- (2015) Volume 16, Issue 2
Tulay Kus1*, Mehmet Emin Kalender1, Gokmen Aktas1, Ali Suner2 and Celaletdin Camci1
1Division of Oncology, Department of Internal Medicine, University of Gaziantep, Gaziantep, Turkey
2Division of Oncology, Department of Internal Medicine, University of Ad'yaman, Gaziantep, Turkey
Received November 20th, 2014 – Accepted January 30th, 2015
Context Cancer is a prothrombotic state and anticancer therapies are often complicated by vascular events. The risk of developing thromboembolic events is substantially increased in patients with pancreatic cancer. One possible presentation of vascular events in pancreatic cancer is disseminated intravascular coagulation (DIC). Case report In our case a patient with a diagnosis of pancreatic cancer initially presented with thrombosis and received low molecular weight heparin (LMWH) in addition to standard chemotherapy regimen. He was thought to have DIC by assessment of clinical and laboratory findings. Conclusion Clinically, thrombosis was first located in the left femoral vein and encountered at right femoral artery after three weeks. This pattern was an unusual presentation of DIC. Subclinical DIC is common in patients presenting with pancreatic cancer and is considered a ‘poor’ prognostic factor. Acute DIC, on the other hand is a potentiallymortal condition.
Adenocarcinoma; Disseminated Intravascular Coagulation; Mesenteric Ischemia
Pancreatic cancer is the fourth most common cause of cancer related death in the United States [1]. Pancreatic adenocarcinoma is among the most common malignancies associated with thromboembolic events. A retrospective analysis of 1915 patients diagnosed with pancreatic cancer showed that thromboembolic events had been detected in 36% of patients. 78.3% of patients with thrombosis had stage IV disease. 95.4% of the events were venous and 4.4% arterial. Concomitant arterial and venous thromboembolism has a very unusual rate of 0.1% [2, 3]. The most common vascular events are deep venous thrombosis (DVT) and pulmonary embolism. Arterial events like stroke and myocardial infarction are less common.
Disseminated intravascular coagulation (DIC) is a procoagulant condition that is well defined in autopsy cases [4]. In an analysis, 45% of established DIC cases presented with cancer. This co-occurrence is more frequent in hematologic malignancies and respectively in gastric cancer, lung cancer and pancreatic cancer. DIC is a progress consisting of thrombosis and bleeding due to consumption of coagulation factors and has six diagnostic criteria’s according to the International Society on Thrombosis and Haemostasis (ISTH): underlying disease, clinical symptoms, platelet counts, fibrin-related marker, fibrinogen level (g/L) and prolonged prothrombin time (PT) [5] (Table 1).
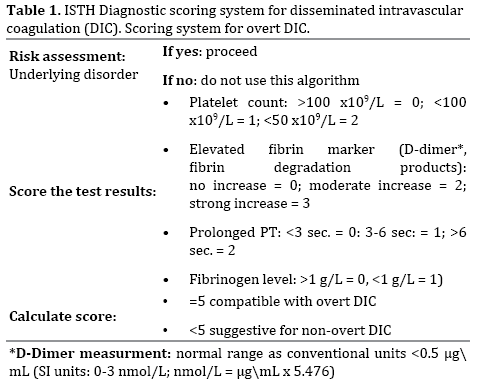
A sixty-eight-year-old male patient with a history of smoking (40 packs/year) without known cardiovascular disease was admitted to hospital. He was complaining of fatigue, dyspepsia, epigastric pain, weight loss of 10 kg over the previous month and also swelling, pain and hyperemia in left leg. Acute thrombosis was detected in the left main, deep and superficial femoral veins and popliteal vein at venous Doppler ultrasound. An upper gastroendoscopy revealed pangastritis and external compression of antrum. Multiple solid lesions greater than 1 cm in size were detected in abdominal ultrasonography and considered as prospective metastatic lesions. Abdominal computed tomography demonstrated a 4.5×2.5 cm mass in the tail of pancreas (Figure 1). Laboratory investigations revealed elevated CEA (5 ng/mL), CA19-9 (>1000 U/mL) and protrombin time (16 sec) levels with mild thrombocytopenia (130000 109/L) and an increased D-dimer (4 μg/mL (conventional units)). Percutaneous liver biopsy was performed on the lesion. Full dose LMWH treatment was initiated immediately following liver biopsy. Liver histology confirmed adenocarcinoma with morphology consistent with pancreatic primary. Stage IV pancreatic cancer with thrombotic complications was suggested. Chemotherapy was initiated as gemcitabine 1000 mg/m2 day 1 and day 8, carboplatin AUC5 day 1 per three weeks. Seven days after the initiation of chemotherapy, the patient presented with hematemesis, thrombocytopenia (43000/μL) and a prolonged PT (16 sec) and he was hospitalized. Thrombocytopenia was initially considered to be secondary to chemotherapy. On physical examination, coolness, pallor and decreased pulse in right lower extremity were detected and arterial and venous Doppler ultrasonography was performed on both legs (Figures 2 and 3). Subacute thrombosis was detected in the left main, superficial, profound femoral veins and popliteal vein and thrombi causing obstruction of the right main femoral, popliteal and posterior tibial arteries. LMWH could not be given because of hematemesis and thrombocytopenia. Surgical intervention for arterial thrombi was not considered due to rapid deterioration of the patient's status. Thrombocytopenia got worse and the patient received thrombocyte concentrate and plasma. The patient's orientation in time and space broke down during the follow-up. Ten days after hospitalisation, thrombocytopenia worsened, PT got prolonged, fibrinogen levels increased to 310 g/L and D-dimer was also elevated (15 μg/mL). Hepatic and renal failure developed. Peripheral blood smear revealed findings compatible with microangiopathic hemolytic anemia (schistocytes). Evaluation of the patient according to ISTH criteria suggested overt DIC with a score of 8. Differential diagnoses included liver failure secondary to metastases, other microangiopathic syndromes, anti-phospholipid syndrome, vitamin K deficiency and these were excluded according to clinical and laboratory findings. The patient passed away 2 months after the diagnosis.
Thrombosis is the second-leading cause of death in patients with cancer [6]. Cancer patients with vascular thromboembolism (VTE) have a doubled or greater risk in mortality compared with cancer patients without VTE [7]. The pathogenesis of the prothrombotic state in cancer is very complex. Primarily, procoagulant molecules are produced by tumor cells and fibrinolytic activity is suppressed. At the same time the genetic mechanisms such as oncogene activation (RAS, MET) and tumor suppressor gene inactivation (P53, PTEN) are responsible for malignant transformation which directly induce the expression of genes regulating hemostasis [8].
Other factors such as antineoplastic therapy, surgery and vascular access ways also contribute to the prothrombotic state. The most important procoagulant expressed by tumor cells is tissue factor (TF). TF is present on neoplastic cells as well as endothelial cells in a variety of cancers. TF expression occurs early in neoplastic transformation and is driven by oncogenic mutation in KRAS and P53 genes [9] that is associated with increased angiogenesis, tumor invasiveness and worse prognosis in cancer [10].
The spectrum of presentation of patients with thrombosis varies widely from abnormal coagulation tests and the absence of thrombotic symptoms to massive thromboembolism. Subclinical abnormality in the hemostatic system can be observed in averagely 90% of cancer patients. Clinical presentation includes migratory superficial thrombophlebitis (Trousseau's syndrome), DVT and other sites of venous thrombosis, marantic endocarditis, DIC, thrombotic microangiopathy and arterial thrombosis [11].
DIC is a coagulopathy which includes fibrinolytic syndrome and a systemic process causing both thrombosis and hemorrhage. It is initiated by conditions such as sepsis, trauma, ischemia, excessive metabolic stress, heat, chemicals and tumors. DIC always occurs secondarily and increases the risk of mortality associated with the primary disease. Fibrin formation in the circulation, fibrinolysis, depletion of clotting factors, and low platelet counts occur as a result of endothelial damage exposure which leads to procoagulants such as tissue factor [12].
Clinical presentation of DIC depends on the balance between activation of thrombin and secondary fibrinolysis. There are four clinical presentations of DIC. The first one is the asymptomatic form and the second includes abnormality of laboratory without clinical symptoms such as thrombosis and hemorrhage. The third presentation is thrombosis, hemorrhage and purpura fulminans and the fourth one is only purpura fulminans. The first two presentations, usually observed in cancer patients are called or compensated DIC. Tissue factor is released intermittently at the period. Therefore, liver and bone marrow can easily compensate. When compensation fails; petechiae, purpura, thrombosis develops causing especially liver, kidney and other organ failures due to microangiopathic hemolytic anemia. Deep vein thrombosis of extremities, arterial thrombotic events such as digital ischemia, renal infarction, cerebrovascular event and marantic endocarditis can be encountered in patients secondary to solid tumors [13]. DIC is a secondary condition depending on the underlying disease. Treatment should primarily focus on addressing the underlying disorder. There is no proven treatment, but heparin and derivatives can be used to prevent thrombosis, and plasma and thrombocyte concentrates can be used to prevent bleeding [12].
In our case, the patient was diagnosed with pancreatic cancer while differential diagnostic investigations for DVT were ongoing. Pancreatic adenocarcinoma is commonly associated with DIC. This case is an unusual presentation of DIC which exhibits atypical peripheric extremity findings like arterial gangrene on the right leg and venous thrombosis on the left leg. According to two large, prospective randomized clinical trials (CLOT and CONCO 004), the risk of developing symptomatic venous thromboembolism was lower for patients on LMWH treatment. One meta-analysis showed that use of LMWH provides strong prevention of thrombosis among patients with lung and pancreatic cancer [14]. However, despite primary and prophylactic treatment with LMWH, the underlying procoagulative state may persist and decompensated DIC may develop especially in patient with pancreatic cancer.
Authors declare to have no conflict of interest.