Keywords
cancer nursing, post-registration
courses, recruitment of black and minority ethnic
nurses, workforce planning
Introduction
The initiative for this study came from the chief nurse
and deputy chief executive of an NHS trust
specialising in cancer nursing services. There was
concern at the apparently low numbers of black and
minority ethnic (BME) nurses applying for trust-sponsored places on the cancer nursing educational
programmes. The trust has a long history of initiating
and providing specialist post-qualifying cancer nursing
courses. Recruitment to the educational programme
includes encouraging those employed by the trust to apply for a sponsored place, and through
external advertisements in nursing journals. The package
for successful candidates includes appointment
on a permanent work contract as a staff nurse, payment
of tuition fees, provision of accommodation and full
study leave. The selection criteria require that the
applicant has at least one year’s nursing experience,
which ideally includes six months caring for cancer
patients, although exceptions may be considered.
Prospective candidates without such experience have
the option of joining the Dgrade rotation programme
of the trust, with a guarantee that they will be considered
for a sponsored place on the course.
Blackand minority ethnic nurses
in cancer care
The UK Department of Health recognises that nurses
play a crucial role in the national cancer programme,
and has highlighted the need to increase the cancer
nursing workforce. An inadequate number of nurses
has undertaken specialist cancer education (Department
of Health/National Health Service Executive,
2000). However, in discussing the shortage of nurses
within the NHS, no reference is made to BMEnurse s’
contribution to cancer care. In contrast, the national
nursing strategy Making a Difference (Department
of Health, 1999) stated that there is still considerable
scope to ‘secure equality of access to education, development
and career advancement for nurses, midwives
and health visitors from black and ethnic minority
groups’.
Recruitment of BME students to
pre- and post-registration
nursing programmes
Iganski et al (1998) analysed all 54 194 applications to
pre-registration nursing programmes stored in the
former English National Board for Nursing, Midwifery
and Health Visitors (ENB) admissions database
between October 1993 and September 1996. They
reported that minority ethnic applicants were less
likely than white applicants to have been offered a
place, and that a higher proportion was rejected
without an interview. This could not be explained by
variables such as qualification level, the specialty
chosen or age. Mahoney (2001), in a follow-up study,
found that 34% of both white and black Caribbean
applicants secured a place, compared to just 17% of
African candidates. There were also substantial differences
between various colleges of nursing in this regard. Consequently, the educational consortia of
the time were advised to: ‘give particular attention
to considering ways of encouraging people from
ethnic minority communities (many of whom live in
the areas of greatest shortage) into nursing and other
professions, and fostering a climate in the NHS which
encourages them to stay’ (NHS Executive, 1997).
Equality of access to post-registration nursing education
and training is cited as a significant feature of
the policy to improve care delivery (Audit Commission,
2001). Baxter (1988) reported that BMEstaff
encountered difficulties in accessing training in
higher-status and more popular areas of work. A study
conducted in Birmingham (Klem and Notter, 2001)
involved interviewing 164 health practitioners (nurses
and allied health professionals), of whom 92 (56%)
were from BMEcommuni ties. Of the reported incidents
of perceived racial discrimination, 7% were in
education and 16% in respect to promotion. Other
research that provided similar evidence includes the
Commission for Racial Equality (1987), the King’s
Fund (King’s Fund Equal Opportunities Task Force
(KFEOTF), 1990), the Policy Studies Institute (Beishon
et al, 1995) and the English National Board for Nursing,
Midwifery andHealthVisiting (ENB) (Gerrish et al,
1996; Iganski et al, 1998).
Beishon et al (1995) identified that little monitoring
of applicants’ post-registration education was carried
out by NHS trusts, and Iganski et al (1998) noted a
similar situation in colleges of nursing and midwifery.
The King’s Fund (KFEOTF, 1987) included recommendations
such as mandatory equal opportunity
training for those involved in recruitment, and avoiding
the use of informal visits, unsolicited references and
patronage. The ENB (1998) undertook an audit of
ethnic monitoring systems in colleges of nursing and
midwifery, but this only covered pre-registration
programmes. In respect of qualified NHS staff, the
Audit Commission (2001) noted that ‘the potential
for discrimination exists when appraisal and the
identification of individual training needs is patchy
and unsystematic. Therefore, it is important that
trusts monitor appraisal/PDP [personal development
planning] coverage, and application for and uptake of
training opportunities in relation to ethnic origin’.
Career development of BME
nurses
The Policy Studies Institute explored the experiences
of BMEnurs es and midwives (Beishon et al, 1995).
The survey comprised:
1 a qualitative study of six case study nurse employers
across the country, involving interviews with 114 qualified and unqualified staff, 60 with white staff
and 54 with ethnic minority staff
2 a national postal survey of 23 251 nursing and
midwifery staff with 14 330 (62%) completing the
questionnaire.
While the data suggested that minority ethnic groups
were well represented in the higher grades, a more
detailed statistical analysis identified that it took some
groups (particularly black nurses) a much longer time
to reach those grades, regardless of similar qualifications
and experience. Findings identified a big gap between
theoretical policies on equal opportunities, such as in
recruitment and promotion, and the actual practices
undertaken on the ward and in other workplaces.
The Race Relations (Amendment) Act 2000 gives
public authorities, such as NHS trusts and higher
education institutes (HEIs), a general duty to promote
race equality. To help public authorities meet this
general duty, the Home Secretary has made an order
(under the Act) that gives them specific duties in
policy, service delivery and employment. As an example
of the latter, they are obliged tomonitor by ‘racial group’:
staff in post; and applicants for jobs, promotion and
training (Commission for Racial Equality, 2002).
The NHS Plan (Department of Health, 2000a)
reinforced the need for NHS trusts to demonstrate
that their procedures for recruitment, development
and promotion should be demonstrably fair and to
encourage BMEstaff to develop their careers within
the NHS. More recently Sir Nigel Crisp, the former
Chief Executive of the NHS, issued a 10-point Race
Equality Action Plan (Department of Health, 2004),
and reiterated that the NHS must target recruitment
and development opportunities for people from different
ethnic groups ‘whose skills are often underused’.
Recruitment of BME nurses into
cancer services
The representation of BMEnurses in cancer services
would appear to be a workforce planning issue. However,
in an analysis of the evidence base Richardson
et al (2001) commented that ‘Despite the importance
of an effective and efficient cancer nursing workforce
in ensuring cost-effective and positive patient outcomes,
the evidence available on which to base organisational
decisions is so weak as to be almost non-existent’. In
their review of current practices Richardson et al
(2002) noted that ‘There is still much to be achieved,
primarily in the areas of workforce planning, the skill
development of non-specific nurses, and research and
development’.
A search of the literature (using CINAHL and
MEDLINE databases) identified a dearth of research on BMEnurse s in cancer care, but several studies
highlighted the value of their presence in the workforce.
For example, Thomas et al (2000), in their study
on the efficacy of bilingual health advocacy in an inner
London cancer centre, reported that all the healthcare
professionals interviewed experienced communication
difficulties due to language and cultural barriers.
Olsen and Frank-Strombourg (1994) undertook a
survey of African-American nurses applying for participation
in a workshop organised by the National
Cancer Institute and Oncology Nursing Society. They
concluded that African-American nurses favourably
influence cancer prevention and screening beliefs and
practices for African-American clients. In addition,
ethnic and cultural appropriateness of care can be
positively influenced by shared values and beliefs
between nurses and service users.
CancerLink has recommended that ‘Management
and care staff at all levels should broadly reflect the
local population including black and minority ethnic
groups. There should be regular training to raise
awareness and promote discussion about the needs
of black and minority ethnic people’ (ScanLink, 1996).
In the UK, the results of a national survey of over
65 337 patients with cancer from over 170 NHS trusts
(Airey et al, 2002) are of interest: 2% (n = 1307)
classified themselves as other than white; of these, half
were black and one-third South Asian and nearly half
were in the London region. Thirty-six percent of black
and 42% of South Asian patients said that they did not
have confidence in all nurses, compared with 27% of
all patients (Airey et al, 2002).
In a postal survey of doctors and nurses at the Royal
Marsden NHS Trust Aspinall et al (2002) found that
one of the most frequently mentioned single measures
thought to best contribute to improving access for
BMEpopulations was a wider use of staff fromminority
ethnic groups in a range of roles.
It was disappointing that an evaluation of the
Macmillan Lead Cancer Nurse Initiative (Booth et al,
2001) gave no information about the ethnic group of
the respondents based in 12 sites, nor did it discuss
representation of BMEnurse s within cancer care. It is
also regrettable that the Royal College of Nursing
(RCN) makes no mention of BMEnurses in cancer
services in its framework for adult cancer nursing
(RCN, 2003).
Conduct of the study
The aims of the study were to:
• describe the ethnic group profiles of those applying
and of those accepted for an NHS trust-sponsored
place on cancer nursing courses between September
1999 and September 2002
• elicit the views of students in the September 2001
and 2002 cohorts concerning recruitment and
retention into cancer care of both white and BME
nurses.
The survey used a postal questionnaire that was
designed to find out the views of students concerning
issues relating to white and BMEnurses undertaking
cancer care nursing. The course organiser provided a
profile of the students undertaking the courses. Following
approval from the local NHS trust research
ethics committee, the study was undertaken between
April 2001 and December 2002.
The timeframe for the study period allowed the
purposive recruitment of students in two cohorts.
While there were an initial 48 students in the first
cohort that commenced in September 2001, there
were only 43 remaining at the time the questionnaire
was distributed. In the second cohort, all 37 students
that started in September 2002 were approached to
participate in the study.
The questionnaire design was kept simple but
focused. Closed and open-ended questions were
generated to target responses to the issues being
studied (de Vaus, 2001). Information about personal
and professional profiles, motivation to do cancer
nursing, sources of information about the course
and the outcome of the recruitment process were
requested. Respondents were also asked their views
about career prospects in cancer nursing, possible
barriers to recruitment and retention of cancer nurses,
both white and BME.
Questionnaires, together with an information sheet,
invitation letter and consent form and a stamped
addressed envelope were sent out to the remaining
43 students of cohort 1 in April 2001, and to the 37
cohort 2 students in November 2002. A reminder was
sent to non-responders within two weeks. The responses
rate of the two cohorts combined was 30
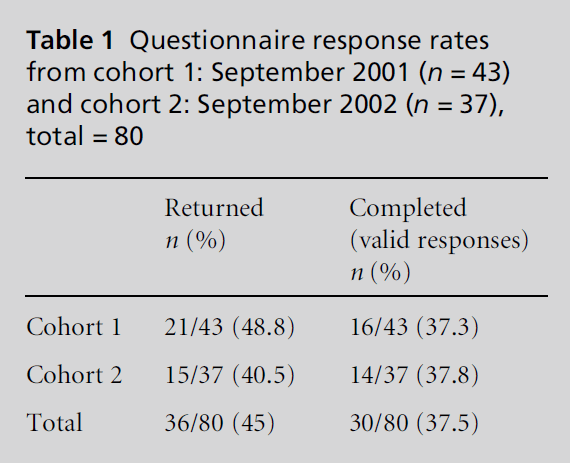
(37.5 %) with full details set out in Table 1.
Statistical data analysis was carried out using the
SPSS version 10 software package. Descriptive statistics, including frequency and percentage distribution,
together with the range and mean values were calculated
for some numerically coded variables (Punch,
1998). The small numbers in the study did not allow
differences in BMEnum bers across cohorts to be
subjected to inferential statistical analysis. Analysis
of the written responses to open-ended questions was
carried out using a thematic analysis approach, with
coding and categorisation of data and generation of
themes (Punch, 1998).
Table 1: Questionnaire response rates
from cohort 1: September 2001 (n = 43)
and cohort 2: September 2002 (n = 37),
total = 80
Findings
Ethnic group composition of the four
cohorts
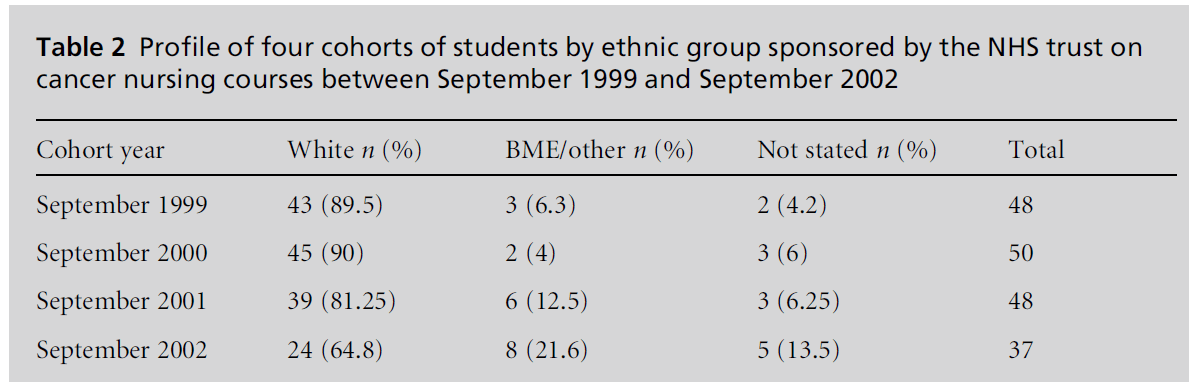
In order to detect trends in recruitment of BME
students, the ethnic group profile of four cohorts
between 1999 and 2002 was obtained from the human
resources department and is shown in Table 2. The
ethnic group of five (13.5%) students in the 2002
cohort was either not known or not stated. This compares with a range of 4.2% to 6.25% in the three
previous cohorts. Overall, there was an observable
increase in the percentage of BMEstudents enrolled
on courses over this four-year period, from 6.3% in
1999 to 21.6% in 2002.
Table 2: Profile of four cohorts of students by ethnic group sponsored by the NHS trust on
cancer nursing courses between September 1999 and September 2002.
Unfortunately it was not possible to undertake an
analysis by ethnic group of thosewho were accepted or
rejected for a sponsored place during this four-year
period. This was due to the completed application
forms not being retained, or the information not being
stored on a database.
Respondents’ profiles
There were three males and 27 females, with a mean
age of 29 years. Twenty-eight out of 30 gave details of
their country of birth. The majority (20) were born in
the UK and the remainder were born in the following
countries: Ireland (2), the Philippines (2), Finland (1),
Malaysia (1), Zimbabwe (1) and South Africa (1). The
ethnic groups as stated by the respondents showed
that in cohort 1, 10 (68.8 %)were white (including one
Manx), and six (31.2%) were BMEnurs es. In cohort 2,
12 (85.7%) were white and two (16.6%) were BME
nurses.
Out of the 30 respondents, the large majority (70%)
were registered in the UK (18 in England, three in
Scotland), with two in Ireland, two in the Philippines
and one each in Singapore, Zimbabwe, South Africa
and Australia. One respondent did not state the
country of registration.
With respect to the above, 10 respondents had
completed the three-year pre-registration programme
leading to the registered general nurse (RGN) qualification.
Another 11 had completed the diploma in
higher education (adult nursing), seven had completed
a degree in nursing and two had undertaken a
postgraduate diploma in nursing.
Across the two cohorts there were differences in the
length of time respondents had been registered. In
cohort 1, the length of time the respondents had been
registered ranged from one to 10 years, with a mean of
4.7 years. In the second cohort, the minimum was
one year and the maximum 29 years, with a mean of
7.2 years. Fourteen respondents indicated that they
would continue to degree-level study. Nine were not
sure, five stated that they already held a first degree and
two stated that they were planning to leave the course.
Seventeen out of 30 respondents (57%) had had
experience of a cancer care placement during their
pre-registration nursing course, seven had not and six
did not respond. All respondents had professional
experience in cancer care, 17 having worked in this
specialty for up to two years.
Sources of information
Fourteen respondents (46.6%) learnt about the sponsored
places programme from a nursing journal, and
12 (40%) from working at the trust. Other sources of
information included an overseas recruitment agency
(2) and by ‘word of mouth’ (1).
Motivation to do cancer care nursing
and perceptions of career prospects
All 30 responded to this question. Career opportunities
within the context of professional development
appeared to be a prime motivator. Cancer nursing
was perceived as being both challenging and rewarding
due to the complexity of the condition and the
variation in patient outcomes. Three respondents were
not clear about the reasons for coming into cancer
nursing, indicated by ‘drifted into’ and ‘wanting a
change’. Only one person mentioned the influence
of a placement during the initial pre-registration
training programme.
Respondents acknowledged that the specialty provided
‘a lot of job opportunities, promotion prospects
and professional development’. However, progression
to the higher F grade and specialist clinical practice
grade was seen as limited and competitive. The NHS
Cancer Plan was perceived as promising nurses a varied
career pathway (Department of Health, 2000b). The
positive aspects of oncology nursing were identified
(the cohort and respondent number are given in
brackets):
‘Oncology is actually a popular and ‘‘trendy’’ area of
nursing at present.’ (C1, 12)
‘... once [nurses] have worked in oncology many really
enjoy it and therefore stay.’ (C1, 14)
Barriers to recruitment and retention
in cancer nursing
Fourteen of the respondents thought that there were
barriers, 11 were not sure and four stated that there
were no barriers.
‘... no more than in nursing generally.’ (C1,13)
‘... generally I think there are major recruitment and
retention problems in nursing.’ (C1,12)
Some felt undervalued and that their concerns are
often not heard. The nature of the work in oncology
was perceived as being stressful and depressing.
‘Nurses often have to face [the] reality of their own
fragility with regards to death and dying.’ (C2, 3)
The emotional and psychological aspects of working
in cancer care were also identified.
‘Maybe some perceive it as an emotionally draining job
that only some can manage appropriately.’ (C2, 11)
‘It can be very stressful ... I have met nurses in the pastwho
have ‘‘burned out’’ whilst working in oncology.’ (C2, 2)
A further barrier cited by one respondent was:
‘... lack of exposure to specific oncology placements as a
student nurse.’ (C2, 13)
Finally staffing levels and poor pay were also identified:
‘Not enough staff to care for these patients fully and
holistically as it is very time-consuming.’ (C2, 5)
‘Poor pay (all nursing but also relevant to oncology).’ (C2, 7)
‘Lack of decent money affects retention.’ (C2, 8)
Barriers to recruitment of BME nurses
Only two (6.6%) students (no. 8 and no. 3 in cohort 2)
thought that there were any particular barriers to the
recruitment of BMEnurse s into cancer nursing.
Reasons included:
‘... certain cultural barriers may influence this.’ (C2, 8)
‘Some cultures don’t mention death or shun away from it
as it is frightening.’ (C2, 3)
One respondent, although not sure of any barriers,
offered the following insight:
‘There are no barriers at all. It’s only that a lot of them do
not like looking after ‘‘terminally ill patients’’ since cancer
is viewed as a chronic terminally ill disease.’ (C1, 9)
Fourteen (46.6%) thought there were none, 13
(43.3%) were not sure and two did not respond.
Examples of comments included
‘... did not know enough to comment.’ (C1, 4)
and
‘... nothing that I am aware of.’ (C1, 1)
However, they still expressed their views about the
following possible barriers:
‘The only possible barrier I can think of is that sometimes
language can be an obstacle.’ (C1, 5)
‘... they need to be able to speak, read and write the
language of the country they work in well.’ (C1, 6)
‘None that I am aware of, although a recent talk from a
representative of Cancer Black Care informed us that
cancer diagnosis has stigma attached in certain ethnic
groups as something that occurs as punishment for
behaviour.’ (C1, 13)
‘I am not sure, but working at the [trust] presently,
certainly does not show an equal proportion of nonwhite
ethnic minority nurses.’ (C1, 15)
‘I don’t think there is a problem because there are quite a
few ethnic minority nurses doing this course this year but
if you consider the ratio of ethnic minority nurses to
the total student population you may consider that they
comprise a very small fraction.’ (C1, 16)
Justifications for stating that there were no specific
problems in the recruitment of BMEnurs es included:
‘There is a good mix of different cultures in the ward.’ (C2, 9)
‘I have worked with many nurses from varied countries/
cultures. Many have held high nursing grades.’ (C2, 8)
Discussion
There appears to be a dearth of literature concerning
the representation of BMEnurse s within UK cancer
care services, in contrast to the debate about their
recruitment and career progression within the NHS in
general.
This study reinforces the utility of ethnic monitoring
as a tool to track the profile of nurses enrolling on
cancer care courses. The value of ethnic monitoring
for organisations is clearly set out in the updated guide
produced jointly by the Department of Health, the
NHS Health and Social Care Information Centre and
NHS Employers (2005). It allows organisations to
monitor fairness in recruitment and selection and
learning and development opportunities, and to identify
under-represented groups so that recruitment
drives can be targeted to increase the organisation’s
attractiveness to them.
This particular cancer care NHS trust had been
concerned about the low numbers of applications
received from BMEnurse s and was actively attempting
to recruit more onto their educational programmes.
This resulted in a significant increase in
their representation from 6.3% in September 1999 to
21.6% in September 2002 (cohort 2 in this study). In
cohort 1 (September 2001) the proportion of BME
students was 12.5% compared to 4% in the previous
cohort. This may be one of the reasons why most of
the students in this study did not perceive any major
barriers to the recruitment of BMEnurs es into cancer
nursing. A few did, however, highlight the low proportion
of BMEnurses in the trust, particularly in the
higher grades.
Students chose a career in cancer nursing because
of career development, personal interest and professional
satisfaction. Experience of a specialty during
training often leads students to consider working in
that specialty. Fifty-seven percent of the respondents
in this study had such an experience. This supports the
findings of Marsland and Hickey (2003) who reported
that 82% of nurses qualifying considered working in oncology because of their experiences of the specialty.
Barriers to recruiting nurses into cancer care were
viewed as similar to those of the NHS in general. They
included poor pay, staff shortages and not being
listened to and valued. Specific examples for cancer
nursing included emotional stress, that is to say ‘burn
out’, and the image of cancer as a depressing, frightening,
and terminal illness.
Only two out of 30 students perceived that there
might be particular barriers to the recruitment of
BMEnurs es into cancer care. Possible factors included
language problems, the stigma of cancer, and nursing
terminally ill patients. Two respondents noted the
possible impact of racism, either at a personal or
institutional level.
Reasons for perceiving no barriers to the recruitment
of BMEnurse s included: the existence of equal
opportunity employment policies, their own experience
of working with nurses from different cultures
(some at senior levels), and ‘the influx of Filipino
nurses’.
Conclusion
The low response rate in this study limits the ability to
draw any general conclusions from the findings.
Nevertheless, the majority of students did not view
recruitment of BMEnurse s into cancer services as an
issue. This was in stark contrast to the view of the
director of nursing who had been concerned for some
time at the low numbers of BMEapplicants to the
courses.
The degree of dissonance is of interest, as is the
dearth of papers on this topic within the nursing
literature. It may indicate a possible lack of awareness
among the cancer nursing profession about whether
BMEnurses are under-represented within this
specialty. This is in contrast to the prominence this
topic has acquired amongst other sections of nursing.
The issue of BMErepr esentation requires addressing
by those involved in cancer nursing workforce planning
and recruitment strategies.
Acknowledgements
The authors would like to thank Professor Dickon
Weir-Hughes, Chief Nurse/Deputy Chief Executive,
Royal Marsden NHS Foundation Trust.
References
- Airey C, Becher H, ErensB and Fuller E (2002) National Survey of NHS Patients.Cancer.NationalOverview 1999/ 2000.NHS Cancer Plan: a baseline survey. London: Department of Health.
- Aspinall PJ, WardAandAnionwuEN(2002) Equity of Access to NHS Cancer Services for Members of MinorityEthnicGroups: report of findings of surveys of hospital and medical and nursing staff at the Royal Marsden Hospital.A report to the Board of The Diana, Princess of Wales MemorialFund Project at the Royal Marsden NHS Trust. London: The Royal Marsden NHS Trust.
- Audit Commission (2001) HiddenTalents.Education, training and development for healthcare staff in NHS trusts. Northampton: Belmont Press.
- Baxter C (1988) The Black Nurse: an endangeredspecies. Cambridge: National Extension College for Training in Health and Race.
- Beishon S, Virdee S and Hagell A (1995) Nursing in a Multiethnic NHS. London: Policy Studies Institute.
- Booth K, KirshbaumMandLuker K (2001) An Evaluation of the Macmillan Lead Cancer Nurse Initiative.Final report. Manchester: Macmillan Cancer Relief/The University of Manchester.
- Commission for Racial Equality (1987) EthnicOrigins of Nurses Applying For and In Training – a survey. London: Commission for Racial Equality.
- Commission for Racial Equality (2002) Ethnic Monitoring: a guide for public authorities. London: Commission for Racial Equality.
- de Vaus D (2001) Social Research Methods. ThousandOaks, CA: Sage Publications.
- Department of Health (1999) Making a Difference.Strengthening the nursing, midwifery and health visiting contribution to health and healthcare. London: Department of Health.
- Department of Health (2000a) The NHS Plan.A plan for investment, a plan for change. Cm 4818 London: Department of Health.
- Department of Health (2000b) The NHS Cancer Plan.A plan for investment, a plan for reform. London: Department of Health.
- Department of Health (2004) Race Equality Action Plan. Leadership and race equality in the NHS. London: Department of Health.
- Department of Health/National Health Service Executive (2000) The Nursing Contribution to Cancer Care.A strategic programme of action in support of the national cancer programme. London: Department of Health.
- Department of Health/NHS Health and Social Care Information Centre/NHS Employers (2005) A Practical Guide to Ethnic Monitoring in the NHS and Social Care. London: Department of Health. www.cre.gov.uk/publs/cat_duty. html (accessed 18 April 2006).
- English National Board for Nursing, Midwifery and Health Visiting (ENB) (1998) Quality Assurance Manual.Priority area 1998–2000: equal opportunities. London: English National Board for Nursing, Midwifery and Health Visiting, p. 11.
- Gerrish K, Husband C and Mackenzie J (1996) Nursing for a Multi-ethnic Society. Buckingham: Open University Press.
- Iganski P, Spong A, Mason D, Humphreys A and WatkinsM (1998) RecruitingMinorityEthnic Groups into Nursing, Midwifery and Health Visiting. Research Report SeriesNumber 7. London: English National Board for Nursing, Midwifery and Health Visiting.
- King’sFundEqual Opportunities Task Force (KFEOTF) (1987) A Model Policy for Equal Opportunities in the NHS.OccasionalPaper No. 1. London: King Edward’sHospitalFund for London.
- King’sFundEqual Opportunities Task Force (KFEOTF) (1990) Racial Equality: the nursing profession. Equal Opportunities Task Force OccasionalPaper No. 6, London: King Edward’sHospitalFund for London.
- Klem R and Notter J (2001) Recruitment and Retention in Nursing and Professions Allied to Medicine of Individuals from Black and MinorityEthnicCommunities. Birmingham: University of Central England in Birmingham.
- Mahoney C (2001) White studentstwice as likely to get nursing places. Nursing Times 97:5.
- Marsland L and Hickey G (2003) Planning a pathway in nursing: do course experiences influence job plans? Nurse Education Today 23:226–35.
- NHS Executive (1997) Education and Training Guidance. London: Department of Health, EL(97)58, dated 3 October 1997.
- Olsen SJ and Frank-Strombourg M (1994) Cancer prevention and screening activities reported by African-American nurses. Oncology Nursing Forum 21:487–94.
- Punch KF (1998) Introduction to Social Research.Quantitative and qualitative approaches. London: Sage Publications.
- Richardson A, Miller M and Potter H (2001) Developing, delivering and evaluating cancer nursing services: building the evidence base. NT Research 6:726–35.
- Richardson A, Miller M and Potter H (2002) The organisation of cancer nursing services in the UK: areview of current practices. NT Research 7:288–96.
- Royal College of Nursing (2003) A Framework for Adult Cancer Nursing. London: Royal College of Nursing.
- ScanLink (1996) Guidelines for Commissioners and Providers of Cancer Care.Towardsbetter services for black and minorityethnic people with cancer. London: CancerLink.
- Thomas V, Richardson A and Saleem T (2000) The efficacy of bilingual health advocacy in ethnicminority patients with cancer. Nursing Standard 14:32–3.