- (2010) Volume 11, Issue 1
Naira Sultan Khuroo1, Mohammad Sultan Khuroo1, Mehnaaz Sultan Khuroo2
1Digestive Diseases Centre, Dr. Khuroo’s Medical Clinic; 2Department of Pathology, Sher-e-Kashmir Institute of Medical Sciences. Srinagar, Kashmir, India
Received July 10th, 2009 - Accepted October 27th, 2009
Context Tropical calcific pancreatitis is unique to developing countries with of unknown origin. Objective We evaluated the pattern of pancreaticobiliary ductal union in patients with tropical calcific pancreatitis. Patients Twenty-one patients with tropical calcific pancreatitis were compared to 174 control subjects with no pancreaticobiliary disease and 35 patients with alcohol-induced chronic pancreatitis. Main outcome measure Two experienced people, blinded to the results, evaluated the pattern of pancreaticobiliary ductal union. Pancreaticobiliary ductal unions were classified as: separate ducts (no union), a short common-channel (length less than 6 mm), a long common-channel (length ranging 6-15 mm) and anomalous pancreaticobiliary ductal union (length greater than 15 mm). Anomalous union was defined as P-B type when the pancreatic duct appeared to join the bile duct and B-P type when the bile duct appeared to join the pancreatic duct. Any disparities between the two investigators were sorted out by mutual discussion. Results Pancreaticobiliary ductal union in tropical calcific pancreatitis patients as compared to those in the control group was as follows: separate ducts, 23.8% vs. 49.4% (P=0.036); a short common-channel, 4.8% vs. 28.7% (P=0.017); a long common channel, 33.3% vs. 18.4% (P=0.144) and anomalous pancreaticobiliary ductal union, 38.1% vs. 3.4% (P<0.001). The B-P pattern of anomalous pancreaticobiliary ductal union was more frequent in tropical calcific pancreatitis than in the control group but there was no statistical significance (P=0.103). The angle of the pancreaticobiliary ductal union in the tropical calcific pancreatitis group was 88.1±36.2° as compared to 20.0±11.5° in control group (P<0.001). Alcohol-induced chronic pancreatitis (No. 35) predominantly had either separate ducts (65.7%) or a short common channel (25.7%). Conclusion We concluded that patients with tropical calcific pancreatitis in Kashmir had anomalous pancreaticobiliary ductal union, predominantly of B-P type with a wide angle of ductal union more frequently. This may be related to the etiology of tropical calcific pancreatitis in such regions.
Bile Ducts; Calculi; Cholangiopancreatography, Endoscopic Retrograde; Pancreatitis; Pancreatitis, Chronic
AICP: alcohol-induced chronic pancreatitis; B-P: biliary pancreatic union; ERCP: endoscopic retrograde cholangiopancreatography; P-B: pancreatic biliary union; PBDU: pancreaticobiliary ductal union; TCP: tropical calcific pancreatitis
Tropical calcific pancreatitis is a disease with unique clinical and radiological features and is prevalent in many tropical countries including south India, Sri Lanka, and many African and Asian countries [1, 2, 3, 4, 5, 6, 7, 8]. The disease is reported to affect younger age groups; it is characterized by rapid progression associated with severe pancreatic damage and multiple large ductal calculi, and the absence of a history of alcoholism or biliary tract disease. Abdominal pain and diabetes are dominant clinical manifestations. Steatorrhea and malnutrition may be associated features [9, 10]. The pancreas shows atrophy, markedly dilated pancreatic ducts and large intraductal calculi. A pancreatic neoplasm is a common occurrence in these patients [11]. Over the years, there has been a trend to occurrence in older age groups and it has been reported in countries outside the tropics [12, 13]. The etiology of tropical calcific pancreatitis in such countries remains obscure.
Pancreaticobiliary ductal union is the confluence of the pancreatic duct and the bile duct; this union shows many variations [14, 15]. Patterns of pancreaticobiliary ductal union have been associated with many pancreatic and biliary diseases [16, 17, 18, 19, 20]. The relationship of the patterns of pancreaticobiliary ductal union with tropical calcific pancreatitis has not been studied. We wish to report on the pattern of pancreaticobiliary ductal union in patients from Kashmir, India having tropical calcific pancreatitis.
This was a nested case control study which was designed to study the pattern of pancreaticobiliary ductal union in 21 patients from Kashmir, India having tropical calcific pancreatitis and compares them with 174 control group patients with no pancreaticobiliary disease and 35 patients with alcohol-induced chronic pancreatitis.
The study included all endoscopic retrograde cholangiopancreatographies (ERCPs) carried out by the senior investigator (Author 2) from November 1982 to March 1995 and from April 2005 to March 2008 in Kashmir India. All patients belonged to one ethnic group (residents of Kashmir Valley). All ERCP images were photographed and compiled into folders, each folder containing the images of one patient and carrying a specific patient identification number. The clinical details, laboratory data, histological findings, follow-up and diagnosis of patients in whom ERCPs were carried out were contained in each folder.
For this study, the ERCPs were examined by two investigators (Authors 1 and 2) independently who were blinded to the clinical data. The ERCPs were reviewed from June 2007 to August 2008. The purpose of the study was to define the patterns of pancreaticobiliary ductal union in each ERCP. The findings were recorded on a computer generated proforma. The method of defining the various features of pancreaticobiliary ductal union was first mutually agreed upon [15, 21] and was then practiced on 20 randomly selected patients, and the reporting was standardized. Discrepancies between the two investigators were mutually discussed and sorted out.
The reporting of the ERCPs was done in a stepwise fashion. The first step was to identify ERCPs in which both ducts were filled and pancreaticobiliary confluence was clearly identified in more than one image (inclusion criteria for study) (Figure 1). ERCPs in which only one duct (pancreatic or biliary) was filled or the confluence of the pancreatic and bile ducts was not clearly visualized were excluded from the study (Figure 1). Second, in those ERCPs included in the study, we then reported on whether the pancreatic and bile ducts opened into the duodenum separately or if the ducts were joined to each other and a common channel opened into the duodenum(Figure 2). Third, we measured the length of the common channel in the latter (Figure 3). To do so, we measured the actual length of the channel as it appeared on the images and corrected it with a magnification factor, as determined by the actual and imagined (as on images) width of the endoscope [15, 21]. If the corrected length of the united duct was less than 6 mm, it was reported as a short common channel. If the corrected length of the united duct was between 6 and 15 mm, it was reported as a long common channel. If the corrected length of the common channel was more than 15 mm, it was presumed that the ductal union had occurred outside the duodenal wall and such patients were reported as having anomalous pancreaticobiliary ductal union [20, 22]. For patients with anomalous pancreaticobiliary ductal union, we determined the pattern and angle of the ductal union. Anomalous pancreaticobiliary ductal union was reported as P-B type when the pancreatic duct appeared to join the bile duct and B-P type when the bile duct appeared to join the pancreatic duct. The angle of union was the actual angle at which the union occurred between two ducts [23].
Figure 1. Step 1 of the present study defined the inclusion and exclusion criteria. Three ERCP images are shown. ERCP 1 (included for further
evaluation) shows large hepatic cystic lesions communicating with the bile ducts. Both the pancreatic duct and the bile duct are clearly visualized and
the union of the two ducts before entering the papilla is clearly identified. ERCP 2 (excluded from study) shows the malignant stricture of the bile
duct. Only the bile duct is visualized. ERCP 3 (excluded from study) from a patient with alcohol-induced chronic pancreatitis. Only pancreatic duct is
visualized.
BD: bile duct; PD: pancreatic duct.
Figure 2. Step 2 of the present study classified the ERCPs into those with a separate opening and those with a common channel. On the left, ERCP image from a patient with alcohol-induced chronic pancreatitis. The bile duct (BD) and the pancreatic duct (PD) can be clearly seen and join the duodenum (arrows) without joining each other. On the right, the image belongs to a patient with choledocholithiasis. The pancreatic duct (PD) and the bile duct (BD) join each other to form a long common channel (13 mm) which enters the duodenum.
Figure 3. Three ERCP images showing the definition of a short common channel (short CC: channel length 3 mm), a long common channel (long CC: channel length 12 mm) and anomalous pancreaticobiliary ductal union (anomalous pancreaticobiliary ductal union: channel length 4 cm). CC: common channel; PBDU: pancreaticobiliary ductal union
Overall, 2,100 ERCPs were available for study. In the first study phase, 1,473 were excluded from further evaluation as either only asingle duct had been filled (bile duct alone in 990 and pancreatic duct alone in 460) or the pancreaticobiliary junction was not clearly identified on the ERCP images (in 23). The remaining 627 formed the study group. These included 21 patients with tropical calcific pancreatitis, 174 patients in control group (no biliary or pancreatic diseases), 35 patients with alcohol-induced chronic pancreatitis, 317 patients with benign gallbladder disease, 14 patients with acute pancreatitis, 47 patients with gallbladder cancer, 10 patients with pancreatic cancer and 9 patients with a choledochal cyst. For this study, we evaluated the ERCPs of the 21 patients having tropical calcific pancreatitis and compared them with the 174 control subjects and the 35 patients with alcoholinduced chronic pancreatitis for pancreaticobiliary ductal union.
Tropical calcific pancreatitis was diagnosed when there were unique clinical, biochemical and radiological features. These included: i) recurrent abdominal pain; ii) diabetes mellitus; iii) large ductal calculi seen on plain film and other imaging tools (Figure 4) and iv) no history of alcohol or other metabolic or structural causes of chronic pancreatitis. The control group included patients in whom ERCPs had been performed but were found to have diseases unrelated to the biliary tract or pancreas. Alcohol-induced chronic pancreatitis included patients in whom ERCPs showed features of chronic pancreatitis and were etiologically related to alcohol as per the above-mentioned criteria [24, 25].
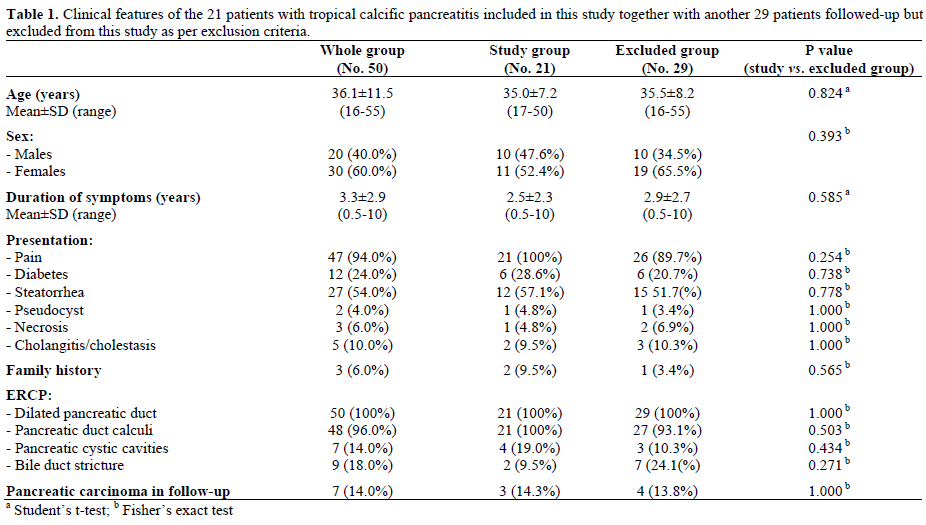
In all, we studied and followed up 50 patients with tropical calcific pancreatitis. All such patients had ERCPs available. Twenty-nine patients were excluded from the study due to the above-mentioned exclusion criteria. The clinical, biochemical and radiological features, and the follow-up of the 21 patients of the study group and 29 other patients with tropical calcific pancreatitis not included in this study are shown in Table 1. The two groups were comparable. This suggested that our study group was representative of the profile of tropical calcific pancreatitis in our community.
Written informed consent explaining the indications, adverse affects and alternatives was obtained from all patients before the ERCP was carried out. The study protocol was submitted to the ethical committee of Dr. Khuroo’s Medical Clinic and was approved. The study protocol conformed to good medical practice as defined in the Helsinki principles.
Comparisons of the categorical variables were analyzed using the Fisher’s exact test. Comparisons of the continuous variables were analyzed using the Student’s t-test. In addition, odds ratios were computed from the coefficients and their 95% confidence intervals were calculated. All values are expressed as mean±SD and frequencies. The statistical analysis was carried out using SPSS for Windows (version 13.0). Two-tailed P values less than 0.05 were considered significant.
The distribution of pancreaticobiliary ductal union in 174 control group patients with no pancreaticobiliary disease was as follows: separate opening in 86 (49.4%), a short common channel in 50 (28.7%), a long common channel in 32 (18.4%) and anomalous pancreaticobiliary ductal union in 6 (3.4%). In contrast to the control group, the distribution of pancreaticobiliary ductal union in the 21 patients with tropical calcific pancreatitis was as follows: separate opening in 5 (23.8%; P=0.036; OR=0.32, 95% CI: 0.11-0.91), a short common channel in 1 (4.8%; P=0.017; OR=0.12, 95% CI: 0.02-0.95), a long common channel in 7 (33.3%; P=0.144; OR=2.22, 95% CI: 0.83-5.94) and anomalous pancreaticobiliary ductal union in 8 (38.1%; P<0.001; OR=17.2, 95% CI: 5.19- 57.2) (Table 2). The data suggest that separate openings and a short common channel were less often seen in tropical calcific pancreatitis as compared to the control group and a long common channel and anomalous pancreaticobiliary ductal union were more often seen in tropical calcific pancreatitis patients as compared to the control group. The type of anomalous pancreaticobiliary ductal union in the 2 groups was different: 6 (75.0%) of the 8 patients with tropical calcific pancreatitis had the B-P type of anomalous union in contrast to the control group in whom five (83.3%) of the 6 patients had the P-B type of anomalous union (P=0.103; OR=15.0, 95% CI: 1.03- 218). The bile duct had joined the pancreatic duct in the neck region in one, the body region in 4 and the distal body/tail region in one patient (Figure 5). The angle of union of the anomalous pancreaticobiliary ductal union was also significantly different in tropical calcific pancreatitis patients (88.1±36.2°) than in control group (20.0±11.5°) (P<0.001). Patients with tropical calcific pancreatitis had significantly (P<0.001) longer anomalous channels (26.6±12.2 mm) than did those in the control group (19.6±6.1 mm).
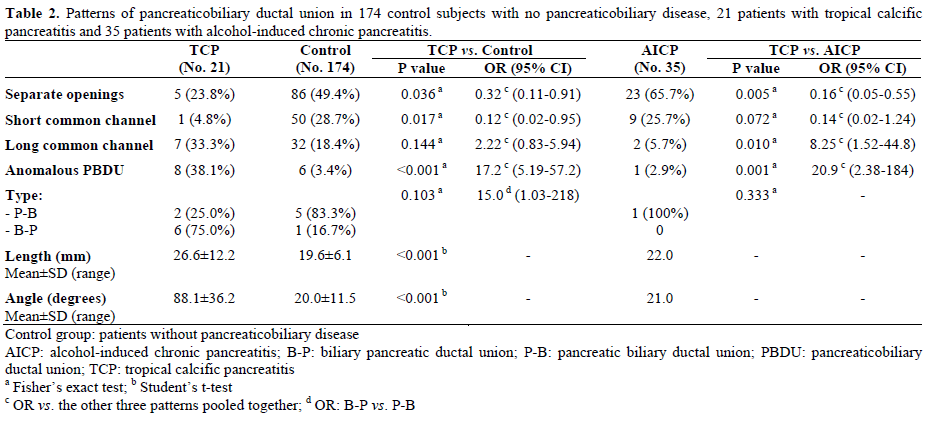
Figure 5. Tropical calcific pancreatitis. a. ERCP image showing a grossly dilated pancreatic duct with filling defects in the side branches and a dilated bile duct joining it in the pancreatic neck region (arrow) to form anomalous pancreaticobiliary ductal union of the B-P type. b. ERCP image showing a grossly dilated pancreatic duct with multiple large filling defects and the bile duct joining it in the body region (arrow) to form anomalous pancreaticobiliary ductal union of the B-P type. c. ERCP image showing a grossly dilated pancreatic duct with filling defects in the side branches and the bile duct joining it in the distal body region (arrow) to form a very long anomalous pancreaticobiliary ductal union of the B-P type.
The distribution of the pancreaticobiliary ductal union in the 35 alcohol-induced chronic pancreatitis patients was as follows: separate opening in 23 (65.7%), a short common channel in 9 (25.7%), a long common channel in 2 (5.7%) and anomalous pancreaticobiliary ductal union in 1 (2.9%). In contrast to this group, the distribution of pancreaticobiliary ductal union in the 21 patients with tropical calcific pancreatitis was as follows: separate opening in 5 (23.8%; P=0.005; OR=0.16, 95% CI: 0.05-0.55), a short common channel in 1 (4.8%; P=0.072; OR=0.14, 95% CI: 0.02-1.24), a long common channel in 7 (33.3%; P=0.010; OR=8.25, 95% CI: 1.52-44.8) and anomalous pancreaticobiliary ductal union in 8 (38.1%; P=0.001; OR=20.9, 95% CI: 2.38-184) (Table 2). The data suggest that separate openings and a short common channel were less often seen in tropical calcific pancreatitis as compared to alcohol-induced chronic pancreatitis, and a long common channel and anomalous pancreaticobiliary ductal union were more often seen in tropical calcific pancreatitis patients as compared to alcohol-induced chronic pancreatitis.
The etiology of tropical calcific pancreatitis in tropical countries has generally remained obscure [10, 11]. Early on, malnutrition, genetic and environmental factors, such as cassava, were thought to be important in the pathogenesis of tropical calcific pancreatitis [26, 27, 28]. These links have recently been found to have only a weak association with the disease and pancreatic secretory trypsin inhibitor (PTSI, unigene name: serine protease inhibitor, Kazal type 1; SPINK 1, a 56-AA peptide, has been identified [29, 30]. This is synthesized by acinar cells. SPINK1 gene mutations result in a loss of function and predispose to early trypsin activation and pancreatitis. The SPINK1 mutation occurs in the general population with allele frequencies of 1 to 2% and in a high percentage of recurrent acute pancreatitis and chronic pancreatitis patients in Western countries. The SPINK1 mutation occurs in 45% of patients with tropical calcific pancreatitis. However, the low penetrance of this gene does not indicate a primary etiologic role. Instead, the gene mutation may act as a disease modifier [31, 32]. Thus, there must be additional factors, which may be primary or secondary factors of importance, in the etiology of tropical calcific pancreatitis.
Pancreaticobiliary ductal union is the confluence of the pancreatic duct and the bile duct, and this union has many variations [14, 15]. The ducts may open into the duodenum separately or join together in the duodenal wall before entering the duodenum. The common channel may be short (length less than 6 mm) or long (length ranging 6-15 mm). In a small percentage, bile and pancreatic ductal union may occur outside the duodenal wall (length of channel greater than 15 mm) and is therefore not under the influence of the sphincter of Boyden. This pattern of ductal union is classified as anomalous pancreaticobiliary ductal union [21]. Anomalous pancreaticobiliary ductal union is further divided into the P-B type (pancreatic duct appears to join bile ducts) and the B-P type (bile ducts appears to join pancreatic ducts). The angle at which two ducts meet is also relevant [15, 23].
The pattern of pancreaticobiliary ductal union has been associated with many pancreaticobiliary diseases. The classic example of these is a choledochal cyst [33, 34, 35]. High percentages of patients with choledochal cysts have anomalous pancreaticobiliary ductal union of the P-B type. The exact mechanism of cystic dilatation of the bile ducts in this entity is not known. It has been proposed that, due to the union of the ducts outside the duodenum, there is maldevelopment of the sphincter of Oddi which results in a reverse pressure gradient between the common bile ducts and the main pancreatic duct.
This leads to regurgitation of the pancreatic juice into the bile ducts, repeated attacks of cholangitis and ectasia of the ducts. In fact, the amylase content of the bile in most patients with choledochal cysts has been reported to be high. Carcinoma of the gallbladder has also been associated with anomalous pancreaticobiliary ductal union of the P-B type [36]. It is postulated that regurgitation of the pancreatic juice leads to chronic inflammation, metaplasia of the biliary epithelium and, eventually, to gallbladder cancer.
We found that patients with tropical calcific pancreatitis had a high prevalence of anomalous pancreaticobiliary ductal union. The anomalous union in tropical calcific pancreatitis patients was long, of the B-P type in 6 out of 8 patients and presented a wide angle of union. What could the possible mechanism of pancreatic ductal and parenchymal damage due to this type of anomalous pancreaticobiliary ductal union be?
We believe this pattern of anomalous union should encourage the flow of bile into the pancreatic ducts rather than pancreatic juice into the bile ducts as seen in choledochal cysts. Bile salts can induce pancreatitis and, in the long run, lead to transformation into chronic pancreatitis and stone formation. Apart from anomalous union, 7 patients with tropical calcific pancreatitis had a long common channel which may also encourage regurgitation of bile into the pancreatic ducts.
The alcohol-induced chronic pancreatitis patients in our study had a predominance of separate openings or short common channels. Studies reported in the literature have shown a similar pattern of pancreaticobiliary ductal union in such patients [15]. It is hypothesized that separate openings of the common bile duct and the main pancreatic duct are associated with hyperplasia of the pancreatic ductular epithelium. Chronic alcohol worsens hyperplasia of the pancreatic ductular epithelium and causes an increase in pancreatic juice leading to obstructed ducts and precipitation of the protein plugs. Thus, the mechanisms of pancreatic injury in alcohol-induced chronic pancreatitis and tropical calcific pancreatitis differ from each other.
As mentioned above, the SPINK1 mutation occurs in 45% of patients with tropical calcific pancreatitis. However, the low penetrance of this gene does not indicate a primary etiologic role. Instead, gene mutation may act as a disease modifier. We believe that tropical calcific pancreatitis may be due to the combination of an underlying genetic defect and a structural abnormality of the pancreatic and bile ductal union.
All authors have no conflict of interest in conducting this study
the study was funded by research grants from Dr. Khuroo’s Medical Clinic. Authors 1 and 2 reviewed the ERCPs and reported on computer generated forms; Authors 3 compiled data, did statistical work and helped in writing the manuscript; all three authors reviewed the manuscript, made corrections, checked references and processed the manuscript