What is known on this subject
• Inequalities exist in maternal and fetal outcomes.
• Patient and public involvement is a central feature of effective healthcare services.
• The exploratory nature of qualitative research methods is suitable for applied research.
What this paper adds
• The needs of the target group must be assessed throughout the research process.
• To ensure that the most suitable data collection tools and methods are used, researchers must be consistently reflective of their own motivations and the needs of their target groups.
• Researchers must be flexible and open to change if an imbalance is found between the chosen research
method and the target group.
Keywords
‘at-risk’ groups, maternity care, qualitative research methods
Introduction
Patient and public involvement in healthcare and
healthcare services is a key feature of health policy in
the UK. Patients have the right to be involved in decisions
about their care and treatment. The Department of Health recognises that patients are the experts on
their own care, and patient satisfaction is a very
important factor in ensuring adherence to care and
treatment regimes (Department of Health, 2001; Darzi, 2007). Feedback from patients enables service
providers to determine whether services are truly
accessible and meet the needs of the population for
which they are intended.However, it is not always easy
to gather feedback from some service users, especially
those most at risk of adverse health outcomes. This
group of people are often collectively regarded as ‘at
risk.’ Numerous characteristics can make a person
more at risk of adverse health outcomes. Two such
examples are area deprivation and ethnicity. There are
extensive findings which link relative deprivation (e.g.
Marmot et al, 1991; Marmot, 2005; Marmot and
Wilkinson, 2006) and ethnicity (Bharj and Salway,
2008) to adverse health outcomes in the general
population in the UK.
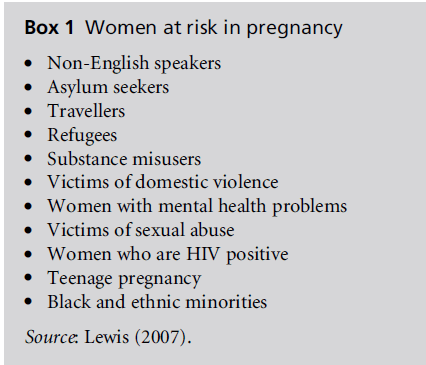
In maternity services, the term ‘at risk’ is applied
to women who are considered to have a higher than
normal risk of adverse outcomes as a result of pregnancy
(see Box 1). Several reports indicate that some
groups of women are more likely than others to
experience inequalities in maternal and fetal health
outcomes (Confidential Enquiry into Stillbirths and
Deaths in Infancy, 2001; Lewis, 2007). Specifically,
individual and area-level deprivations are associated
with worse birth outcomes (Luo et al, 2006). The
prevalence of adverse outcomes such as gestational
diabetes and hypertension has been associated with
ethnicity (Shen et al, 2005). For example, maternal
obesity is linked to numerous adverse maternal and
fetal outcomes. It is highest in women of lower socioeconomic
status and among some ethnic groups
(Kinra et al, 2000). Engagement with healthcare professionals
and health services tends to be lower in these
at-risk groups of women than for other women
(Lewis, 2007). These findings support the extensive
literature that links deprivation to adverse health
outcomes.
Box 1 :Women at risk in pregnancy
The vision of world class commissioning sees the
NHS focusing on ‘better care for all’ (Department of
Health, 2007, p. 4). Patient engagement is central to world class commissioning because it allows the health
service to understand the needs of the public. However,
at-risk groups are not generally represented in
initiatives that involve collaboration between service
users and professionals (Craig, 1998). For example, in
a survey of 2406 women undertaken by the Audit
Commission, younger women (aged under 25 years),
unemployed women and those with no educational
qualifications were under-represented (Audit Commission,
1998). As a result, the voice of those women
is not heard and their needs are not included in the
design of healthcare. To ensure that interventions can
target the women who are most at risk of adverse
outcomes, healthcare services research must explore
why the people who are most likely to suffer from the
worst health outcomes are those who are also least
likely to engage in research and share their experiences.
Only then will researchers and healthcare professionals
be able to start to understand which strategies
will maximise the participation of these groups in
healthcare services. This reflective paper presents a discussion
of the authors’ personal experiences of conducting
maternity care research, specifically collecting
qualitative data from at-risk samples, and offers
suggestions for best practice when working with these
groups.
The discussion is based on issues arising from
qualitative approaches, which are frequently used in
midwifery and health services research and which are
well suited to examining why certain groups of people
are at risk for certain adverse health outcomes. Qualitative
methods allow people’s experiences to be heard
directly from them and in their ownwords. Reflexivity
is an important feature of qualitative research, as it
enables researchers to reflect on possible ways in which
they have influenced the research (personal reflexivity)
and possible ways in which assumptions that have
been made during the research process (e.g. research
questions) have affected the data and results (epistemological
reflexivity) (Willig, 2001). This paper includes
discussion about the outcome of both authors’ reflexivity
at key points in the research process.
Highlighting the sample and
designing a recruitment strategy
The first stage in research is to highlight the target
sample and design a sample frame that will be productive
in identifying and recruiting participants.
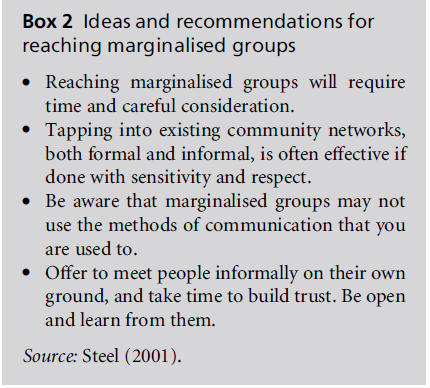
Reaching at-risk groups and involving them in research
requires tenacity and a more proactive approach than
when recruiting other sample groups. Researchers may
have to invest a lot of time to gain an understanding
of the culture of the population and thus be able to successfully engage them in research. Purposive sampling
is often used to ensure recruitment of participants
from each target group. The best way to do this,
according to Steel (2001), is through the use of local
networks, including local councils, community voluntary
services, local libraries, community centres, local
gatherings and word-of-mouth networking (see Box 2).
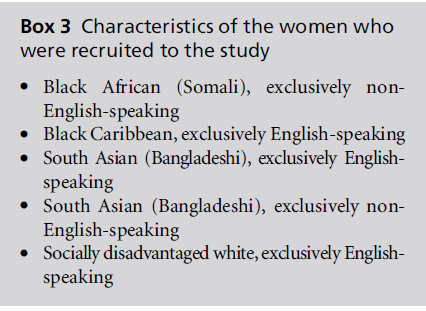
The authors of this paper were both recently
involved in a study examining the antenatal experiences
of at-risk pregnant women (Raine et al, 2010).
The study took place at one NHS Trust (i.e. hospital in
Central London, England). The study aimed to recruit
a sample that reflected the populations identified as at
risk in the NHS trust (see Box 3).
English- and non-English-speaking groups were
recruited for the Bengali and Somali groups because,
when English-speaking women attend mixed-language
focus groups with non-English-speaking women from
the same ethnic background, the English speakers tend
to dominate the responses and attempt to interpret the
responses of the other women (Richens, 2003). Moreover,
the experiences of healthcare services differ greatly
for women who are unable to communicate in English,
especially in terms of the way that they are treated by
healthcare professionals (Richens, 2003).
Box 2:Ideas and recommendations for
reaching marginalised groups.
Box 3:Characteristics of the women who
were recruited to the study.
Women were recruited to the study using the
framework suggested by Steel (2001). Community
midwives were viewed as the key gatekeepers, so a
series of meetings was arranged to inform them about
the aims and objectives of the study. This also helped
to make contacts, build relationships and identify
possible facilities, such as rooms for focus groups
and cre`che facilities.
The midwives were asked to inform women of the
purpose of the study and explain what participation
would involve. The plan was that women who were
interested in taking part would then meet with one
of the researchers, who would explain the study in
more detail, and if the women were still interested in
participating, their preferred contact details would be
taken. Both the information sheet and the researcher
informed the women that transport would be provided
in the form of a pre-booked taxi or reimbursement
of a day travel card. Approval from the NHS
Research Ethics Committee (REC) required that women
were given a minimum of 24 hours before consenting
to participation in the study. The women were asked
to indicate when it would be convenient to attend
a focus group, and were told that they would be
contacted by a member of the research team with
focus group dates. To ensure that the women received
all of the relevant information to enable them to make
an informed decision about their participation in the
study, the information sheet and invitation letter were
translated into Bengali and Somali. Women who
could not read were contacted by telephone by a
member of the research team who spoke Bengali or
Somali. The research team attended antenatal clinics
on a regular basis, and had a good relationship with
the community midwives. In addition, posters and
information sheets about the research study were
displayed in antenatal clinics and Sure Start children’s
centres.
Reflection on the recruitment strategy
The recruitment strategy was successful to the extent
that a small number ofwomen expressed an interest in
participating and were keen to give the researchers
their contact details. However, the majority of the
women who provided their contact details were from
white, educated backgrounds, and there was a lack of
response from women in the at-risk groups. The
research team were very aware of the need to be
reflexive throughout the research process, and scheduled
regular meetings to enable this to occur (as
supported by Mauthner and Doucet, 2003). Reflecting
on the recruitment strategy indicated two possible
reasons for the lack of interest shown by the majority
of the women who were approached about the study,
and in particular the at-risk women. First, the REC required the researchers to give the women at least 24
hours to consider participation before consenting to
the study and taking part in a focus group. A number
of women reported being busy with work and family
responsibilities. They were keen to take part in the
study while waiting for their appointment, for which
they had made work and childcare provision, but were
not willing to return to participate at a later date.
Secondly, in order to identify women who could be
approached about the study, the research team had to
rely heavily on the help and support of the midwives
and other key gatekeepers, such as community group
leaders. The midwives and direct contact with the
research team in maternity clinics were found to be the
most successful recruitment routes. This finding is
supported by a recentUK study which found that UKborn
migrants are less likely than non-UK-born migrants
to be recruited through community groups.
Rapport and the relationship between the researcher
and the UK-born migrants were more important in
successful recruitment (Twamley et al, 2009). However,
midwives are extremely busy in their clinical
roles, and are not always able to fulfil the added
responsibility of identifying prospective participants
for researchers. They may view the extra work negatively,
which means that recruitment may take longer
(Kinnunen et al, 2008). Following these reflections,
the consultant midwife (YR) became involved in the
recruitment process. Initially she had not been involved,
as it was generally felt that her role at the hospital from
which women were recruited might create a bias and
deter women from taking part. These changes led to
successful recruitment of women from all ethnic
groups.
In a subsequent maternity care study, one of the
authors (DS) has experienced successful recruitment
rates due to the employment of full-time research
midwives. Using full-time research midwives to recruit
women for maternity care studies has three
advantages. First, the research midwives understand
the maternity care pathway and the logistics of the
clinics in the hospital and community setting. Secondly,
they are sensitive to women’s unique pregnancy
needs, and pregnant women are more receptive to
research midwives because they perceive them to be
the most appropriate people to care for them during
their pregnancy. Thirdly, midwives tend to have good
links within the hospital and clinical setting, and
midwives working in the clinical area and community
teams are more receptive to research midwives, due to
their shared interests and knowledge.
The data collection method: focus groups
Another aspect of recruitment was the use of focus
groups as the data collection method. A focus group
consists of an in-depth, open-ended group discussion
that explores a specific set of issues associated with a
predefined topic and a homogenous group of participants.
A distinguishing feature of the focus group
method is the group dynamic and interaction between
participants (Kitzinger, 1994). Focus groups are convened
under the guidance of a facilitator, who allows a
free-flowing discussion to occur between the participants
(Howard et al, 1989). Focus groups provide
direct feedback and can be used as a way of obtaining
rich information within a particular social context.
The focus group method has been used for many years
to elicit people’s experiences of disease and of health
services (Barbour and Kitzinger, 1999). During the
discussion the participants hear other focus group
members’ responses to the questions, and make comments
of their own (Chui and Knight, 1999). The
groups are not required to reach any kind of consensus,
but simply allow a group of individuals to clarify
their views and thoughts in ways that would not be
possible in a one-to-one interview. This process of
sharing, comparing and justifying viewpoints that
spontaneously occur between participants adds a level
of context, depth and self-interpretation that is difficult
to replicate via other qualitative data collection
methods.
Focus groups can facilitate the identification of
cultural values, and they have been identified as being
useful when researching ethnic minority groups
(Hennings et al, 1996; Duff, 1999; Wilkins Winslow
et al, 2002; Richens, 2003; Dorset County Council,
2006). They are commonly used to collect information
or to investigate individual responses to different
situations or policy initiatives, particularly those of a
sensitive nature (Grbich, 1999). They are particularly
useful for encouraging participation by people who
are reluctant to be interviewed on an individual basis
or who feel that they have nothing to contribute, and
for tapping into a given cultural context (Kitzinger,
1995).
Focus groups are well suited to exploration and
discovery when little is known about the beliefs and
attitudes that are held by individuals about a particular
topic (Morgan, 1998). Since little is currently known
about the reasons why some pregnant women use or
access antenatal care suboptimally, the focus group
method was considered to be the best option for the
London study.
Reflections on the data collection method
The successful use of focus groups: example of research with young parents
Young parents are a socially isolated and at-risk group.
As a result, there is a lack of understanding about
available support services for young parents, and many
barriers to accessing antenatal and postnatal care have
been described by young parents (Smith and Roberts,
2009a). The importance of specialist antenatal clinics
and support services that address young parents’
individual needs has been reported several times
(Peckham, 1993; Drife, 2004; Wiggins et al, 2005).
Focus groups were successfully used in previous research
by one of the authors (DS) with young parents
(Smith and Roberts, 2009b). In that study the research
question examined young parents’ experiences of
antenatal and postnatal support in order to ascertain
the reasons why they did or did not adhere to medical
advice and attend antenatal and postnatal services.
The main aim of the focus groups was to collect
qualitative data in order to clarify the findings highlighted
in survey data collected fromthe same group of
young parents. A focus group format was chosen to
enable the young parents’ cultural beliefs and perceptions
of antenatal care to be heard.
Recruitment took place in one London borough
through several gatekeepers, such as teenage pregnancy
coordinators and health visitors. It became
evident that the researcher needed to meet with the
young parents several times before inviting them to
attend the focus group. These meetings helped to
build rapport and trust between the researcher and
the participants, and were deemed to be a success, as
the required number of participants attended each
focus group. In addition, as many young parents
experience financial hardship, young parents were
given £15 in ASDA vouchers to thank them for giving
up two hours of their time to take part in the focus
group. The focus groups were designed in an informal
and semi-structured manner to encourage discussion
and comfort, and were run by a female researcher
(DS). A topic guide, including key questions and
prompts, was designed to ensure that important topics
raised in the questionnaire responses were addressed.
As they were an at-risk group and not likely to attend
antenatal and postnatal groups, precautions were
taken to make the parents feel at ease in the group
and to encourage discussion. This was achieved by
dividing the participants into smaller groups for the
first question of the focus group. They were then asked
in their small groups to write down their views on a
piece of flipchart paper. Subsequently these responses
were displayed to the whole group in order to facilitate
discussion. The researcher read out a few points from
the paper and participants were told that they could comment on or discuss these points at any stage. This
method was very successful, and the young parents
started discussions about the points as soon as these
were displayed to the whole group. This method also
helped the researcher at the analysis stage, as some of
the key themes were already written down on the
flipchart paper along with descriptions and quotations
from the young parents. Similar success with the
use of activities in the focus group setting with young
people has been reported by Colucci (2007). She
describes the use of activities such as the one highlighted
here as a way to collect in-depth data on
sensitive subjects, by enabling the participants to feel
more at ease with the focus group topic. In addition, a
beneficial effect on recruitment was suggested, as the
participants were more likely to recommend the study
to friends when these activities were used.
Barriers to using focus groups in the London study
In the London study of antenatal experience, women
were recruited froma number of different community
groups and clinics throughout the hospital catchment
area. Therefore it was decided that smaller focus
groups of 4 to 6 participants, instead of 10 to 12 group
members, would be used. However, the main problem
that arose involved trying to get women from the atrisk
groups to attend the focus groups in the first place.
Attendance was very low for these groups, despite the
enthusiasm of participants at the time of initial recruitment.
On one occasion this resulted in the
cancellation of a focus group for English-speaking
Bengali women. In contrast, the recruitment of ‘educated
white’ women was completed within one week.
The low attendance by members of at-risk groups led
the team to re-examine the recruitment strategy. On
reflection, there were a number of reasons for the low
consent and attendance rates.
First, women were not keen to return to participate
in the focus groups because of the time constraints and
childcare issues associated with this research method.
They were not able to commit to attending the university
for two hours because of busy schedules and
the need to care for their other children. Reflections on
this limitation resulted in changes to the protocol, and
an amendment was submitted to the NHS REC to
enable women to consent to participate at any stage
after they had been given a written and verbal explanation
of the study and had had time to consider their
participation. This recruitment strategy was very successful
and resulted in a large number of women, of all
ethnic groups, consenting to participate in the study
within a short period of time. In addition, recruitment
rates were highest when women were asked to participate
in the study by their midwife, rather than merely
being given the study information to read.
Secondly, the women were deterred by the amount
of time that was required for the focus groups, and by
the venue. The focus groups were scheduled to take
place at the university, a venue with which the women
were not familiar and which was some distance from
the community clinics where they were recruited.
Moreover, the distance travelled by the women to
get to the clinic and hospital may differ according to
both level of personal deprivation and ethnicity, and
this may explain the reluctance of the at-riskwomen to
attend the focus groups. For example, in an American
study, the time that it took to travel to receive healthcare
was significantly greater for African American
adults than for white Americans (Probst et al, 2007).
To overcome this barrier, taxis were arranged to
collect the women and, where possible, focus groups
were conducted in community centres that were
familiar to them.
Thirdly, following on from the difficulties involved
in arranging a time and location that were suitable for
a whole group of women, it was decided that interviews
would be included as an amendment to the NHS
REC. This overcame the obstacles of location and
time, as it allowed interviews to be conducted in
women’s homes and after their hospital appointments.
Fourthly, as suggested by Singer and Kulka (2000),
incentives were introduced to thank the women for
giving up their time to take part in the research, as
a way to increase participation. In this instance,
Mothercare vouchers were given to the women at
the end of the interview to thank them for giving up
their time. The women were found to respond positively
to this token of gratitude, and consequently the
recruitment rates for women from all ethnic groups
increased.
Finally, the gender of the researcher was important
to certain groups of women, and the research team
had to be sensitive to this. In the London study, the
necessity of a female researcher was demonstrated at
several points early in the study, and was therefore
adopted throughout the data collection phase. For
example, the Bengali and Somali women were not
comfortable with a male researcher being present at
recruitment, which resulted in low recruitment rates
at these times, nor were they comfortable with a male
researcher making the follow-up phone call, which
was seen as critical to recruitment (MacDougall and
Fudge, 2001). Finally, interpretation is very important
to ensure that questions and answers are correctly
translated. Misinterpretations of meaning in data can
occur for many reasons. A bias may arise due to the
motivation of the interpreter or to differences in
dialect. This was the case with the Bengali and Somali
women. In the cases where the interpreter also recruited
the women, several leading questions were evident
during the interviews, despite the fact that training had been given. A similar finding has been reported by
one of the authors in a previous study (Richens, 2003).
Conclusion
In conclusion, research with at-risk populations is
essential if inequalities in maternal and fetal outcomes
are to be addressed by maternity care. Qualitative data
collection is a suitable research method for applied
research, as it produces detailed and descriptive data
on the views and experiences of the sample. However,
engaging at-risk samples in qualitative research is a
challenge to researchers, and involves a greater investment
of time than research with other populations.
Researchers must understand the cultural and environmental
needs of their target group and use this
knowledge to constantly evaluate the success of their
recruitment strategy and data collection method. The
process of reflexivity is vital for understanding the
influence of the researcher and the research design on
data collection and analysis, and for highlighting any
imbalances between the participants and the current
research design. We must be mindful that our views
and motivations as researchers may differ from those
of the individuals we are trying to recruit and the
clinicians whose practice we are hoping to inform. If
we are aware of these differences, we are more likely to
be open to the needs of all involved in applied research
and to design a successful research protocol. This was
true of all the experiences of the authors as shared in
this paper. In addition, researchers must be aware that
in many healthcare service studies and qualitative
research studies the participants are self-selected and
may therefore have an extreme experience to share.
Thus caution must be exercised when analysing such
results.
The need to be reflexive at all stages of the research
process was highlighted in this short paper. This
reflexive practice enables researchers to identify barriers
and examples of best practice and design, and to
conduct effective and efficient research. The authors
believe that researchers have a responsibility both to
their study sample and to their research to explore the
cultural reasons for the success and failure of their
research method. They then need to share detailed
information about these successes and failures, to
ensure both that the evidence base for the research
method grows, and that examples of best practice are
available for all target populations, especially those at
greater risk of adverse health outcomes. Researchers
also need to find a strategy for communicating with
healthcare professionals in order to ensure optimal
recruitment of participants.
CONFLICTS OF INTEREST
None.
References
- Audit Commission (1998) First Class Delivery: a national survey of women’sviews of maternity care. London: Audit Commission.
- Barbour RS and Kitzinger J (eds) (1999) Developing Focus Group Research: politics, theory and practice. London: Sage Publications Ltd.
- Bharj KK and Salway SM (2008) AddressingEthnicInequalities in Maternity Service Experiences and Outcomes: responding to women’sneeds and preferences. London: Race EqualityFoundation.
- Chiu LF and Knight D (1999) How useful are focus groups for obtaining the view of minority groups? In: Barbour RS and Kitzinger J (eds) Developing Focus Group Research: politics, theory and practice. London: Sage Publications Ltd.
- Colucci E (2007) ‘Focus groups can be fun’: the use of activity-oriented questions in focus group discussions. Qualitative Health Research 17:1422–33.
- ConfidentialEnquiry into Stillbirths and Deaths in Infancy (CESDI) (2001) FifthAnnual Report. London: Maternal and Child Health Research Consortium.
- Craig G (1998) Women’sViews Count: building responsive maternity services. London: College of Health.
- Darzi A (2007) A Framework for Action. www.healthcare forlondon.nhs.uk/assets/Publications/A-Framework-for- Action/aFrameworkForAction.pdf NHS London
- Department for Communities and Local Government (2004) The English Indices of Deprivation 2004 (Revised). www.communities.gov.uk/index.asp?id=1128444 (accessed 10 February 2010).
- Department of Health (2001) The Expert Patient: a new approach to chronic disease management in the 21st century. www.dh.gov.uk/en/Aboutus/MinistersandDepartment Leaders/ChiefMedicalOfficer/ProgressOnPolicy/ ProgressBrowsableDocument/DH_4102757 (accessed 16 February 2009).
- Department of Health (2007) World Class Commissioning: vision. www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_080952.pdf (accessed 1 October 2010).
- Dorset County Council (2006) MinorityEthnic Groups in Dorset: a qualitative research study. www.dorsetcommunity action.org.uk/ethnic_minority_groups_dorset (accessed 18 October 2010).
- Drife J (2004) Teenagepregnancy: a problem or what? British Journal of Obstetrics and Gynaecology 111:763–4.
- Duff L (1999) Development of an interview questionnaire to measure satisfaction with maternity care in women from the Bangladeshi community in England. UnpublishedPhDthesis. London: London School of Hygiene and Tropical Medicine, University of London.
- Grbich C (1999) Qualitative Research in Health. London: Sage Publications.
- Healthcare Commission (2008) Maternity Services ScoredAssessment. www.healthcarecommission.org.uk/_db/_downloads/MaternityServicesReviewOrganisationResults _200801242628.xls (accessed 8 September 2009).
- Hennings J, Williams J and NaherHaque B (1996) Exploring the health needs of Bangladeshi women: a case study inusing qualitative research methods. Health Education Journal 55:11–23.
- Howard E, Huble Bank J and Moore P (1989) Employer evaluation of graduates: use of the focus group. Nurse Educator 14:38–41.
- Kinnunen TI, Aittasalo M, Koponen P et al (2008) Feasibility of a controlled trial aiming to prevent excessive pregnancy- related weight gain in primary health care. BMC Pregnancy and Childbirth 8:37.
- Kinra S, Nelder RP and Lewendon GL (2000) Deprivation and childhoodobesity: a cross sectional study of 20 973 children in Plymouth, United Kingdom. Journal of Epidemiology and Community Health 54:456–60.
- Kitzinger J (1994) The methodology of focus groups: the importance of interaction between participants. Sociology of Health and Illness 16:103–21.
- Kitzinger J (1995) Qualitative research: introducing focus groups. British Medical Journal 311:299–302.
- Lewis G (ed.) (2007) SavingMothers’ Lives: reviewingmaternaldeaths to make motherhoodsafer, 2003–2005. The Seventh Report on ConfidentialEnquiries into MaternalDeaths in the United Kingdom. London: ConfidentialEnquiry into Maternal and Child Health (CEMACH).
- Luo ZC, Wilkins R and Kramer MS (2006) Effect of neighbourhoodincome and maternaleducation on birth outcomes: a population-based study. Canadian Medical Association Journal 174:1415–20.
- MacDougall C and Fudge E (2001) Planning and recruiting the sample for focus groups and in-depth interviews. Qualitative Health Research 11:117–26.
- Marmot M (2005) Social determinants of health inequalities. Lancet 365:1099–104.
- Marmot M and Wilkinson RG (2006) Introduction. In: Marmot M and Wilkinson RG (eds) Social Determinants of Health, 2nd edn. Oxford: Oxford University Press. pp. 1–6.
- Marmot MG, Davey Smith G, Stansfeld SA et al (1991) Health inequalities among British civil servants: the Whitehall II study. The Lancet 337:1387–93.
- Mauthner NS and Doucet A (2003) Reflexiveaccounts and accounts of reflexivity in qualitative data analysis. Sociology 37:413–31.
- Morgan DL (1998) Focus Group Kit. ThousandOaks: Sage Publications.
- Peckham S (1993) Preventingunintendedteenagepregnancies. Public Health 107:125–33.
- Probst JC, Laditka SB, Wang JY et al (2007) Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National HouseholdTravel Survey. BMC Health Services Research 7:40.
- Raine R, Cartwright M, Richens Y et al (2010) A qualitative study of women’sexperiences of communication in antenatal care: identifying areas for action. Maternal and Child Health Journal 14:590–99.
- Richens Y (2003) Exploring the Experiences of Women of PakistaniOrigin of UK Maternity Services. London: Department of Health.
- Shen JJ, Tymkow C and MacMullen N (2005) Disparities in maternaloutcomes among four ethnic populations. Ethnicity and Disease 15:492–7.
- Singer E and Kulka RA (2000) PayingRespondents for Survey Participation. Survey Methodology Program WorkingPaperNo. 092. Ann Arbor, MI: Survey Research Center, Institute for Social Research, University of Michigan.
- Smith D and Roberts R (2009a) Young parents’ perceptions of barriers to antenatal and postnatal care. British Journal of Midwifery 17:620–27.
- SmithDand Roberts R (2009b) Social acceptance: a possible mediator in the association between socio-economicdeprivation and under-18 pregnancy rates? Journal of YouthStudies 12:669–83.
- Steel R (2001) InvolvingMarginalised and Vulnerable Groups in Research: a consultation document. www.invo.org.uk/ pub.htm (accessed 9 October 2003).
- Twamley K, Puthussery S, Macfarlane A et al (2009) Recruiting UK-bornethnicminority women for qualitative health research – lessonslearned from a study of maternity care. Research Policy and Planning 27:25–38.
- Wiggins M, Oakley A, Sawtell M et al (2005) TeenageParenthood and Social Exclusion: a multi-method study. Summary report of findings. London: Social Science Research Unit Report, Institute of Education.
- Wilkins Winslow W, Honein G and Eluzubeir MA (2002) The use of focus groups with an Arab population. Qualitative Health Research 12(4):566–77.
- Willig C (2001) Introducing Qualitative Research in Psychology. Buckingham: Open University Press.