Milin Patel1, Tusharsindhu Chauhan2* and Vimal Amin3
1Department of Gastroenterology and Hepatology, Carolinas Healthcare System, Charlotte, NC, USA
2Allied Gastrointestinal Associates, Department of Gastroenterology, Virtua Hospital, Voorhees, NJ, USA
3Department of Gastroenterology, Springs Memorial Hospital, Lancaster, SC, USA
*Corresponding Author:
Tusharsindhu Chauhan
Department of Gastroenterology
Virtua Hospital, Voorhees
NJ, 08103, USA
Tel: +1 856-247-3000
E-mail: tc_chauhan@yahoo.com
Received Date: May 17, 2017 Accepted Date: June 19, 2017 Published Date: June 21, 2017
Citation: Patel M, Chauhan T, Amin V (2017) APC Treatment Resulting in Pneumoperitoneum; Perforation or Just Escape of Luminal Gas? J Clin Gastroenterol Hepatol 1: 2. doi: 10.21767/2575-7733.1000018
Argon plasma coagulation (APC) is an electrocoagulation technique commonly used for treatment of gastrointestinal bleeding secondary to arteriovenous malformations (AVMs). Although this modality is generally safe, a rare complication reported is perforation. We present an elderly female, who was found to have multiple colonic AVMs which were treated with APC, however, resulted in complication of pneumoperitoneum. With absence of peritonitis and hypotension, patient was treated with needle decompression of the peritoneal space, bowel rest, and antibiotics, which resulted in a successful recovery in the absence of surgical intervention.
Keywords
Plasma coagulation; Electrocoagulation; Muscularis propria; Submucosal vessels.
Introduction
AVMs are aberrant sub-mucosal vessels caused by chronic, intermittent low-grade obstruction of sub-mucosal veins at the level of the muscularis propria. They account for approximately 6% of lower gastrointestinal bleeds, and are predominately found in the proximal colon, where wall tension is the greatest. While iatrogenic perforation occurs in approximately 1 in 3000 solely diagnostic colonoscopies, the risk of perforation grows with increasing extent of the intervention [1]. Only nine cases of colonic perforation secondary to APC treatment have been published since 2007, none of which were reported in the United States. [2,3].
Case Report
63-year-old female with history of a colonic AVM presents with hematochezia and drop in hemoglobin from 14 to 11.5 g/dL. Colonoscopy was performed and revealed a small sigmoid polyp, which was removed using cold biopsy forceps. There was one AVM in the ascending colon, which appeared to have a feeding vessel. An endoclip was placed to control the bleeding and argon plasma coagulation (APC) was used to destroy the area. An 80% destruction of that AVM was achieved. There was minor bleeding from the area of destruction and a second endoclip was placed. There were two more AVMs in the cecum. The larger AVM was injected with epinephrine and once the bleeding was under control, APC was used to destroy all the visible area. The second cecal AVM was also treated with APC with flushing.
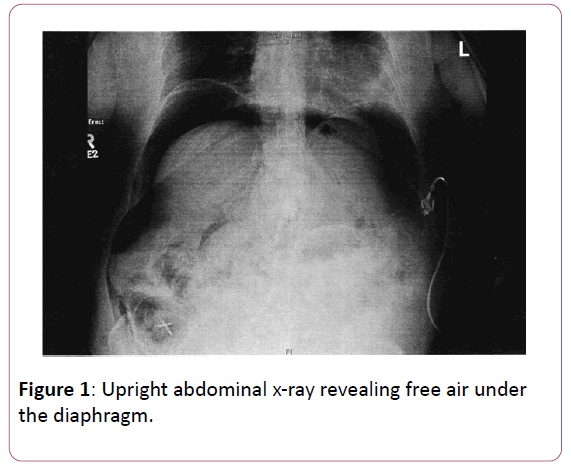
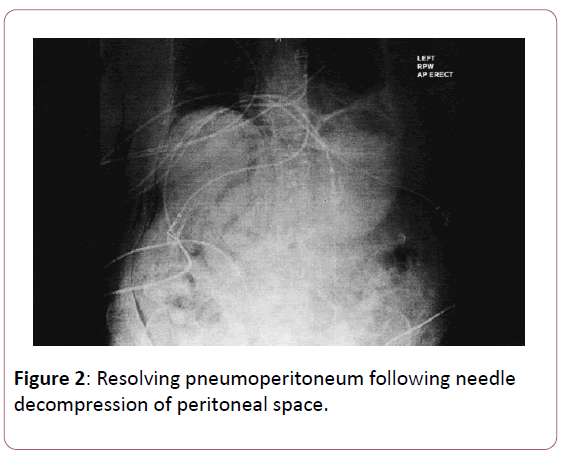
Following the colonoscopy, patient was complaining of pain in the right lower quandrant. The exam at the time was consistent with soft, but distended abdomen with mild tenderness to the right lower quandrant. An upright abdominal x-ray revealed free air under the diaphragm (Figure 1). Patient underwent immediate needle decompression of the peritoneum, with successful evacuation of free air (Figure 2). Patient was treated with bowel rest, intravenous fluids, and ten days of intravenous ceftriaxone and metronidazole. Follow up CT enterography was negative for extravasation of contrast.
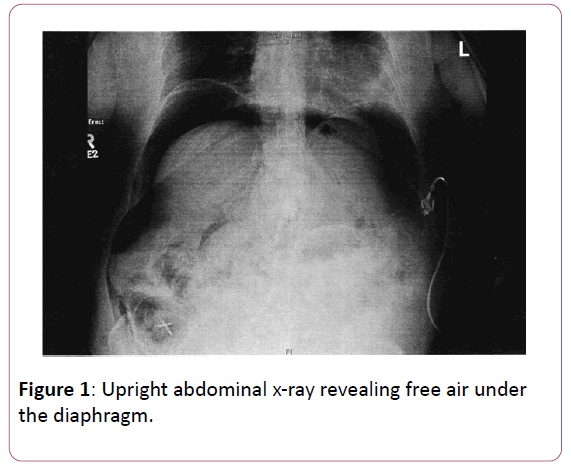
Figure 1: Upright abdominal x-ray revealing free air under the diaphragm.
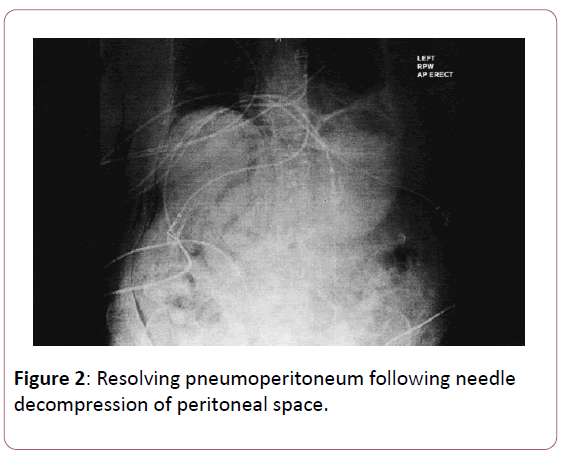
Figure 2: Resolving pneumoperitoneum following needle decompression of peritoneal space.
Discussion
Argon plasma coagulation is a noncontact electrocoagulation technique used to control gastrointestinal bleeding. It is suggested to maintain an operative distance of 2 to 8 mm from probe to tissue, and performed by applications of 0.5 to 2 sec duration as per Grund and Naamua [4,5]. The theoretical advantages of APC include its ease of application, rapid treatment of multiple lesions in the case of arteriovenous malformations or wide areas (the base of resected polyps or tumor bleeding), safety due to reduced depth of penetration, and lower cost compared to laser by Cohen [6]. A full colon preparation is recommended when performing APC, even in the rectum and sigmoid colon, due to the risk of colonic gas explosion from inadequate preparation as studied by Ladas [7]. Although, use of APC is generally safe, perforation following APC therapy as reported by Manes et al. [8]. APC colonic perforation occurs at a rate of 0.27% out of 1062 patients, and only nine cases have been published in literature since the year 2007 [2,3]. The authors have reported ten minor complications, most commonly subcutaneous emphysema. Transmural bowel wall injury can lead to pneumoperitoneum, an abnormal presence of air or other gases in the peritoneal cavity. As free gas accumulates in the peritoneal cavity it can compress intraabdominal veins or lead to respiratory insufficiency by compromising diaphragmatic function, a phenomenon known as tension pneumoperiteonum as studied by Addison [9]. Diagnosis of pneumoperitoneum after APC should not automatically mean that there is a perforation. Contact of the probe with the mucosa, thermal injury, and a high argon flow can all lead to transfer of gas through the gastrointestinal wall without the macroscopic correlate of a visible lesion as per Manes et al. [8]. Conservative therapy is considered first line treatment with air in the peritoneum after APC, with surgery considered for those with signs of peritoni ti s [8]. Our patient was treated with needle decompression of the peritoneum, intravenous fluids, bowel rest, and ten days of intravenous antibiotics, resulting in a successful recovery.
Conclusion
In conclusion, APC is a widely used hemostatic method to control gastrointestinal bleeding in the setting of AVMs. Colonic perforation is a rare complication, and in the absence of hemodynamic compromise and peritonitis, treatment is primarily conservative.
References
- Raju GS, Saito Y, Matsuda T, Kaltenbach T, Soetikno R (2011) Endoscopic management of colonoscopic perforations (with videos) Gastrointest Endosc 74: 1380–1388.
- Prost B, Poncet G, Scoazec JY, Saurin JC (2004) Unusual complications of argon plasma coagulation. Gastrointest Endosc 59: 929-31.
- Grund KE, Zindel C, Farin G (1998) Argon plasma coagulation (APC) in flexible endoscopy: Experience with 2193 applications in 1062 patients. Gastroenterology 114: A603.
- Grund KE, Storek D, Farin G (1994) Endoscopic argon plasma coagulation (APC) first clinical experiences in flexible endoscopy. Endosc Surg Allied Technol 2: 42-46.
- Nakamura S, Mitsunaga A, Murata Y, Suzuki S, Hayashi N (2001) Endoscopic induction of mucosal fibrosis by argon plasma coagulation (APC) for esophageal varices: A prospective randomized trial of ligation plus APC vs. ligation alone. Endoscopy 33: 210-215.
- https://www.uptodate.com/contents/argon-plasma-coagulation-in-the-management-of-gastrointestinal-hemorrhage
- Ladas SD, Karamanolis G, Ben-Soussan E (2007) Colonic gas explosion during therapeutic colonoscopy with electrocautery. World J Gastroenterol 13: 5295-5298.
- Manes G, Imbesi V, Bianchi-Porro G (2007) Pneumoperitoneum after argon plasma coagulation treatment: perforation or accumulation of air in the cavity? Endoscopy 39: E98.
- Addison NV, Broughton AC (1976) Tension pneumoperitoneum: A report of 4 cases. Br J Surg 63: 877.