- (2007) Volume 8, Issue 1
Fung J Foo1, Upkar Gill1, Caroline S Verbeke2, James A Guthrie3, Krishna V Menon1
Departments of 1Hepatobiliary Surgery, 2Histopathology, and 3Radiology, St James’s University Hospital. Leeds, United Kingdom
Received November 4th, 2006 - Accepted November 13th, 2006
Context Annular pancreas is an uncommon congenital abnormality. Co-existence of this condition with a pancreaticobiliary malignancy is an exceptionally rare occurrence. Case report We present a case report of a 78- year-old woman with jaundice due to an ampullary carcinoma associated with an annular pancreas treated by pancreaticoduodenectomy. Conclusions A collection of previously reported cases is reviewed together with the relevant literature. Obstructive jaundice is an uncommon feature of annular pancreas; hence the possibility of co-existent pancreaticobiliary malignancy should be excluded. INTRODUCTION Annular pancreas
Adenocarcinoma; Ampulla of Vater; Jaundice, Obstructive; Pancreas /abnormalities, /embryology; Pancreatic Neoplasms
PD: pancreaticoduodenectomy; PPPD: pylorus preserving pancreaticoduodenectomy, TP: total pancreatectomy
Annular pancreas was first described by Tiedemann in 1818 and is due to malrotation of the pancreatic ventral bud during embryological development [1]. Popular theories explaining the pathogenesis include adhesion of the right ventral bud to the anterior duodenal wall [2] and failure of the left ventral bud to in volute [3]. This congenital anomaly is a rare occurrence. In 20,000 autopsies only three were discovered [4], while a review of 22,243 surgical cases demonstrated only a single one [5]. Coexistence of annular pancreas with pancreaticobiliary malignancy is therefore exceptionally rare and hence only few cases have been reported. We report a case of ampullary adenocarcinoma in a patient with an annular pancreas.
A 78-year-old woman presented with epigastric pain radiating into her back, made worse on eating. She had no significant comorbidity. Laboratory investigations were unremarkable apart from abnormal liver functions with raised total bilirubin (67 μmol/L; reference range: 5-21 μmol/L), ALT (42 IU/L; reference range: 0-40 IU/L) and alkaline phosphatases (719 IU/L; reference range: 70-300 IU/L). Tumour markers CEA and CA 19-9 were normal.
ERCP revealed an enlarged and protuberant ampulla of Vater. This was biopsied and reported as tubulo-villous adenoma with high grade dysplasia. An abdominal CT scan demonstrated marked intra- and extrahepatic bile duct dilation. The common bile duct was dilated to 2 cm (Figure 1) down to the level of the ampulla where a 2 cm tumour was noted (Figure 2). There was no evidence of distant disease or contraindications to a curative resection.
The patient underwent a pancreaticoduodenectomy. Findings were of a complete annular pancreas wrapping around the duodenum 5 cm distal to the pyloric sphincter. There was a palpable tumour in the ampullary region. The resection was performed without any complications and after an uneventful recovery the patient was discharged home on the tenth post operative day.
Gross pathological examination confirmed the presence of a complete annular pancreas with pancreatic parenchyma wrapping around and narrowing the duodenum over a length of 2.5 cm (Figure 3). With the exception of minimal pancreatic duct dilatation, histology of the annular pancreas was normal and there was no evidence of inflammation or pancreas divisum. The ampulla of Vater was occupied by a 1.2x3.5 cm polypous tumour (Figure 4). Histology demonstrated a papillary adenoma of intestinal type showing severe dysplasia. In addition, there was a focus of well differentiated adenocarcinoma, which was confined to the fibromuscular layer of the ampulla. The tumour stage was pT1 N0 V0 R0 and hence no adjuvant treatment was indicated.
Annular pancreas has a bimodal pattern of presentation, the first peak is in infancy and a later peak occurs in the fourth decade of life. The proportion of patients treated for annular pancreas is split equally between the two age groups. However, both have very different clinical pictures. Paediatric cases usually present with gastrointestinal obstruction or jaundice. Associated conditions include mongolism, intestinal malrotations, duodenal atresia/stenosis/webs, tracheoesophageal fistulas and cardiac defects [6].
Presentation in adulthood is rare, although annular pancreas is now identified with increasing frequency because of more liberal use of abdominal CT, ERCP and MRCP. Adult annular pancreas is associated with duodenal obstruction (60%) [6], pancreatitis (15-50%) and peptic ulceration (26-48%) [7]. Obstructive jaundice is an uncommon feature and not usually a direct result of the annular pancreas. Morrell and Keynes reported on 15 annular pancreas patients with jaundice and causes included pancreatitis (10 cases), choledocholithiasis (4 cases) and alcoholic liver disease (1 case) [8]. A series of 135 adult annular pancreas cases revealed only one case with biliary obstruction due to the pancreatic annulus [6].
Later work in the Japanese literature started to elude attention to co-existent pancreaticobiliary malignancy as a cause of the obstructive jaundice or as an association in annular pancreas patients. A review by Yogi et al. of 105 annular pancreas patients revealed nine with obstructive jaundice due to ampullary carcinoma (5 cases), pancreatic carcinoma (2 cases) and cholangiocarcinoma (2 cases) [9]. A subsequent collection of 151 cases of annular pancreas by Ogawa et al. revealed 15 had pancreaticobiliary malignancy, including 5 cholangiocarcinomas, 4 gallbladder carcinomas, 4 duodenal and 2 pancreatic carcinomas [10]. Hence, clinical presentation of annular pancreas with obstructive jaundice is rare and should alert the clinician to the possibility of another cause such as underlying malignancy.
Including ours, there are 14 cases of carcinoma associated with annular pancreas in the English literature (Table 1) with the first published in 1982 [10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21]. There were eight female and six male patients with ages ranging from 40 to 88 years. Seven of the 14 patients were of oriental ethnicity. The most common presenting symptoms were jaundice (11 cases), upper abdominal pain (7 cases) and weight loss (4 cases).
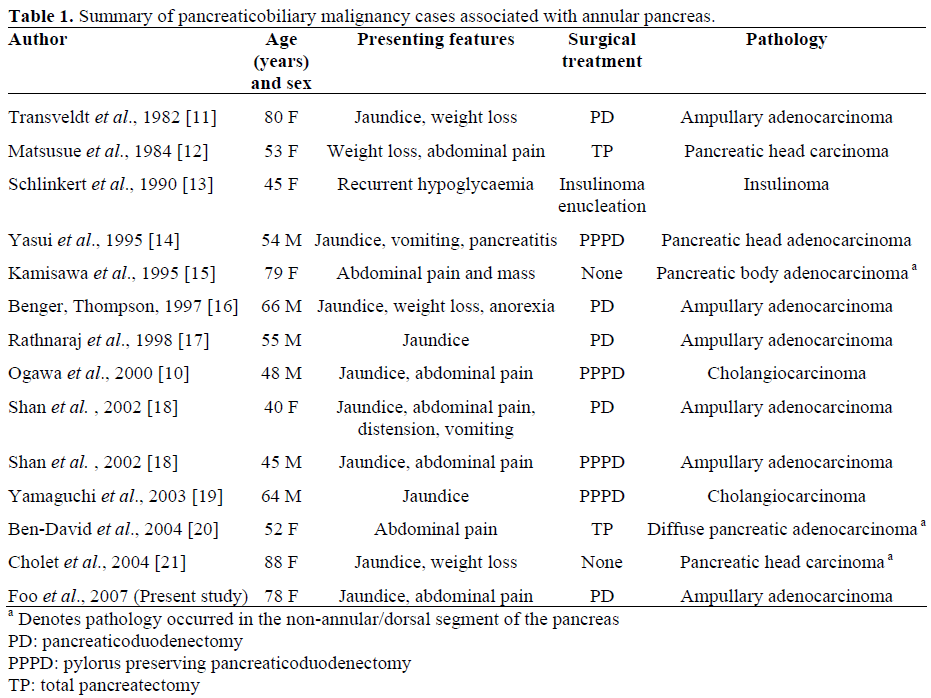
Biochemical investigations revealed jaundice and deranged liver function tests in 85% of patients. Tumour markers were poor indicators with positive predictive values of only 50% and 57% of the time for CEA and CA 19.9 respectively.
Annular pancreas was diagnosed preoperatively in 6 cases mostly by means of ERCP. CT was poorly sensitive and failed to detect annular pancreas in 10 out of 13 times performed. Diagnosis of annular pancreas on CT and MRI is obtained by visualisation of pancreatic duct and parenchyma surrounding the duodenum. However, this is difficult without adequate thickness of the pancreatic parenchyma. ERCP is more sensitive, providing a definitive diagnosis by visualisation of the pancreatic duct encircling the duodenum, but this investigation has attributed risks. MRCP and endoscopic ultrasound have been found to be less invasive alternatives which can also diagnose a co-existent malignancy [19].
Amongst the cases reported in the English literature, the most commonly occurring cancer in the annular pancreas was ampullary carcinoma (6 cases). Others included pancreatic head carcinoma (3 cases), cholangiocarcinoma (2 cases), pancreatic body adenocarcinoma (1 case),diffuse pancreatic carcinoma (1 case) and insulinoma (1 case) [10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21]. The malignancy usually involved the annular (ventral) segment of the pancreas. This has been attributed to chronic inflammatory changes in this area associated with pancreatitis. There were only three reports of cancer occurring in the non-annular (dorsal) segment [15, 20, 21]. Surgical treatment of pancreaticobiliary malignancy in the annular pancreas was similar to that in the non-annular pancreas.
Annular pancreas presenting with obstructive jaundice is a rare occurrence. The possibility of a co-existent underlying malignancy of the pancreaticobiliary system should always be considered in the management of the patient.