Original Article - (2018) Volume 19, Issue 6
1Division of Hepatobiliary, Pancreas, and Abdominal Organ Transplantation at Keck Hospital of USC, USA
2Department of Surgery, Westchester Medical Center, Valhalla, NY, USA
3Department of Surgery, Southern Arizona Veterans Affairs Health Care System, Tucson, AZ, USA
4Department of Surgery, University of Arizona College of Medicine, Tucson, Arizona, USA
Received October 05th, 2018 - Accepted November 06th, 2018
Objective Several large volume centers have published positive outcomes with laparoscopic and robotic pancreaticoduodenectomy. The purpose of this study was to compare postoperative outcomes between open, laparoscopic and robotic pancreaticoduodenectomies using ACS National Quality Improvement Program. Methods We performed a review of 2014-2015 NSQIP targeted data for patients undergoing pancreatoduodenectomies for pancreatic cancer. Patient who underwent conversion from robotic or laparoscopic approach to open were excluded. Outcome measures were 30-day postoperative complications, and mortality. Results 11,218 patients who underwent pancreaticoduodenectomies were evaluated. Majority were performed in open fashion (n=8654) were open, followed by laparoscopic (n=1508), and robotic approach (n=596). Compared to open approach, laparoscopic PD had lower rates of SSI, and pneumonia rates; however longer operative time (354 vs. 482 min; p < 0.001). We found higher rates of 30-day mortality in patients undergoing robotic or laparoscopic pancreaticoduodenectomy when compared to the open group. Conclusion Smaller incisions did not predict reduced mortality or morbidity benefit in patients undergoing pancreaticoduodenectomy.
Adenocarcinoma; Pancreaticoduodenectomy; Pancreatic Neoplasms; Robotics
Pancreatic cancer is a devastating disease [1]. The annual incidence of pancreatic cancer in the US is 43,000 which will increase to 88,000 by 2030 [2]. The annual death toll due to pancreatic cancer is expected to rise from 36,888 to 63,000 by 2030 and it will be among the “Big Three” deadly cancers [3]. 15-20% of patients with pancreatic ductal adenocarcinoma present with a potentially resectable cancer. Surgical resection with a radical intent is the only curative treatment strategy available for these patients. Tumor size, vascular involvement, age and comorbidities are considered for the preoperative staging and decision to perform the surgical intervention [1]. Total pancreatectomy, distal pancreatectomy or Whipple procedure /pancreatoduodonectomy (PD) are the modalities used for surgical management of pancreatic cancer. Since Whipple published his landmark paper in Annals of Surgery, Whipple procedure is being increasingly used for the management of pancreatic cancer [4]. With the advent of minimally invasive surgery, advancement in anesthesia techniques, and availability of excellent postoperative care unit, this complex and previously high risk procedure has become the standard of care for patients with pancreatic ductal adenocarcinoma [5].
Previously pancreatic surgery belonged exclusively to the field of traditional open surgery. Gagner and Pomp reported the first laparoscopic PD; but there were concerns regarding the use of laparoscopic PD due to its complexity, unaltered morbidity, and technical difficulties [6, 7]. Application of robotic technology for PD has overcome some of these difficulties, and has emerged as an alternative to open surgery [8]. Minimally invasive surgery is considered a superior alternative to traditional open surgical method due to advantage of shorter incision, reduced postoperative pain, shorter hospital length of stay and earlier return to daily activities of living. There are multiple single center studies which compared laparoscopic vs. robotic PD, however outcomes in patients undergoing laparoscopic and robotic PD remain unknown on a national level. The aim of our study was to evaluate the impact of type of surgical approach (Open, Laparoscopic, and Robotic) on clinical outcomes after PD on a multiinstitutional national level. We hypothesized that Robotic/ Laparoscopic approaches were not associated with better outcomes than open technique for PD.
We performed a 2-year (2014-2015) analysis of the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) pancreatic demonstration project databank. The NSQIP is initiated by the ACS and is a quality improvement database. This database collects preoperative and 30-day postoperative data for various surgical procedures. The designated pancreatic project databank built within the NSQIP began abstracting data in 2011 from 43 hospitals [9]. In addition to the regular NSQIP variables, the pancreatic demonstration project databank contains certain pancreatic surgery specific variables. These includes preoperative variables (biliary stent, presence of obstructive jaundice), intraoperative variables (pancreatic duct diameters, pancreas texture, vascular reconstruction, type of pancreatic reconstruction, and drain placement), and postoperative variables (presence of drain, drain amylase levels, day of drain removal, presence of pancreatic fistula, use of percutaneous drainage, pathology results and delayed gastric empting) [10]. As the NSQIP only contains de-identified data, Institutional Review Board (IRB) approval was not required for this study.
Study population; Inclusion & Exclusion Criteria
We included all adult (age ≥18 years) patients who underwent pancreaticoduodenectomy for the indication of pancreatic cancer. We excluded all patients who underwent emergent procedures, patients with peri-ampullary cancers, cholangiocarcinoma or pancreatic cancers with vascular involvement or vascular reconstruction. We also removed patients who underwent neo adjuvant chemo radiation therapy or had laparoscopic or robotic surgery with open assist or hybrid approach. Patients who were converted from a laparoscopic or robotic procedure to an open operation were excluded from the analysis.
Data Points
The following data points were analyzed for each patient: demographics (age, gender, and race); mechanism of injury; preoperative laboratory parameters (serum albumin, hematocrit, International Normalized Ratio); comorbidities (coronary artery disease, chronic liver disease, diabetes mellitus, hypertension, and congestive heart failure); American Society of Anesthesiologists Classification score; hospital and intensive care unit length of stay; discharge disposition; and mortality.
Patients’ Stratification
We stratified patients into three groups based on operative approach; patients who underwent open pancreaticoduodenectomy, laparoscopic pancreaticoduodenectomy, and robotic pancreaticoduodenectomy.
Outcomes
Our primary outcome measures were 30-day complications. 30-day complications included pancreatic fistula, pancreatic bleed, superficial surgical site infection (SSI), deep SSI, organ specific SSI, wound disruption, pneumonia, unplanned intubation, time spent on ventilator ≥ 48 hours, deep venous thrombosis (DVT), pulmonary embolism (PE), transfusion occurrence, and return to operating room. Pancreatic fistula is defined in the PDP as either a persistent drain output of amylase rich fluid in combination with a drain longer than 7 days, percutaneous drainage, or reoperation; or as a clinical diagnosis and drain longer than 7 days, spontaneous wound drainage, percutaneous drainage, or reoperation [11]. Secondary outcome measures were 30-day readmission and mortality.
Data Presentation & Statistical analysis
We performed multiple imputations using a missing value analysis technique to account for the missing values. To impute the datasets, the original dataset was analyzed for random missing data points using little’s missing completely at random (MCAR) test. We used the Markov Chain Monte Carlo method for multiple imputations. This method refers to a collection of methods for simulating random draws from non-standard distributions.
We have reported the data as a mean with standard deviation for continuous parametric data and as median with interquartile range for non-parametric data. We have reported proportions for categorical variables. We utilized the student’s t-test and the Mann-Whitney U test to explore the differences between parametric and nonparametric data in our two groups, respectively. Similarly, the chi-square test was utilized for evaluating differences in categorical variables. A p-value <0.05 is considered statistically significant in our study.
We performed multivariate regression analysis to control for confounders. To assess the association between each potential dependent variable and the binary outcomes, we first performed a univariate analysis. Variables with a p-value less than 0.2 on the univariate analysis were then used in a multivariate logistic regression model. On the multivariate logistic regression analysis, variables were considered significant at a p-value less than 0.05. We then performed the Hosmer-Lemeshow test to assess the fitness of our overall model. In our logistic regression model, the Hosmer–Lemeshow test exceeded 0.05 and the tolerance was greater than 0.1 for all independent variables with a variance inflation factor of less than 10.0.
All statistical analyses in our study were performed using the Statistical Package for Social Sciences (SPSS, Version 24; SPSS, Inc., Chicago, IL).
We analyzed a total of 28,420 patients undergoing pancreatic resection. Of these, 11,218 patients underwent PD for pancreatic cancer. 8654 (77.2%) patients underwent an open procedure, while 1885 (16.8%) had a laparoscopic resection and 679 (6 %) patients had robotic resection. Of the total 1885 laparoscopic PDs, 25% (n=377) were converted to open intraoperatively. Similarly, of the 679 robotic PDs, 15% (83) were converted to open.
Table 1 Summarizes the demographics of the study groups. Patients who underwent robotic PD were more likely to be the youngest (p=0.02). However, there were no differences in gender, race, BMI, comorbidities, jaundice, pre-op biliary stenting, albumin ≤3g/dl, total bilirubin ≥2 mg/dl, pancreatic duct diameter, and pancreatic gland texture. Moreover, patients who underwent robotic PD had the longest operative time compared to laparoscopic and open PD.
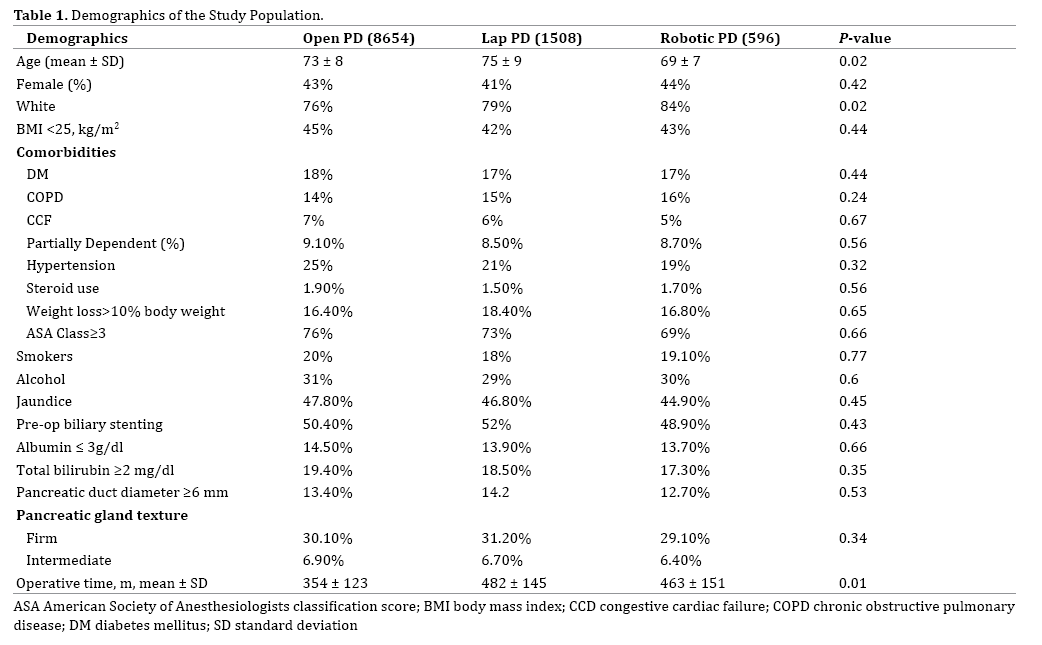
Table 2 summarizes the outcome measures of the study groups. Patients who underwent open PD had the highest rates of superficial SSI and pneumonia and lowest rates of return to OR and pancreatic bleed or angio-embolization. However, there were no differences in deep SSI, organ specific SSI, wound disruption, unplanned intubation, ventilator ≥ 48 hours, DVT, PE, transfusions, pancreatic fistula. Moreover, there were no differences in IR drain placement, hospital length of stay, and 30-day readmission. Patients who underwent robotic or laparoscopic PD had higher mortality rates compared to open PD group.
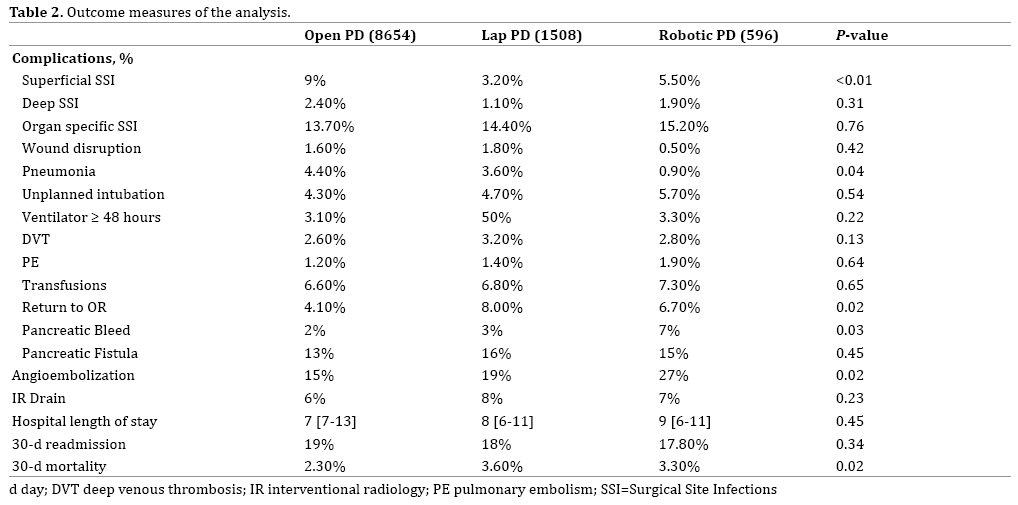
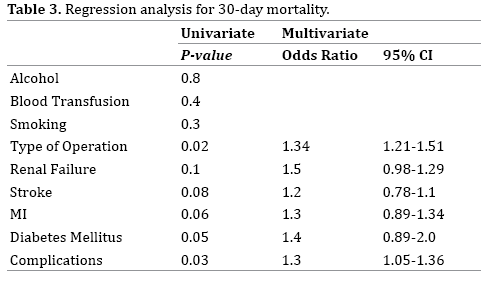
Table 3 summarizes the univariate and multivariate regression analysis for mortality. On univariate regression analysis, independent predictors of 30-day mortality were type of operation, renal failure, stroke, MI, diabetes mellitus, and complications. On multivariate regression analysis, after controlling for confounding factors, independent predictors of 30-day mortality were approach of PD (OR: 1.34), and complications (1.3).
The results of our study suggest that minimally invasive procedures for PD are not associated with improved morbidity or mortality. Patients who underwent laparoscopic/robotic surgery did not have lower hospital length of stay, decreased complications or mortality compared to patients who had open procedures. On the other hand, the operation time and the return to the OR were higher in patients who underwent laparoscopic/robotic surgery compared to open approach. In addition, we found a higher mortality rate in the minimally invasive group.
Several case reports and small case series have reported outcomes in patients undergoing laparoscopic PD. In 2011, a review of 27 published articles regarding laparoscopic PD concluded similar morbidity and mortality rates as compared to open PD [12, 13]. In addition, numerous other case series have concluded similar oncologic outcomes of laparoscopic PD compared to open PD in terms of consistent negative margin resection rates and lymph node retrieval [13, 14, 15]. However, like our study, all of these case series failed to demonstrate any superiority of laparoscopic PD compared to open PD in terms of morbidity, mortality. Most of these studies demonstrated longer operative times than open techniques.
In the past decade, the experience with robotic major pancreatic resections has evolved. However, literature suggests that they have been slow to expand. Giulianotti et al. in published the first large series of robotic pancreatic procedures in 2010 and demonstrating the safety and feasibility of the procedure [16]. Another case series of 132 robotic PD demonstrated the safety and feasibility of robotic surgery as compared to laparoscopic and open approach, with low incidence of conversion [17]. The rate of pancreatic fistulae was higher in this series compared to a similar high-volume institution for open PD. Here again, like our study, there was no difference in the hospital length of stay and robotic approach had longer operative times. Several other case matched studies and case series have showed similar results [18, 19, 20, 21, 22, 23]. None of these studies have demonstrated superiority of robotic approach compared to the open approach.
Our study does have certain limitations. Like any retrospective cohort comparing different interventions, a potential exists for selection bias. We attempted to mitigate this bias by performing multivariate regression analysis. The participating institutions of the Pancreatectomy Demonstration Project are more commonly high-volume centers that might be encountered in general practice. Thus, our study findings may be limited to these specialized centers with expertise in performing pancreatic surgery and may not be generalizable to the general population. Finally, the Pancreatectomy Demonstration Project only captures 30-day data from the time of surgery. The ACSNSQIP lacks long-term data on outcomes and survival. Thus, this study may not have captured all procedurerelated morbidity because outcomes in ACS-NSQIP are assessed at 30 days after surgery. Nonetheless, despite these limitations, our study provides data on outcomes in patients undergoing robotic and laparoscopic PD compared to open approach from national data.
Smaller incisions did not predict a small hospital length of stay; or a reduced mortality or morbidity benefit in patients undergoing PD.
The authors have no conflicts of interests to declare.