the 2013 ASCO Gastrointestinal Cancers Symposium studies presented above should be interpreted with caution because of the small number of patients that participated, but allow optimism. New prospective, large, randomized trials should be done to confirm these results and the enrollment of patients in future trials must be encouraged.
The authors have no conflicts to disclose