Case Report - (2021) Volume 5, Issue 4
Biliary Sodium Depletion: A Rare Cause of Hyponatremia and Renal Failure
Lemfadli Yassine1*,
Jallouli Abderrahmane1,
Ait Errami Adil1,
Samlani Zouhour1 and
KratiKhadija1
1Department of Gastroenterology, Mohammed VI University Hospital, Marrakech, Morocco
*Correspondence:
Lemfadli Yassine, Department of Gastroenterology,
Mohammed VI University Hospital, Marrakech,
Morocco,
Email:
Received: 16-Dec-2021
Published:
06-Jan-2022
Abstract
External biliary drainage is a necessary procedure in some situations, particularly in tumour obstructions of the bile ducts. We report the case of a 51-year-old man with hyponatremia and functional renal failure after high- volume biliary excretion following external percutaneous transhepatic biliary drainage for an obstructive Klatskin tumor. Our case shows that internal drainage should be preferred to external drainage which is a source of hydro electrolyte and circulatory complications that can be life- threatening.
Keywords
External biliary drainage; Hyponatremia; Renal failure; Klatskin tumor; Jaundice
Introduction
The majority of biliary obstructions of tumor origin are unresectable at the moment of diagnosis, thus requiring biliary drainage for palliative purposes; at best internal drainage. Otherwise, external drainage may be necessary [1]. During external biliary drainage, the amount of bile fluid drained daily varies between 200 to 1600 mL. However, higher volumes have been described in some cases in the literature [2].
We report the case of a patient who underwent external biliary drainage for a Klatskin tumor, with a high biliary drainage rate, leading to hyponatremia and functional renal failure.
Case Presentation
A 51-year-old man was admitted for frank cholestatic cutaneous-mucous jaundice (dark urine, discolored stools and generalized pruritus) which had progressed for 3 months. He also had mild to moderate epigastralgia with no aggravating or relieving factors. He reported 16 kg weight loss in 3 months. He had no other associated symptoms. He had no specific medical history and was not taking any treatment.
The biological assessment showed biological cholestasis: hyperbilirubinemia at 276 mg/L predominantly conjugated (230 mg/L), Alkaline Phosphatases (ALP) elevated to 1172 U/L (9.8 times the upper reference value) as well as an increase Gamma- glutamyl Transferases (GGT) at 2528 U/L (35 times the upper reference value), associated with minimal cytolysis: ASAT at 107 U/L (2.1 times the upper reference value) and ALAT at 115 U/L (2.8 times the upper reference value). The rest of the laboratory tests showed hemoglobin at 13.4 g/dl, leukocytes at 6240/μl, a slightly elevated C-Reactive Protein (CRP) (16 mg/L), a normal level of prothrombin (78.2%), serum sodium was 136 mmol/L and serum potassium 4.2 mmol/L. Creatinine was 8 mg/L and urea 0.5 g/L.
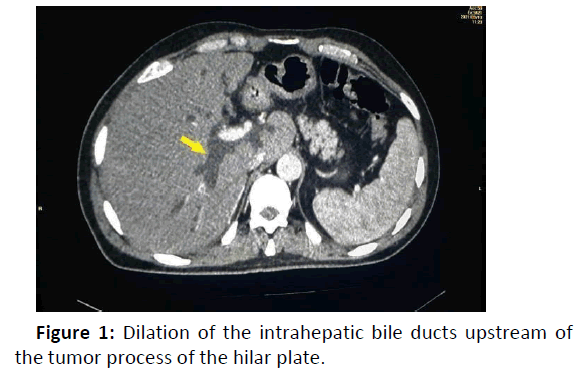
An abdominal ultrasound performed showed dilation of the intrahepatic bile ducts, most likely by compression in the hepatic hilum. A complement by MRCP (Magnetic Resonance Cholangiopancreatography) revealed a significant dilation of the whole of the intrahepatic biliary arborization contrasting with a normal aspect of the main bile duct. This was caused by a tumor process from the hilar plate extending to the biliary convergence, without obstruction of the right and left main bile ducts. The description was in favor of a stage 2 Klatskin tumor according to the Bismuth classification.
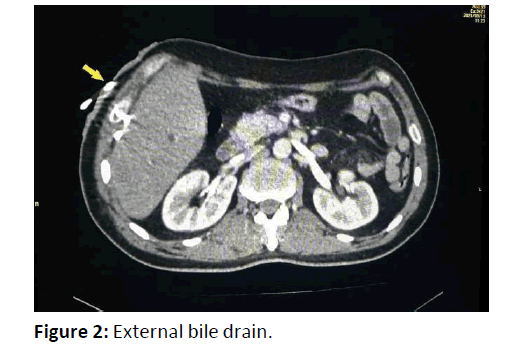
The patient underwent radiological external biliary drainage. The procedure consisted of performing a catheterization of a peripheral bile duct, the opacification of which showed tight stenosis of the hilar convergence. It was not possible to pass the stenosis of the main bile duct using catheters, which led the operator to insert an 8 French external drain (Figures 1 and 2).
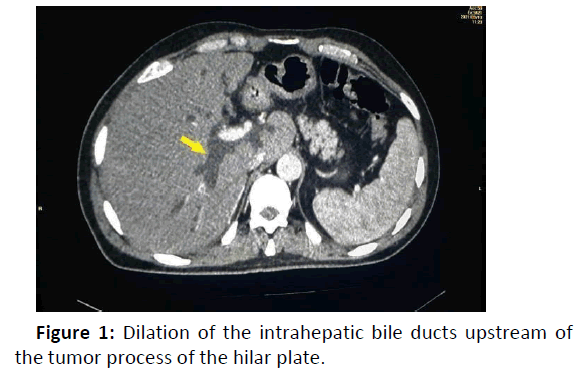
Figure 1: Dilation of the intrahepatic bile ducts upstream of the tumor process of the hilar plate.
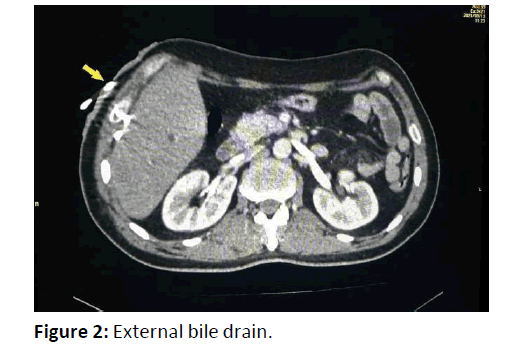
Figure 2: External bile drain.
The evolution was marked by a decrease in the intensity of the jaundice and pruritus. The stools regained their normal color and the urine was still dark. The drain was functional bringing back 2 to 2.5 liters of bile per day. The patient had no other fluid losses, notably no vomiting or diarrhea.
A biological assessment performed three days after the installation of the bile duct showed a regression of the biological cholestasis, with the appearance of a hyponatremia at 124 mmol/L which is hypo-osmolar (254 mosmol/Kg) as well as a renal insufficiency (urea at 1.6 g/L and creatinine at 22.1 mg/L).
The patient was initially placed on parenteral supplementation with sodium chloride (4 grams/day intravenously). The hyponatremia was persistent despite correction.
A week later, the patient reports a spontaneous fall of the biliary drainage catheter. A remarkable rise in serum sodium and a correction of renal failure were noted a few days after this incident (serum sodium increased to 139 mmol/L. Urea and creatinine became normal (0.44 g/L and 9.7 mg/L respectively).
This hyponatremia was therefore secondary to a significant loss of sodium through the external biliary drainage, and the renal failure was of functional origin.
The patient subsequently underwent Endoscopic Retrograde Cholangiopancreatography (ERCP) with biliary brushing, the histological study of which was in favor of cholangiocarcinoma. The extension assessment did not reveal any secondary locations. The patient's file was presented to a multidisciplinary consultation meeting for surgical resection.
Results and Discussion
Daily biliary production is normally between 500 and 1000 mL [3]. In certain situations, this production can increase up to 8 liters per day, especially in the case of biliary fistulas or after biliary drainage, exposing the patient to the risk of hydroelectrolytic disorders (hyponatremia, functional renal insufficiency, decrease bicarbonate levelsin serum, orthostatic hypotension) [4-6]. In a series of seven patients, biliary losses ranging from 1.3 to 7.7 L/day occurred immediately after external biliary drainage and lasted for 2 to 14 days [7]. In another report of two patients, biliary losses of 17 L over 4 days in the 1st patient and 20.8 L over 7 days in the 2nd patient were responsible for orthostatic hypotension, hyponatremia and functional renal failure [8].
The average sodium concentration in the bile is around 145 mmol/L (usually varies between 122 and 164 mmol/L) [9]. In our case, the biliary drain brought back a daily volume of about 2 liters each day, which represents about 290 mmol per day, which is equivalent to a loss of about 6 to 7 g of sodium per day, explaining the persistence of hyponatremia despite insufficient sodium supplementation (4 g/day).
Some situations favor the development of hyponatremia secondary to biliary drainage, including pre-existing renal pathology, use of diuretics, hepatic cirrhosis, adrenal insufficiency, and a low sodium diet [9].
Although the mechanism by which this occurs in some cases is not clear, the development of acute renal failure complicating external biliary drainage has been described in the literature [10,11]. It seems that hydrosodic depletion through biliary drainage leads to a loss of ionic reserves and consequently to circulatory insufficiency. In the context of metabolic acidosis, this will lead to a decrease in renal perfusion, parenchymal hypoxia and an alteration in tubular function in the absence of immediate and appropriate therapeutic management.
Therapeutic management of these complications requires filling with isotonic fluids containing sodium, chloride, lactate, bicarbonate, and potassium in patients with hyponatremia, and should be tailored to the volume of bile fluid and serum electrolyte levels [10]. On the other hand, good filling with octreotides and renal support with hemodialysis, have been found to be effective in the management of renal failure complicating external biliary drainage [2].
External biliary drainage in some conditions should be avoided by opting for internal biliary drainage, which has more advantages: More access to the biliary tree and no external catheter [12]. Internal drainage is preferred after certain procedures, such as hepatectomy, in which external drainage suppresses liver regeneration under certain conditions [13].
Conclusion
External biliary drainage can lead to major hydro electrolytic complications, especially during high biliary flows, due to the loss of large quantities of water and solutes through the biliary drain. This situation can lead to circulatory insufficiency responsible for functional renal failure.
The interest of this observation is to search for these complications in patients having benefited from an external biliary drainage, by a clinical and biological monitoring of the signs of hyponatremia, hypovolemia and renal failure.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author’s Contributions
All authors participated in the conception, drafting the work, critically revised the manuscript, approved the final version to be published, and agree to be accountable for all aspects of the work.
REFERENCES
- Pu LZ, Singh R, Loong CK, de Moura EG (2016) Malignant biliary obstruction: Evidence for best practice. Gastroenterol Res Pract 2016: 1-7.
- Jayarajah U, Basnayake O, Wijerathne PK, Sivaganesh S (2019) Acute kidney injury due to high-output external biliary drainage in a patient with malignant obstructive jaundice: A case report. J Med Case Rep 13: 1-3.
- Whipple GH (1922) The origin and significance of the constituents of the bile. Physiological Reviews 2: 440-459.
- Knochel JP, Cooper EB, Barry KG (1962) External biliary fistula: A study of electrolyte derangements and secondary cardiovascular and renal abnormalities. Surgery 51: 746-754.
- Lenthall J, Reynolds TB, Donovan AJ (1970) Excessive output of bile in chronic hepatic disease. Surg Gynecol Obstet 130: 243-253.
- Dumont AE (1982) Significance of excess drainage of bile in patients with chronic hepatic disease. Surg Gynecol Obstet 154: 209-213.
- Taber DS, Stroehlein JR, Zornoza J (1982) Work in progress: Hypotension and high-volume biliary excretion following external percutaneous transhepatic biliary drainage. Radiol 145: 639-640.
- Sandborn WJ, Gross Jr JB, Larson DE, Phillips JK, Lindor KD (1993) High-volume postobstructive choleresis after transhepatic external biliary drainage resolves with conversion to internal drainage. Journal of Clinical Gastroenterology 17: 42-45.
- Furey AT (1966) Hyponatremia after choledochostomy and T tube drainage. Am J Surg 112: 850-855.
- Kichloo A, Zain EA, Khan MZ, Wani F, Singh J (2019) Severe persistent hyponatremia: A rare presentation of biliary fluid loss. J Investig Med High Impact Case Rep 7: 1-3.
- Basten A, Opit LJ (1966) Severe sodium depletion with renal failure following common bile duct drainage. ANZ J Surg 36: 105-110.
- Nussbaum JS, Kumta NA (2019) Endoscopic ultrasound-guided biliary drainage. Gastrointest Endosc Clin 29: 277-291.
- Saiki S, Chijiiwa K, Komura M, Yamaguchi K, Kuroki S, et al. (1999) Preoperative internal biliary drainage is superior to external biliary drainage in liver regeneration and function after hepatectomy in obstructive jaundiced rats. Ann Surg 230: 655.
Citation: Yassine L, Abderrahmane J, Adil AE, Sofia O, Zouhour S, et al. (2022) Biliary Sodium Depletion: A Rare Cause of Hyponatremia and Renal Failure. J Clin Gastroenterol Hepatol Vol.5 No.4:1
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.