Case Report - (2021) Volume 6, Issue 7
Received: 03-Dec-2021 Published: 23-Dec-2021
A 32 years old man who is known to have Klippel-Trenaunay syndrome was involved in a “head-on” Motor Vehicle Collision (MVC) as a restrained driver. He was managed in a level one trauma center where trauma protocol CT angiography was done and showed an active bleeding from an unidentified vessel in the pelvis on CT angiogram with a possible bowel injury. He underwent trauma laparotomy and was found to have bleeding from the left testicular artery on an undiagnosed undescended intra-abdominal testis. Orchidotectomy was done and the final pathology showed normal testicular tissue without malignant transformation. The patient recovered well from his surgery and had no further complications.
Klippel-Trenaunay Syndrome (KTS) is a rare disease, characterized by capillary and venous malformations and soft tissue or bone hypertrophy with overgrowth of the affected extremity [1]. It may also have some genitourinary manifestation. We report here a case of a blunt abdominal trauma in an adult with KTS resulting in intra-abdominal bleeding which was found to be secondary to an undiagnosed intra-abdominal testis. The trauma investigation led to the diagnosis of the undescended testis which was managed with Orchidotectomy. The final pathology showed no malignant transformation. The case highlights the unusual cause of bleeding from blunt abdominal trauma and the incidental finding and management of intra-abdominal testis in a syndromic adult patient which should help decrease his future risk of developing malignancy in that organ.
A 32 years old man who is a known case of Klippel-Trenaunay syndrome was involved in a “head-on” Motor Vehicle Collision (MVC) as a restrained driver. He was brought to the emergency department by the Emergency (EMS) and managed in accordance with trauma protocol.
On Primary survey, He was breathing normally with bilateral equal air entry and normal oxygen saturation on room air. Blood pressure was 124/70 mmHg, heart rate of 96 per minute. His Glasgow Coma Scale (GCS) was 15 and he was kept on C-collar. On exposure, he had seat belt sign across the chest and abrasion in the left groin area. On a secondary survey, his abdomen was tens and tender and there was a port-wine stain over the left gluteal area and varicosities in the left scrotum.
Investigations if relevant
His Chest X ray and Pelvic X ray showed no major abnormalities.
His blood work was within normal values except for a hemoglobin of 5.7 g/dL (the patient is known case of chronic anemia with close follow up with hematology team and the latest recorded hemoglobin one month prior to the trauma was 6.2 g/dl). After the initial resuscitation and assessment he reminds hemodynamic normal and therefore he was sent for Trauma protocol Computer Tomography (CT).
The chest CT scan showed a fracture in the anterior part of the second rib and sternal fracture. There was minimal ground glass opacity in the right middle lobe, and a right pleural effusion. The abdominal CT scan, revealed a large hemangioma with phlebolith in the anterior pelvis with multiple enhancing veins. There was large left gluteal low flow vascular malformation with enhancing veins. The recto-sigmoid area showed mural wall thickening and edema likely due to venous congestion and hypertension with free fluid in the abdomen and pelvis. There was no solid organ injury and no pelvic fractures.
CT angiography revealed a focal area of contrast extravasation in the left iliac fossa from an unidentified vessel [Figure 1A]. The venous phase abdomen CT showed an increased size of the contrast extravasation in the left iliac fossa with free fluid [Figure 1B,2]. There was a soft tissue mass between the urinary bladder and the sigmoid colon with multiple mural calcifications suggestive of phleboliths in an intra-mural hemangioma together with diffuse thickening of the rectum and distal sigmoid colon consistent with soft tissue hemangioma [Figure2].There was a diffuse subcutaneous heterogeneous soft tissue density at the left gluteal region with dilated veins consistent with subcutaneous hemangioma [Figure 3]. The left iliac veins are dilated compared to the right side due to increased venous flow from hemangiomas [Figure 4,5].

Figure 2:Coronal reformat of the venous phase abdomen CT shows the focal area of contrast extravasation (short arrow) and pelvis free fluid (long arrow). There is soft tissue mass between the urinary bladder and the sigmoid colon with multiple phleboliths consistent with soft tissue hemangioma (asterix). There is diffuse thickening of the rectum and distal sigmoid colon (arrow head).
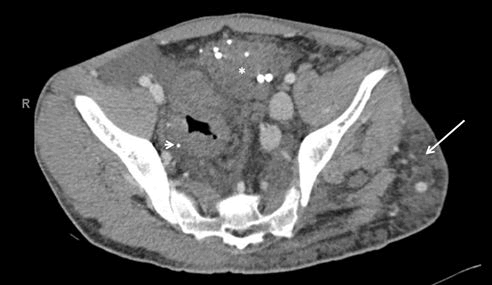
Figure 3:Pelvic hemangioma anterior to the sigmoid colon (asterix). Diffuse thickening of the rectum and sigmoid colon with few mural calcifications suggestive of phleboliths in an intra-mural hemangioma (arrowhead). Diffuse subcutaneous heterogeneous soft tissue density at the left gluteal region with dilated veins consistent with subcutaneous hemangioma (arrow). The left iliac veins are dilated compared to the right side due to increased venous flow from hemangiomas.
Differential diagnosis if relevant
The deferential diagnosis at this point was intra-abdominal bleeding secondary to pelvic vascular bleeding or bleeding from the vascular malformation over the sigmoid colon associated with his syndrome. Sigmoid injury couldn’t be ruled out also. All other major vessels like common iliac and external/ internal iliac were traced and seen in the scan without injuries therefore the specific vascular structure that was bleeding couldn’t be identified/named in that anatomical location.
Treatment if relevant
Based on these findings the patient was taken to the Operating Theater (OR) for exploration and assessment of the bleeding structure and assessment for concurrent bowel injury. The abdomen was entered through a midline laparotomy incision and there was moderate amount of blood. All four quadrants of the abdomen were packed and 500 cc of blood was aspirated. All quadrants were then examined carefully, and the bleeding source was found in the left lower quadrant. The sigmoid was occupying the LLQ and it was covered with a network of dilated veins of varying size on its entire length (a malformation which is part of his disease) with a contained hematoma on the upper aspect of the sigmoid.[Fig4] Although some of these veins were oozing, they did not account for the blood seen in the abdomen. The sigmoid itself was viable without any perforation. On further examination we identified an arterial bleeding form a tubular structure running along the external iliac artery with a round grayish structure at the end of it lying below the sigmoid colon. The left and right ureters and the major vascular structures were identified and isolated [Fig5]. The location and appearance of the bleeding structure was suggestive to be an undiagnosed undescended intra-abdominal testis and the bleeding vessel was presumed to be a testicular artery. In order to control the bleeding the vessel was ligated and the structure was resected as it lost its blood supply. The rest of the trauma laparotomy was carried through as per protocol and no further injury was found.
The histopathological examination of the resected specimen showed testicular tissue composed of variably sized seminephrous tubule lined by Sertoli cells some of which exhibit deeply eosinophilic granules and all tubules show thick basement membrane and peritubular fibrosis.No spermatogenesis was seen. The interstitium was oedematous and shows florid Leydig cell hyperplasia with occasional small nodule formation. No intratubular germ cell neoplasia is seen. The surrounding tunica was thickened and showed a focus of fibrin deposition mixed with acute inflammatory cells compatible with the history of trauma.
The finding of this undescended testis as a source of his bleeding was surprising as there was no pre-operative suspicion of an undescended testis especially an intra-abdominal undescended testis.
Outcome and follow-up
The patient was discharged home in stable condition, and he was seen again four weeks later in the outpatient clinic where he has had a full and satisfactory recovery.
Blunt abdominal trauma is a common cause for hospital admission worldwide as it occur in 31% patients of polytrauma and it is commonly secondary to Motor Vehicle Crash (MVC) [2]. Blunt abdominal injury can result in bleeding that could be intra peritoneal (13 from liver and 16% from spleen), pelvic (28%) or retroperitoneal [2].
The trauma management protocols include a primary survey aimed to assessing and stabilizing the hemodynamics of the patient followed by chest and pelvic X ray, blood investigation alongside initial resuscitation with the appropriate products. The secondary survey focuses in assessing the site and severity of injuries followed by the definitive imaging and management.
In hemodynamically unstable patients, Extended Focused Assessment with Sonography for Trauma (EFAST)) is usually used to assess the presence of intra-abdominal source of bleeding. However, there is a high rate of false negative results. The destination of the patient will depend on the condition of the patient and available resources of the institute. Traditionally these patients would require surgery however with recent advances in endovascular techniques, there is an increasing role for it in the management of traumatic hemorrhage [3]. Angioembolization is over 90 % effective in controlling hemorrhage in the abdomen and pelvis from both blunt and penetrating trauma [4]. It is most effective in managing bleeding form the pelvis, the liver, the spleen and the kidneys. In patients with suspected hollow viscus injuries or combined injury, surgery is still the most appropriate intervention.
In stable patients, a full radiological assessment can help to determine the grade of injury and determine the next step in management. A typical blunt abdominal CT protocol includes portal venous phase images and selective acquisition of delayed and/or arterial phase images (CT angiograms)[5]. Free fluid is a common finding in the trauma CT and it could be secondary to bleeding (hemoperitoneum) or hollow viscus injuries. The management of liver and spleen injuries is dependent on the grade of injury and co-existence of other injuries. The American Association for the Surgery of Trauma (AAST) has developed a CT based scale for splenic and liver injury which could help to guide the management plan. The rate of bleeding and the presence of active extravasation have a more direct effect on patient care decisions [5]. Other possible but very uncommon sources of bleeding is the major vascular structures like the aorta, inferior vena cava, renal vessels, celiac axis, superior mesenteric vessels, lumbar vessels, and iliac vessels. There were no case reports of bleeding form the testicular artery from an undiagnosed intra-abdominal testis like our patient. The management of any bleeding form a vascular structure is either repair or ligation which depends on the size of vessel, the type of injury and the patient’s condition. In our case the bleeding was isolated form one artery feeding the undescended testis. Ligation of the vessel and removing the testis had the benefit of controlling the acute bleeding and decreasing the future risk of this testis.
The patient is known to have Klippel-Trenaunay Syndrome (KTS) which is a rare disease, characterized by capillary and venous malformations and soft tissue or bone hypertrophy with overgrowth of the affected extremity [1]. It may occasionally affect the upper extremity or both legs. The disorder has three characteristic features: a port-wine stain, abnormal overgrowth of soft tissues and bones, and venous malformations. Vascular malformations include varicose veins, Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) [6]. Vascular complications may include, thromboembolism, bleeding and venous insufficiency. Treatment is mainly supportive and includes management of complications [1]. KTS is also known to have some genitourinary manifestation including cutaneous genital abnormalities, and visceral genitourinary involvement [7]. A Brazilian team publish their experience with urological manifestation of KTS patients. They managed 7 KTS patients with urological problems, out of which 3 presented with genital deformities, 2 with hematuria, 2 with urethrorragia one of which associated with cryptorchidism and phimosis. Three patients had an association of pelvic and genital malformations, including 2 patients with hematuria due to vesical lesions and 1 patient with left ureterohydronephrosis due to a pelvic mass. Two patients had urethral lesions [8]. In the general population the Incidence of undescended testis varies between 1.0% and 4.6% in full-term neonates, with rates as high as 45% in preterm neonates [9]. The testis could be palpable (inguinal or retracted) or not palpable (abdominal, ectopic etc.). The commonest complications include infertility and malignancy. Although boys with one undescended testis have a lower fertility rate, they have a similar paternity rate to those with bilateral descended testes. Boys with bilateral undescended testes suffer both lower fertility and paternity rates.[9] The management is usually orchidopexy by the age of 18 months at the latest, to decrease the possibility of fertility issues and cancer risk. In our patient, he was never diagnosed with undescended testis and he did father two children. The final pathology did not reveal malignant transformation in the testis despite lack of early intervention. His overall recovery was satisfactory from both the trauma prospective and the undescended testis point of view.
As it was specified earlier new developments in interventional radiology have increased the use of non-operative management in bleeding form blunt abdominal injury especially pelvic injury and solid organ injuries. In this case the CT finding was of an active extravasation of contrast indicating a vascular injury in an unidentified vessel in those anatomical locations, on a background of a syndrome that has multiple vascular malformations. The intra operative finding and intervention was probably beneficial to the patient in the short course of the trauma but more importantly it had the added benefit of decreasing potential future risk of cancer.
Learning points/take home messages 3-5 bullet points
This is a required field
Klippel-Trenaunay syndrome has multiple urological manifestations and they should be evaluated in any diagnosed patients to eliminate future complications.
Citation: Al Shaibi MA (2021) Blunt Abdominal Trauma Causing Intra-Abdominal Bleeding from an Undescended Intra-Abdominal Testis in a Syndromic Adult Patient. J Trauma Acute Care Vol.6 No.7
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.