Keywords
Health expenditure; Primary care; Telehealth; Personalized healthcare; Big data
Introduction
The old saying that “an ounce of prevention is worth a pound of cure” is nowhere more applicable today than in primary care, the first point of contact in healthcare system. While global spending on health is expected to increase to $18.28 trillion in 2040 [1], the future of primary care is positioned to use advancements in telehealth technologies and big data analytics to deliver preventive medicine and personalized healthcare under value based care models [2]. Telehealth allows remote monitoring of patients and managing of their disease progression with continuous assessment; while big data analytics processes data collected from telehealth modality including both objective data (e.g. vital signs, ambient environment) and subjective data (e.g. symptoms, patient behavior) along with historical data to enable risk prediction and management. The significant increase in the global level of chronic diseases and the associated financial burden of hospital utilization; in addition to the progressive nature of these diseases, which often presents with symptoms varying within a day and over longer periods of time, have increased the demands for teleHealth mode to deliver timely care over distance. Multiple studies on telehealth for chronic disease management reported improved quality of life, reductions in hospital admission/readmissions and emergency department (ED) visits, reductions in length of hospital stay and even a decreased rate of mortality [3-5].
While aspects of telehealth and analytics have existed for decades, the developments in emerging digital health technologies provide innovative solutions to collect and process a massive amount of real time data. This has great potential to expand the capacity of primary healthcare to reduce risks, improve physicians-patients and patients-patients communication, and reveal unseen patterns or sensory features in a ubiquitous, personalized and continuous manner. For example, Intel has launched a wearable-to- analytics devices “A-wear” that directly ties wearable devices with big data analytics engine for instant processing and detecting of changes in data. Apple is working on a wearable medical-sensor-laden device “iWatch” to monitor blood through the skin; while Google announced the development of eye contact lenses that could analyze glucose levels through tears. Dell started a pilot program that focuses on analytics and tele-monitoring to predictively target patient with chronic diseases for more effective management. Thus, a patient with diabetes can have critical vital signs actively monitored, with dietary intake and activity tracked in order to receive reminders of prescribed schedule of treatment and encouragement to maintain a certain life style. In a real life applied scenario, El Camino Hospital in USA has made the news as it achieved a 39% reduction in falls in six months a tele-based analytics project to identify patients at risk and immediately prescribe the most appropriate means of intervention. Such solutions also can support the critical role of primary care to deliver responsive, holistic care that will reduce the likelihood of preventable risks.
Primary care is defined as “integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community” [6]. Accordingly, the primary care should be derived by key principals such as: (i) relationships to serve as the bedrock of value fostered by teams, improved clinical operations, and technology; (ii) patients and non-physicians engaged in most aspects of healthcare; and (iii) the whole-person care including health behaviors and social services [7]. In alignment with this vision, we propose the Smart Primary Care Environment (SPCE) as a health ecosystem of interacting objects, e.g. sensors, devices, embedded systems, health professionals, patients, that have the capability to seamlessly provide services and manipulate complex data in a self-organize manner. In smart environments [8], technological devices and intelligent computing systems are adopted to analyze and manage daily activities of people. Translating primary care services to smart environment targets solving issues related to again and dependency; e.g. monitoring chronic diseases and reducing medication administration error. It also contributes to improving patient engagement, and promoting cross-sector integration to realize the whole-person care. The quality, persistency and responsiveness of services in SPCE requires handling the vast amount of data generated from interacted objects by big data analytics methods to support evidence- based decision making and action plans. One unique feature of smart environment, is the ability of its objects to acquire and apply knowledge about the environment in order to optimize the service model and reduce expenses of the essential resources (e.g. prioritize cases that need extra medical attention); while maintaining high communication loads to improve the whole experience.
In this paper, we identify the major technologies to enable our Smart Primary Care Environment (SPCE) model. Our proposed conceptual model for SPCE aims at providing a meaningful blueprint to design and implement telehealth and analytics services in primary care settings. We also discuss the key influencing factors to achieve successful penetration and impact on primary care delivery. The remaining of this paper is organized as follows. Section 2 discusses the emerging technologies on telehealth and big data analytics. Section 3 presents the SPCE conceptual model while key success factors are discussed in Section 4. Section 5 concludes the paper with future outlooks.
Enabling Technologies: Opportunities and Challenges
Wearable systems/sensors
The wearable technology nowadays offers more sophisticated designs of miniaturized electronic devices or sensors that can be implanted within the body of a user to transduce various types of information related to the user or his/her ambient environment. Wearables can capture physical (e.g. heart rate, respiratory rate, blood pressure) and chemical (e.g. glucose, lactate, potassium) signals; and they are usually integrated with a ubiquitous system of smartphone and wireless connectivity (e.g., WiFi and Bluetooth technologies) to develop more dynamic and real-time motioning systems. A wearable monitoring system transmits the continuously acquired data to the cloud or local servers for data processing, and receives feedback and/or notifications for future action. On a recent stage, hearable technology has emerged to add the advantages of audio feedback and even treatment information to be sent to the device’s wearer [9]. For example, AccendoWave has partnered with Samsung to produce a hearable device for pain management [10]. The device measures discomfort in the user's electroencephalography (EEG) system then uses a Samsung tablet to generate audio content (e.g. music, short movies) based on the user’s discomfort level. The user’s pain level is continuously monitored through their brain waves to assess how the suggested content alleviates their pain.
While the wearable systems hold substantial promises to improve the quality of human life by expanding the ability to tailor care to the particular physiology of the individual patient, they still face significant challenges in terms of efficient connectivity and single reliability. The real-time scenario entails the access to live and high-speed streaming data via continuous noise-free signals. However, the length of data transmission is typically short resulting in a sparse data sampling with uncertainty in the measured variables which reduces quality and utility of the data. On the other hand, poor network connectivity and poor noise-filtration result in data loss and may generate false alarms. In addition, there is a governance challenge such as lack of standards and data protocols especially that captured data are downloaded only using proprietary software and data formats provided by the device manufacturers. The high cost of implementing wearable systems that enable data sensing in a large scale is also an open challenge. More of developments in wearable technologies for telehealth and associated challenges for clinical adoption are presented in [9,11,12].
IoT
The coupling IoT and wearable technology has the potential to improve the availability and accessibility of healthcare services to producing more personalized systems at -relatively-lower cost. The IoT concept reflects a worldwide network of intercommunicating set of anyone, any services, any networks, any physical objects, or “things” that are connected to the Internet, and available from anywhere, anyhow and anytime; with the ability to identify themselves to others. In healthcare industry, it is often referred to as “internet of healthcare things” (IoHT) or “internet of patients” (IoP) to emphasize its potential to ease cost- effective interactions through secure communication mechanisms across different parties in the healthcare system including individual patients, clinics, and healthcare organizations. IoT-based healthcare systems can be established using different technologies, topologies and architectures but with basic building elements that are: i) sensors to collect data, ii) micro-controllers to process, analyze and wirelessly communicate the data; iii) micro-processors to enable rich graphical user interfaces; and iv) healthcare-specific gateways through which data is further analyzed and forwarded to the cloud. A prototype of a cloud-based IoT system is presented in [13] to collect sensor biosignals data, motion data (through accelerometers) and contextual data (e.g. location, ambient temperature, activity status). Data is wirelessly sent to a mobile phone or directly to the cloud infrastructure utilizing the established techniques for IoT communication. Next, appropriate interfaces or gateways enable the data dissemination to external applications that provide the essential data real-time monitoring, management and analysis. Similarly, a telehealth model controlled by IoT , “Cogsense”, is proposed in [14]. The “Cogsense” system works with sensors module and cloudnetwork communication module to enable interconnection and collaboration of multiple devices and personals involved in the patient care. The system also incorporates analytics module to process information from cloud infrastructure with IoT algorithms and machine learning techniques.
Yet, the penetration of IoT-driven healthcare solutions into actual clinical practice is in its infancy with many challenges to address in areas such as heterogeneity and semantic interoperability of devices on IoT networks. The study in [15] provides a comprehensive survey for advances in IoT-based healthcare technologies including a review of the state-of-the-art IoTnetwork architectures, platforms, applications, and industrial trends.
Edge/fog computing
Edge computing or Fog computing is an emerging trend that brings cloud computing capabilities to the edge of the network and as a result, closer to the IoT devices and applications that increasingly generate massive amounts of data while they interact and consume cloud services. Thus, IoT services and data computations are performed only at the network edge, or where data is originated, resulting in higher efficiency processing than if it needed to be sent to the cloud. In other words, fog computing acts as a middle layer or a smart gateway of computing power between the sensing devices and the cloud in a sense that it allows wearables and IoT health devices to conduct critical processing based on their computing capacity. They become processing nodes that can handle smaller and time-sensitive computational decisions without having to send all their data up to the cloud. This new perspective aims at extending the cloud computing to address the need to adequate distribution of services in ambient environments in order to provide sensitivity to real-time monitoring and other applications that require minimum and predictable latency. It also displaces the focus from centralized processing in cloud computing to a middleware platform perceived by sensors as a service point that enables the distribution of information processing among several central processing units or sensors.
In addition to latency reduction, the advantages of fog computing to telehealth applications include enforcing of security measures and data privacy due to the hierarchal structure of the system and the concept of service localization [16]. For example, a service-oriented fog computing architecture proposed is in [17] to reduce storage requirements and, thus, increase the overall efficiency of telehealth communication and big data solutions. The proposed system is built using Intel®’s Edison embedded processor, referred to as fog computer, to perform local data analytics and only transmits necessary data to the cloud after preliminary processing and filtering. A fog computing assisted distributed analytics system, FAST, is also proposed in [18] as a real-time fall detection system to monitor fall for stroke patients. The system employs a set of fall detection algorithms, including algorithms based on acceleration measurements and time-series analysis methods. It also applies several filtering techniques to extract important features and facilitate fall detection process. The system divides the fall detection task between the edge/ fog devices and the cloud in order to achieve a high sensitivity and specificity while enhancing the efficiency and reliability of the system operations. More on fog computing principles, architectures, and applications for telehealth In a different view, is reviewed in [19].
Big data visual analytics
Big data analytics is evolved from business intelligence to enable healthcare organizations to analyse an immense volume, variety and velocity of health data for insights. HIMSS defines health analytics in general as the “systematic use of data and related clinical and business insights developed through applied analytical disciplines such as statistical, contextual, quantitative, predictive, and cognitive spectrums to drive fact-based decision making for planning, management, measurement and learning” [20]. In a different view, it refers to a complete series of “integrated capabilities” that provide progressively deeper insights into health-related information. It encompasses a four-stage model composed of descriptive analytics, predictive analytics, prescriptive analytics and discovery analytics that are ideal for analyzing the totality of data related to patient healthcare and well-being which makes up the “big data”. Predictive analytics in particular is believed to go beyond reducing cost, to be able to reduce preventable deaths [21]. For instance, predictive analytics could be used to identify high-risk patients for healthcare providers to intervene early and make proactive decisions to provide them treatment and avoid unnecessary readmissions or hospitalizations. It also can be used to develop a prediction model from past history of individuals so that a new individual can get a predictive alert to prevent a future risk. For doing so, predictive analytics involves using statistical techniques, machine learning methods and modeling to examine historical or summarized health data, detect patterns of relationships in these data, and then extrapolate these relationships to predict potential outcomes. However, predictive analytics is different from traditional statistics and evidence-based medicine as predictions are made for individuals and not for groups; and they do not rely upon a normal curve. A general overview of big data analytics potentials in healthcare is provided in [22].
The modern generation of big data analytics in healthcare incorporates a range of advanced and innovative data presentation capabilities to enable visual analytics [23]. In such models, visualization allows interactive analytic process, where humans and computers effectively cooperate using their respective distinct capabilities for data processing and visual recognition. The “visual analytics" filed itself has formally begun in 2005 by the publication of Illuminating the Path: The R&D Agenda for visual analytics [24]. R&D agenda defines visual analytics as “the science of analytical reasoning facilitated by interactive visual interfaces”. As people are better to discover and understand their world through integrating direct observations with theoretical models, visual analytics reconciles conceptual models with direct observations of evidence to enable insights to explain those observations when they do not fully conform to existing theory [25]. In big data analytics, the visual representation of the large and complex healthcare data sets in conveys the intensive relationships among many elements in parallel, and provides analysts with directly observable memory. It enables them to dynamically operate between their cognitive models (i.e. experiences and knowledge) and the evolved patterns and insights from data exploration to identify new or verify existing knowledge [26].
However, the exponentially increasing volume of big data poses a challenge for the data current processing, analysis and management capabilities. Process challenge relates to data acquisitions and the ubiquitous capture of life-logging personal health data via wearable monitoring devices and mobile apps along with the signal processing approaches for conditioning highresolution data. It also includes data warehousing and cleaning for analytical operations. The analysis process itself is challenged by the ability to integrate data from heterogeneous sources; and the complexity and cost of data standardization and interoperability between different health information systems. Moreover, there is a need for scale-tolerant visual approaches that enable reasoning over large and diverse information spaces and introduce a holistic information representation synthesizing all forms of data into inter-related knowledge structures. Management challenges, on the other side, cover for example privacy, security, governance and ethical aspects. A recent study in [27] presents a holistic view of the different of big data analytics challenges and discusses the different types methods proposed to overcome these challenges.
Smart Primary Care Environment (SPCE) Model
The enabling technologies discussed above has to move primary care to smart environments where technological tools are adopted to analyze daily-life activities of patients in order to provide an ambient assisted living. The visionary model of Smart Primary Care Environment (SPCE) aims at helping patients to stay with the best quality of life as long as possible in their homes; while they are engaged in advancing their health through improved communication and enhanced self- management. Most importantly, SPCE integrates big data analytics module in a telehealth-based primary care system to analyze both real-time data and historical information of the individual patient to predict possible future outcomes and trigger timely intervention by the healthcare professionals. The embedded IoHT or IoP system can route the action plan necessary for a patient to a wider audience of multiple healthcare professionals without interruption on the speed or quality of the service. For example, captured data and action plan can be forwarded to a specific nurse or a primary care physician responsible for the patient or even to an external specialist/consultant for further discussion - if the medical system of the provider or the region allows for such automatic routing or collaboration. While healthcare professionals will be able to access all the details of patients anytime by accessing multiple IoT devices through the SPCE network; patients will be also able to connect directly with their healthcare providers and/or other patients. If we consider the fact that 40% of of the world population are active on Internet; and apply the six degrees rule of complex network, then every other patients/healthcare professionals can be simply connected to a SPCE through the the users’ contacts.
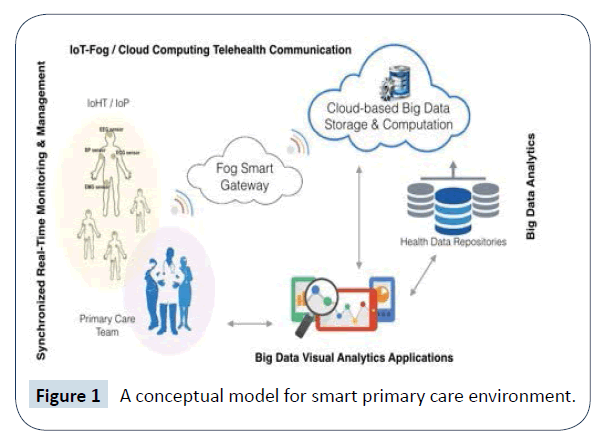
Figure 1 presents the conceptual model for SPCE that consists of four subsystems: (1) wearables/hearables in IoHT/IoP networks for data acquisition; (2) a fog computer acts as a smart gateway for onsite processing that varies from simple filtering to complex wavelet analysis; (3) big data visual analytics module; and (4) a cloud server for big data storage and back-end computation. The fog gateway connects the wearables and IoT sensors to primary care providers for diagnosis, evaluation, and treatment. It also accumulates and processes the real-time data acquired from continuous monitoring of patients in order to perform “on-demand real- time analytics” at that level using specific algorithms for extracting clinically relevant features and mining patterns in time-series data. The features and local data processing techniques (i.e. storage, integration, filtering, mining and management) pertaining fog computers as smart gateways in telehealth systems are described in more details in [28,29]. The acquired data and/or extracted features and index of patterns from time- series analytics are sent to the the cloud; where they can be integrated with data from other data repositories (e.g. EHR, clinical registry, medical imaging and laboratory results, social media posts) and processed by the big data visual analytics module with more complex computing methods to meet requirements of different healthcare applications (e.g. diabetes management, medication management, allergic symptoms, melanoma detection, fall detector, asthma attack prediction, heart failure prediction..etc). The analytics result is displayed to the end users via the visualization engine providing predictions and action plans recommendations based on personal health-risks assessment. The visual module may include mobile, desktop, and web based interfaces; while the visualization strategies include a different combinations of representations mechanisms, such as tables, bar charts, graphs, maps, and 3D modeling and others which enable the multidimensional exploration of health indicators.
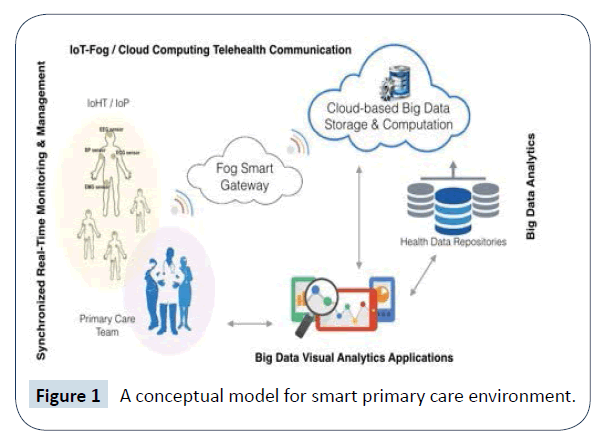
Figure 1: A conceptual model for smart primary care environment.
Key Success Factors
Apart from technical challenges, there are key factor influencing the realization of successful SPCE. The most substantial factor is the development of new education paradigms for patients and healthcare professionals. For patients, it is important to consider their technology knowledge gaps that may create confusion, fear and low confidence in the quality of the service. In order to be effective, SPCE requires patients who are self- determined and motivated to use telehealth technologies. In addition, patients who are ready to utilize the great amount of information created within the SPCE to build knowledge and health literacy about disease self-management. Patients in SPCE are also expected to effectively involve in patient-to- patient interventions and communities enforcing the shift for more preventive care. On the other hand, healthcare professionals should also be ready to adopt the communication and analytics technologies; and to expand technological capabilities to form community of knowledge and practice. Such communities are set to establish a strong evidence base to inform practice while applying the most recent clinical and analytical advances towards scalable and sustainable smart primary care environments.
However, in order to realize optimal preventive primary healthcare system, effective use of data is essential. Bigger and more data doesn’t equate to more or better insights! Predictive data molding should be personalized to each individual focusing on a specific clinical setting and particular individual parameters to avoid generic predictors. Moreover, the lack of diverse knowledge domains among healthcare professionals presents another challenge for generating accurate predictive insights. While the data is driven from different domains (i.e. clinical, administrative, social, research), it is critical to understand facts from other domains in order to predict something in one particular domain. For example, a prediction on cardiovascular damage may require an understanding of the socioeconomic environment that an individual is from or his behavior styles. Building capabilities to combine knowledge from different domains is not only a technical-based challenge; but it also requires creating joint communities of knowledge, solving clinical adoption barriers, and infusing active patient’s engagement. A case study presented in [30] describes the implementation of a telehealth program that reduced 30-day hospital readmissions among heart failure. The study reported two key factors that have contributed to this achievement: (i) the significance of healthcare professionals trust and support to the program as well as their inter-profession collaboration; and (ii) patient engagement and motivation, enhanced by “user-friendly” tools, to achieve self-care.
Another factor is about matching patients with the appropriate technologies to gather the most amount of meaningful data. This may lead to improved insights about current conditions and better assessment of provided care management strategies. The SPCE model is proposed as a possible solution to the cost and shortage of healthcare delivery; and so it is critical to decide wisely how and when to use the technology according to patient’s age, clinical condition, education, physical capabilities, cognitive abilities, functional independence, and ability to use/access technology. For example, elderly patients with visual limitations and limited manual dexterity are best matched with computer based apps with large screens and static interaction. In contrast, younger patients prefer small devices that are able to follow their progress and provide immediate feedback. In fact, the telehealth is not appropriate for any patient! exactly as any other clinical procedure. In order to realize the cost-benefit ratio, it is important to firstly identify patients who will benefit the most from this delivery mode while still saving cost on the care provider end. On this thrust, one interesting recent study [31] investigated the strategies to invest on wearables and big data analytics strategies from an economic perspective revealing that with differentiated consumers/patients densities (i.e. preferences), organizations are more likely to engage in quality competition and achieve higher profits.
One more factor is about telehealth policies and the involved legal, ethical and licensing issues. There is an urgent need to clearly define telehealth care as a mode of healthcare delivery and to regulate its cross-sector and cross-border care (locally and internationally). Moreover, it is required to re-form the traditional licensing laws and policies to accommodate telehealth practice; while at the same time ensuring that care is provisioned by a licensed professional evident via-for instance-a key-policy certified profile that could be shared instantaneously with the patient during the tele-care session.
Concluding Remarks
Telehealth and big data analytics have great potentials to increase capacity of primary care to enact the objectives of health care delivery system reform. The real-time analysis of sensing and historical data expands the bandwidth of primary care team for offering life-saving alerts. We introduced the concept of Smart Primary Care Environment (SPCE) as an interactive space where technology, patients and personals involved in patient care are synchronously connected to enhance disease management and quality of life. The adoption of our model, however, is challenged by a number of technical and nontechnical issues. Yet, at the core of successful realization of SPCE, is the establishment of clear evidences on clinical and economic benefits, and effective strategies to manage changes in the design and practice of current primary care systems. Most importantly is to get healthcare professionals and patients onboard to solve adoption barriers and deliver best value. We hope that this paper provides insights to the future of primary care as a smart environment for delivering continuous and preventive whole-person care.
References
- Dieleman JL, Templin T, Sadat N, Reidy P, Chapin A, et al. (2016) National spending on health by source for 184 countries between 2013 and 2040. Lancet 387: 2521-2535.
- Dinesen B, Nonnecke B, Lindeman D, Toft E, Kidholm K, et al. (2016) Personalized telehealth in the future: a global research agenda. J Med Internet Res 18: e53.
- Paré G, Jaana M, Sicotte C (2007) Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc 14: 269-277.
- Polisena J, Coyle D, Coyle K, McGill S (2009) Home telehealth for chronic disease management: a systematic review and an analysis of economic evaluations. Int J Technol Assess Health Care 25: 339-349.
- Bashshur RL, Shannon GW, Smith BR, Alverson DC, Antoniotti N, et al. (2014) The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health 20: 769-800.
- Yordy KD, Vanselow NA (1994) Defining primary care: an interim report. National Academies Press.
- Ellner AL, Phillips RS (2017) The coming primary care revolution. J Gen intern Med 32: 380-386.
- Vermesan O, Friess P (2013) Internet of things: converging technologies for smart environments and integrated ecosystems. River Publishers.
- Pistorius C (2017) Developments in emerging digital health technologies. DeltaHedron Innovation Insight.
- Marbury D (2017) Top 10 healthcare wearables to watch. Managed Healthcare Executive.
- Zhu X, Cahan A (2016) Wearable Technologies and telehealth in care management for chronic illness. In healthcare information management systems. Springer International Publishing, pp: 375-398.
- Baig MM, GholamHosseini H, Moqeem AA, Mirza F, Lindén M (2017) A systematic review of wearable patient monitoring systems–current challenges and opportunities for clinical adoption. J Med Syst 41: 115.
- Doukas C, Maglogiannis I (2012) Bringing IoT and cloud computing towards pervasive healthcare. In innovative mobile and internet services in ubiquitous computing (IMIS), 6th International Conference on IEEE, pp: 922-926.
- Al-Majeed SS, Al-Mejibli IS, Karam J (2015) Home telehealth by internet of things (IoT). In Electrical and computer engineering (CCECE), IEEE 28th Canadian conference on IEEE, pp: 609-613.
- Islam SR, Kwak D, Kabir MH, Hossain M, Kwak, KS (2015) The internet of things for health care: a comprehensive survey. IEEE 3: 678-708.
- Shi Y, Ding G, Wang H, Roman HE, Lu S (2015) The fog computing service for healthcare. In Future Information and Communication Technologies for Ubiquitous HealthCare (Ubi- HealthTech), 2nd International Symposium on IEEE, pp: 1-5.
- Dubey H, Yang J, Constant N, Amiri AM, Yang Q, et al. (2015) Fog data: enhancing telehealth big data through fog computing. In proceedings of the ASE big data and social informatics, ACM, p: 14.
- Cao Y, Chen S, Hou P, Brown D (2015) FAST: A fog computing assisted distributed analytics system to monitor fall for stroke mitigation. In Networking, Architecture and Storage (NAS), IEEE International Conference on IEEE, pp: 2-11.
- Dastjerdi AV, Gupta H, Calheiros RN, Ghosh SK, Buyya R (2016) Fog computing: principles, architectures, and applications. Cornell University Library.
- Clinical and business intelligence: an analytics executive review (2013) HIMSS clinical and business intelligence.
- Raghupathi W, Raghupathi V (2014) Big data analytics in healthcare: promise and potential. Health Info Sci Syst 2: 3.
- Wang Y, Kung L, Byrd TA (2016) Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technol Forecast Social Change.
- Youbing Z, Farzad P, Hui W, Enjie L, Zhikun D et al. (2016) Visual analytics for health monitoring and risk management in CARRE. In International Conference on Technologies for E-Learning and Digital Entertainment, pp: 380-391.
- Thomas JJ, Cook KA (2006) A visual analytics agenda. J IEEE Comp Graph Appl 26: 10-13.
- Wong PC, Rose SJ, Chin G, Frincke DA, May R, et al. (2006) Walking the path: a new journey to explore and discover through visual analytics. Info Visual 5: 237-249.
- Simpao AF, Ahumada LM, Rehman MA (2015) Big data and visual analytics in anaesthesia and health care. Br J Anaesth 115: 350-356.
- Sivarajah U, Kamal MM, Irani Z, Weerakkody V (2017) Critical analysis of big data challenges and analytical methods. J Bus Res 70: 263-286.
- Rahmani AM, Thanigaivelan NK, Gia TN, Granados J, Negash B, et al. (2015) Smart e-health gateway: Bringing intelligence to internet-of-things based ubiquitous healthcare systems. In Consumer Communications and Networking Conference (CCNC), 12th Annual IEEE, pp: 826-834.
- Stantchev V, Barnawi A, Ghulam S, Schubert J, Tamm G (2015) Smart items, fog and cloud computing as enablers of servitization in healthcare. Sensors Transducers 185: 121.
- O'Connor M, Asdornwised U, Dempsey ML, Huffenberger A, Jost S, et al. (2016) Using telehealth to reduce all-cause 30-day hospital readmissions among heart failure patients receiving skilled home health services. Appl Clin Inform 7: 238-247.
- Wu J, Li H, Cheng S, Lin Z (2016) The promising future of healthcare services: When big data analytics meets wearable technology. Info Manag 53: 1020-1033.