Research Paper - (2009) Volume 17, Issue 5
Lecturer in Economics, School of Economics, University of Queensland, Australia
Received date: 16 June 2009; Accepted date: 27 August 2009
Background This study considers the factors that affect service provision for individuals who present to out-of-hours (OOH) primary care services in the Republic of Ireland and Northern Ireland. The organisations under consideration are known as OOH co-ops. Specifically, an individual can potentially receive one of four services: nurse advice, doctor advice, a treatment centre consultation or a home visit. Aim The principal aim was to investigate whether service provision was consistent across co-ops once patient characteristics, patient complaints and other covariates were controlled for. In this paper, service provision was seen as a necessary but not sufficient condition for quality. Methods A multinomial logit approach was used to model the choice between the three services offered by co-ops. Results The results indicate that service provision was relatively homogenous across co-ops. Conclusions Quality was consistent across co-ops in terms of service provision. Therefore the next step is to consider whether quality within the treatment received varies. Nevertheless, the result provides some support for using OOH co-ops as a means to provide OOH primary care.
consistent care, co-ops, out of hours, primary care.
How this fits in with quality in primary care
What do we know?
There is considerable variation in the mode of treatment patients receive in general practice, over and above their individual and illness characteristics, including in out-of-hours primary care services.
What does this paper add?
This study shows that out-of-hours primary care co-operatives in Northern Ireland and the Republic of Ireland provide nurse advice, doctor advice, a treatment centre consultation or a home visit consistently across centres when individual and illness characteristics are taken into account.
When a patient approaches a medical facility anumber of factors determine the type of treatment received. These factors include patient, complaint and medical facility characteristics. This paper aims to investigate if the type of treatment received by individuals who approach organisations that supply primary care outside normal working hours in Northern Ireland (NI) and the Republic of Ireland (ROI) varies above and beyond their own complaint and characteristics. For example, it is possible that the type of treatment a patient receives is a function of the staff member that they encounter. Ideally, the type of care received by patients would not vary with medical facility characteristics, given that this suggests variations in quality of care –which includes the type of treatment received, whether this is nurse advice, doctor advice, a treatment centre consultation or a home visit. The importance of this is reflected in the number of patients who use out-of-hours (OOH) services, approximately 957 279 per annum in NI and ROI (this calculation is based on data relating to six out of seven NI OOH co-operatives (co-ops) and eight out of 12 OOH coops in ROI and the relative populations that they supply care to; adjustments are made for the area of Dublin, Ireland where OOH co-ops only serve the minority of the population). In addition, it is also reflected in the importance of having formal arrangements for OOH primary care to allow general practitioners (GPs) the freedom of not having to be on call 24 hours.
This study analyses data taken from organisations that supply primary care outside normal GP working hours. These organisations, known as OOH co-ops, use either nurse or doctor triage to decide which type of treatment a patient will receive. An individual who approaches a nurse triaging co-op can receive one of four services involving either a GP or a clinical nurse. A patient who approaches a doctor triaging co-op can receive one of three GP services. The focus of analysis is on factors that determine the choice between these services.
The decision on which service to provide is decided through a conversation between the patient and a triager. The triager acts as a gatekeeper to the type of service the patient receives and hence the triager’s own characteristicsmay affect service provision.Other factors that may affect provision include patient age, sex, complaint, seasonality and severity of case. This analysis aims to analyse the degree to which these factors contribute to service provision, by modelling the decision process using revealed preference multinomial logit models.
Investigating treatment variation is a regular topic in the literature; however, few examples investigate variation in the case of OOH co-ops, even though it has been a concern for many years.[1] This concern has resulted in a call for studies that explore whether consistent care is being distributed by OOH co-ops.[2] This paper falls into this niche. In addition, it is the first study to consider a cross-border treatment variation question for the island of Ireland in the context of any healthcare system. In this paper we think of consistent care as a necessary condition (but not sufficient) for quality in these organisations.
One study of this type relating toOOHco-ops in NI was cross-sectional and therefore could not examine within-co-op variations in treatment type.[3] Its primary aim was to investigate variations in use and equality of access to a doctor for one geographical area in NI. Aside from the NI study, there was one other cross-sectional study that investigated the treatment variation question for an OOH co-op that operated outside of the island of Ireland. This study examined whether the distance of a patient’s residence from the co-op centre affected the probability of their receiving a direct consultation with a GP for an OOH service operating in north west England.[4] In both of these studies no attempt was made to control for variation in the type of complaint a patient presented with. A third study did consider the treatment type variation question across co-ops but was restricted to one disease type – gastroenteritis.[5] In this study of five co-ops operating in ROI, consistent care was distributed to individuals with gastroenteritis. This study was limited in only examining one illness type.
Considering primary care in general, awide range of treatment variation literature exists. Socio-economic status,[6,7] practice characteristics and patient characteristics [8] have all been listed as causes for variation in quality and type of care received. This analysis considers both practice and patient characteristics as factors that may cause variation in the type of service received by OOH services. Socio-economic status was not included due to lack of data. The conclusions from the wider literature show variations in the treatment a patient receives in general practice, over and above their characteristics and illness. This study adds to this body of literature by considering OOH primary care co-ops.
Much of the literature catalogue on treatment variation relates to the US and UK. This work therefore helps to fill this gap. It is seen that this work should interest policy makers – both in NI and ROI, as well as in countries that may be considering the OOH co-op structure – GPs, as well as the management and staff of OOH healthcare facilities.
Background and description of co-op services
In ROI and NI, individuals receive care for an illness from three types of organisations. These are, in-hours GP services, OOH GP services and hospitals. This study considers data fromOOHGP services andOOH co-ops.
Traditionally, the word ‘co-op’ was used to describe a situation where GPs in a similar geographic area came together to provide OOH care. This usually involved each GP being on duty a certain amount of time during evenings or weekends each year, with other GPs covering their patients for OOH care in return. Over time this has grown into a very structured arrangement in ROI and NI, with co-ops having their own management, administrative and nursing staff. In both ROI and NI, co-ops may even encompass several treatment centres as illustrated in Figure 1. This structure still exists in both ROI and NI; however, there has been a move towards ‘buyouts’ by some GPs. This involves GPs substituting themselves with a locumGP for their rostered OOH shifts. In addition, in June 2003 GPs voted throughout the UK to accept a new contract for the delivery of general medical services. This contract was accepted in NI, and under this new contract GP practices are able to opt out of providing OOH care. The responsibility for ensuring such services are provided is with the health and social services boards. Opt outs began from 1 April 2004 but only where an accredited alternative scheme was in place. From 31 December 2004, GPs were no longer personally obliged to provide OOH services, and theoretically it is expected that this may have resulted in increases in the number of locum GPs on duty in NI co-ops (it should be noted that statistical testing does not indicate any structural change over this period). This, however, cannot be observed in the data given that GP identity is confidential. Therefore, the reader may view the co-ops considered here as the traditional co-op structure but with locum GP substitution. This structure is still in place in ROI and NI today.
Although NI and ROI have their own individual health systems, theOOHorganisations themselves are relatively homogenous in structure, opening hours and facilities. In fact, in recent times there has been a call to allow patients to attend an OOH co-op that is across the border of NI and ROI, if it is more convenient to them.9 As yet, it remains the case that a patient’s GP must be an active member of the OOH co-op in order for the patient to be entitled to urgent primary care from these organisations.
There are 12 OOH co-ops operating in ROI. Eight of these co-ops operate from 6 pm to 8 amMonday to Friday. On weekends, the OOH co-op operates a 22- hour shift that starts at 10 am on Saturdays and Sundays and finishes at 8 am the following morning. These co-op treatment centres (see Figure 1) have facilities that are similar to those expected in an inhours GP practice setting. The remaining four OOH co-ops operate from 6 pmto 10 pmMonday to Friday and 10 am to 6 pm Saturday and Sundays. These coops are based in Dublin and operate on a smaller scale. All OOH co-ops operating in ROI were asked to contribute data to this study and eight agreed. Two OOH co-ops were excluded from the analysis because their database definitions were not consistent with the remaining six and also because they did not store the majority of variables necessary for this study. The six co-ops included operate outside Dublin.
It should be noted that since the collection of data for this work, a newOOHco-op initiative has been set up in theNorth Dublin area (this co-op is calledD-Doc) of ROI. This OOH co-op opened its doors on 28 November 2006 and so far has a total of five treatment centres. This initiative is part of a larger plan to extend OOH care to the whole of Dublin.
In NI there are seven OOH co-ops located within four health boards. The northern, western and southern boards each contain one OOH co-op. There are four co-ops in the eastern board, resulting in a total of seven OOH co-ops. The OOH co-ops in NI have identical opening hours and structure to their ROI colleagues who operate outside Dublin. All seven organisations were asked to contribute data and five agreed. The final sample therefore contains 11OOHco-ops, which serve over 50% of the population of the island of Ireland and almost 80% of the geographical area actually covered byOOHco-ops, keeping in mind that Dublin has a very limited OOH service.
In NI and ROI, individuals must seek care in the co-op where their own GP is a member. These organisations can offer some or all of the following services:
a advice via telephone from a nurse
b advice via telephone from a GP
c a consultation with a GP in one of the co-ops’ treatment centres
d a consultation with aGP in the patient’s own home.
Nurse advice is available from co-ops that practise nurse triaging, in this case five out of the six co-ops in the sample. All of the remaining co-ops practise doctor triaging. When patients contact a co-op they are connectedto the triage unit,where an operator takes their details. A triager (a doctor in the case of doctor triaging and a nurse in the case of nurse triaging) then telephones the patient back and discusses the particulars of their complaint, their characteristics and their symptoms, to establish which service best suits the patient’s needs. If a patient is to receive triage advice for their complaint, the triager provides it at this point. For any other service the patient is referred to their nearest centre. The patient is tracked from the point of original contact through to their final diagnosis and treatment.
The resources utilised by the co-op to provide the services increase from (a) to (d) above. That is, a home visit uses more resources than a treatment centre consultation etc. Nurse advice (if it is available) is given to individuals with mild symptoms, or illnesses that are easily recognisable and treatable with over the-counter medicines or home remedies. Nurse advice is also used to provide reassurance. Individuals receive doctor advice for these queries for co-ops that operate doctor triaging. For certain complaints a direct consultation is necessary. The triager ensures the patient receives a treatment centre consultation unless the patient is immobile. A patient is considered immobile if they are too ill or frail to travel, do not have access to transportation, or are physically impaired. In this case a home visit is the service received.
Sample and model
A multinomial logit was used to consider the factors that determine the choice of service to provide. Because nurse and doctor triaging co-ops offer four and three services to patients respectively, simply pooling the data into one model with four services would result in meaningless comparisons. Therefore, nurse advice and doctor advice were pooled, resulting in a three-alternative set. These are therefore, advice, treatment centre consultation and home visit, respectively. Therefore, we consider the case where a triager can decide between giving a patient advice, a treatment consultation and a home visit where this decision is based on patient, call and co-op characteristics. This is given by:
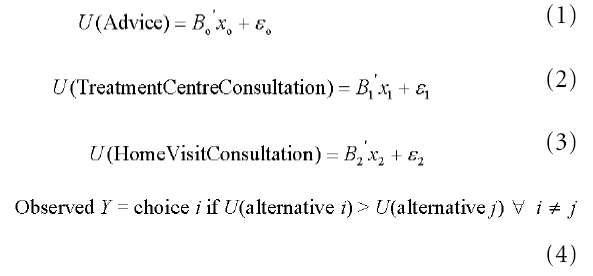
In equations (1) through (3) the utility of each treatment is stated as a function of x and an error component E. In this case are vectors of parameters to be estimated and x is a vector of explanatory variables incorporating patient, call and complaint characteristics as well as seasonality effects and co-op fixed effects. These variables are described in the next section. In equation 4 i and j index the choices 1...3. The probability that i is chosen out of j is:
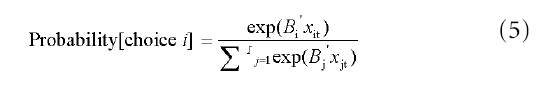
where t = 1 ... n patients, and j indexes the choices 1 ... 3 (because the data are individual patient data clustered within co-ops, a corrected asymptotic covariance matrix is considered).
It was assumed that the triager ensures the patient receives the service that utilises the least amount of co-op resources, subject to maximising the patient’s utility. Therefore, the service provided is based on information supplied to the triager, reflecting the service that gives the patient a greater utility than any of the other services offered without wasting resources. This seems reasonable given that the alternative suggests inadequate care for all patients.
Data and descriptive statistics
The primary data from the OOH services in both NI and ROI were extracted from a database (Adastra). Administrative data are entered into this system which tracks the patient from the time that they contact the co-op until their call is complete. A query was run on this database which retrieved anonymous patient records for the period 1 May 2004 to 30 April 2005. This query allowed the required fields relating to patient case notes to be selected (without any patient identifiers) and downloaded into Excel.
The data used relate to a 5% random sample of patients, which resulted in a sample of 35 523 observations comprising individual first-time visits for a particular complaint. If an observation was chosen that did not receive any of the services offered by the OOH co-op under consideration, this observation was dropped with replacement. These observations related to individuals who were either referred to the emergency department, no shows for consultations, hung up or cancelled their call. There were two reasons for these exclusions: firstly, together they made up less than5%of the entire sample; secondly, in each of these cases the details recorded were incomplete.
The analysis allows for heterogeneity of patient complaint by coding each case with the relevant International Classification of Primary Care (ICPC-2) code. Initially, each case was linked to one of 724 low-level codes; however, including all these effects resulted in the regression collapsing. Therefore, each case was linked to its higher-level category, which described the overall nature of the complaint. It was envisaged that including these fixed effects in the analysis captured some of the heterogeneity across patient complaints. These categories were: (a) General/unspecified; (b): Blood/ blood-forming organs/immune; (c): Digestive; (d) Eye; (e) Ear; (f) Circulatory; (g)Musculoskeletal; (h) Neurological; (i) Psychological; (j) Respiratory; (k) Skin; (l) Endocrine/metabolic/nutritional; (m) Urinary system; (n) Pregnancy; (o) Childbearing; (p) Family planning; (q) Female genital system including breast; (r) Male genital system including breast; (s) Social problems. In addition, two additional codes were created to represent cases that fall outside these categories. Extra code ‘A’ denotes patients who presented for general advice of an unspecified nature or who had a question on medication that they were taking/had yet to take. It was envisaged that individuals who presented under this code were most likely to have received advice. Extra code ‘B’ was used to code individuals who requested a medical test and had no other cause for their call.
Because the ICPC categories were broader than the original codes we considered, it is acknowledged that all case heterogeneity may not have been captured. Therefore, three more indicators were included to allow for severity. These indicated whether the patient had a life-threatening complaint, was in a collapsed condition or had lost body control. For these indicators, it was expected that individuals were most likely to receive a home visit because of the serious nature of their symptoms.
The individual co-op effects considered that the type of service a patient received might vary depending on the co-op they contacted. For example, if triagers allowed their personalities to affect their work thismay have affected the type of service thepatient received. Itwas these variables that allowed us to consider whether quality was consistent across these organisations – at least in terms of the type of treatment received.
The patient characteristics considered related to age, pregnancy status and sex. The predicted effects of age were fuzzy, given that a variety of illnesses vary in severity across age groups. This is adequate however as the only purpose of this variable is to control for heterogeneity. Considering pregnant women, if the nature of the complaint could affect the fetus, they may have received more resource-intensive services. However, this expectation is reversed if this group consults on lower thresholds of illness. For females, while the literature suggests that females receive a higher quantity of primary care,4 evidence suggests that this does not translate into differences in the type of treatment received.2
Over 60% of patients observed who expressed an interest in going to hospital had been advised to do so by their GP if their condition worsened. They may therefore have received advice on how to be admitted to hospital. Alternatively, a consultation may have been a substitute. Patients recently discharged from hospital are likely to be recovering and therefore less mobile. If the individual is very ill, the probability of a home visit is positive, whereas if the patient needs reassurance the individual may receive advice.
Call characteristics related to the time the patient contacted the co-op and the perceived priority of their call. The latter is a clinical indicator, indicating how serious the caller’s complaint is. It is expected that priority individuals would be more likely to receive a home visit or a consultation in a treatment centre depending on their mobility. The time of contact ranged from 0.000 (midnight) to 0.999 (23:59). It was expected that calls received between 12 am and 8 am (red-eye) would be more urgent, assuming that calls during night hours increased with severity of symptoms. Seasonal effects were represented by a set of dummies. Given that many illnesses vary in type and severity over the seasons, the effects were unclear and dependent on the diversity of cases inherent in the data.
The results are shown in Table 1. The coefficients in the individual columns show the effect the independent variables had on the probability of the state, relative to the probability of the reference state. For example, a positive coefficient on a female indicator in the home visit column indicates that a woman had higher odds of receiving a home visit over an advice service (reference state). If in the same example the female coefficient was again positive and higher than the value in the home visit column, this can be interpreted as showing that women had higher odds of getting a treatment centre visit over a home visit and nurse advice. The probabilities of significance of the individual variables are in brackets. Coefficientswith a probability equivalent to 0.05 or greater are insignificant at the 5% level of significance with respect to traditional t testing. The estimated coefficients for the ICPC codes were omitted for brevity. These can be requested from the author.
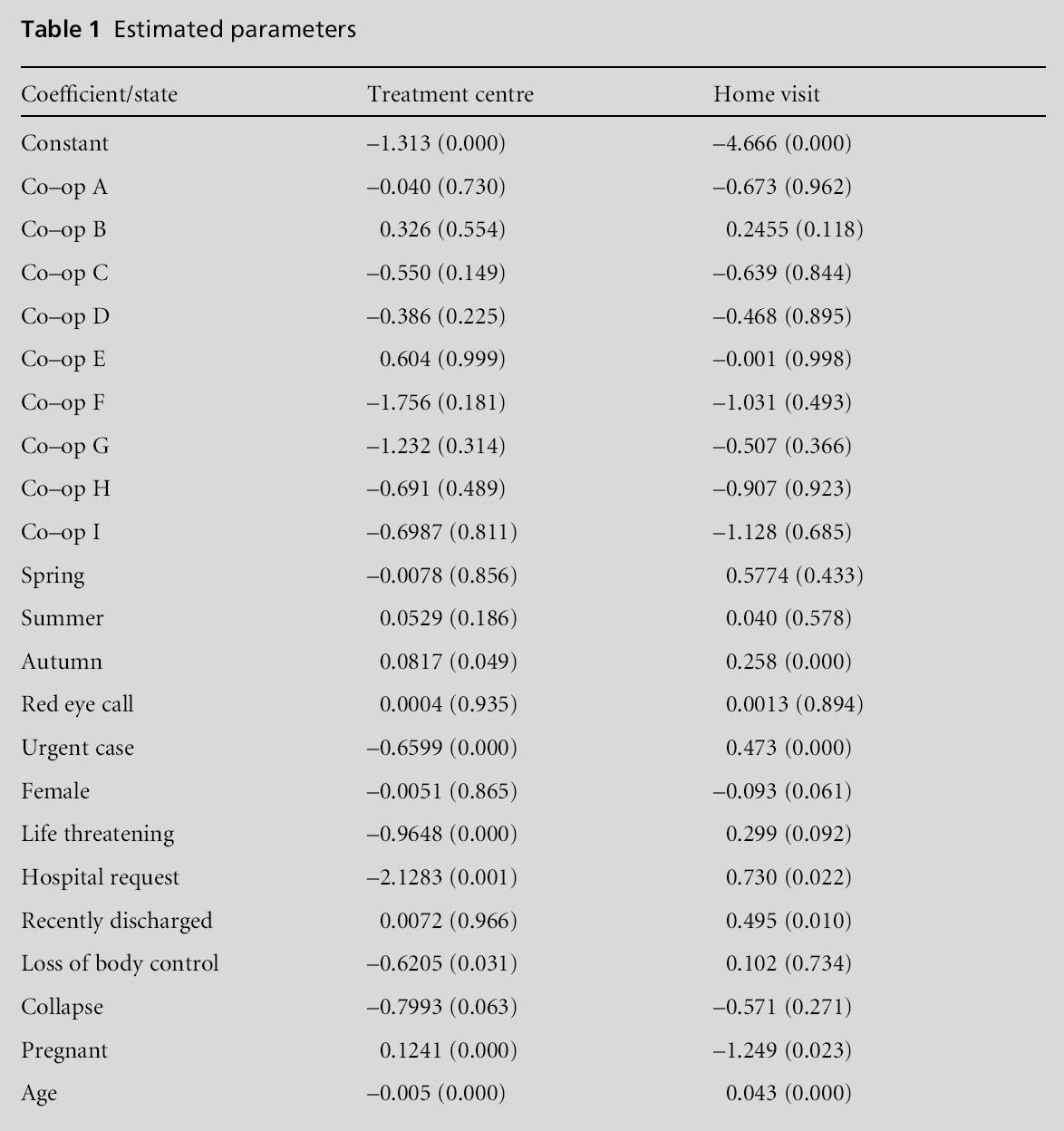
Interestingly, all of the co-op coefficients are insignificant. This suggests co-op fixed effects are not influential on the type of service provided.
All seasonality effects are insignificant with the exception of autumn. In addition the red eye effect is also insignificant. For all of these insignificant coefficients the interpretation is that there are no increased odds of receiving advice over a treatment centre consultation or a home visit.
Priority callers were most likely to receive a home visit. The results indicated minimal sex differences in the type of service received, with women having the same probability as men of receiving an advice service.
For individuals recently discharged from hospital, there was a strong positive coefficient attached to the probability of receiving a home visit, and a strong negative coefficient attached to the probability of receiving a treatment centre visit over any advice service.
For individuals who requested to go to hospital, the results suggest that these groups were more likely to receive a home visit.
For individuals who presented with a life-threatening illness, the negative coefficients attached to the probabilities of treatment centre visits for all three variables (albeit the coefficient on collapse is insignificant at the 5% level) indicate that the odds were negative of them receiving this service over advice. Conversely, there was a positive probability effect associated with receiving a home visit for individuals presenting with a life-threatening illness or loss of body control. This indicates that the odds were highest that they would receive a home visit.
Pregnant women were most likely to receive a treatment centre consultation. This is illustrated by the positive coefficient in the treatment centre column. The probabilities attached to the age variable are very small and significant, with treatment centre visits being the marginally preferred service.
The main aim of this study was to examine the consistency in the type of treatment received by patients from OOH services that operate in Ireland (NI and ROI). The results showed that all of the co-op fixed effects were insignificant, implying that the type of service provided was determined by factors external to the co-op. With respect to quality, this finding is good news for the growing number of countries in Europe who are considering co-ops as a feasible arrangement for OOH primary care, as it suggests consistent quality of care in terms of treatment type received. It should be noted that while this indicated consistency in the type of service received, it did not mean that the standard of treatment within services was consistent. For example, it is not possible to determine if individuals received the same quality of care within treatment centre consultations. Therefore, wemay think of service type provision as a necessary but not sufficient requirement for quality.
Most of the remaining results are consistent with expectations with the exception of the red-eye coefficient. This may be explained by certain individuals contacting the OOH co-op at lower thresholds of illness regardless of time, and by the increase in the number of individuals who work unsociable hours.
Overall, patient characteristics and perceived priority were found to significantly impact the type of service a patient received upon presenting to an OOH co-op. This work provides evidence of the reasons for treatment variation in the type of treatment received across OOH organisations operating in Ireland. The next step is to gather evidence on causes for variation in quality of care across types of treatment and prescribing patterns in these organisations.
Not commissioned; externally peer reviewed.
None.