Past
Until today, there are assumptions that brain death was “invented” at Harvard Medical School in 1968 for the single purpose to harvest organs. Those who argue into this direction cite an “ad hoc” publication [1] that followed these first and unsavory transplantations of human hearts [2,3]. The main protagonist was Hans Jonas [4] obviously unaware of primary literature. Admittedly, most of it was not published in English [2,3].
One might have expected at least that official guidelines (German: Richtlinien) would refer to historical data. But this wasn’t realized for Germany [5] only the Harvard paper [1] is mentioned, there.
The concept of brain death fascinates by the fact that both, the very beginning as well as its completion can be exactly and completely determined for time, place and protagonists:
It started on August 27th, 1952 in Copenhagen with Ibsen and was fulfilled on March 11th, 1960 in Lyon by Pierre Wertheimer [6]:
On Monday, August 27th, 1952, the anesthesiologist, Ibsen in Copenhagen [6], founded modern intensive care medicine, when rescuing a 12 year old girl: Vivi suffered from poliomyelitis with tetraplegia and was in danger of suffocation. Ibsen changed the ventilation by iron lung (i.e., preserved own respiration supported by intermittent negative pressure without protection of the upper airways) into a ventilation with intermittent positive pressure via endotracheal tube and pharmacological deactivation of spontaneous breathing. By this means he lowered the mortality of respiratory insufficiency due to polio from 84% to 21%. In consequence, the problem of long term ventilation developed.
In 1953 Riishede and Ethelberg [7] from Aarhus/Denmark published their angiographic findings of five patients in deepest coma under ventilation: there was no filling of the intracranial vessels. All these patients died. At autopsy, all carotides proved to be patent. Only later, this apparent contradiction was understood as a sequence of an increased intracranial pressure during intensive care treatment. By the same year, Wertheimer and Allègre [8] published their data on missing EEG potentials in patients in deepest coma on the intensive care unit in Lyon.
Since 1956 there were observations from pathologists in Paris and Basel [3,10,24], documenting different degrees of intravital autolysis of the central nervous system from deceased coma patients after long term ventilation.
Because of the increasing complexity of intensive care medicine Haid [11], anesthesiologist from Innsbruck/Austria, addressed the Pope in 1957: “Is it allowed to terminate mechanical ventilation in obviously hopeless cases?”
Pius [12] invited Haid and his team to come to Rome and answered the questions in a still valid manner during his historical speech in French delivered on November 24th, 1957: ‘Yes’, he said, ‘it is allowed to stop mechanical ventilation if the soul of the patient has already left the body’. And he added: ‘It remains for the responsibility of physicians (not of the church) to define and to determine death’.
In January 1959, the Lyon group around Wertheimer [13] published their concept of brain death in a way that is principally valid until today (prerequisites, clinical syndrome, proof of irreversibility). By March 11th, 1960, Wertheimer et al. [14] terminated the ventilation in a 13 years old boy after intensive care treatment due to a severe traffic accident after the determination of brain death by respective results in clinical examination, EEG and angiography. This was the very first published termination of therapy after determination of brain death. Wertheimer validated the concept, that brain death means death of an individual person (in contrast to the apprehension of contemporary neurologists in Paris [26].
He realized what the Pope meant by his analogy to intensive care medicine namely that the soul might have been gone, despite the fact that the rest of the body is still supplied with oxygen via respirator and from a phenomenological point of view the body discloses a seemingly vital appearance [2,3,12]. Though this dual view of body and soul is somewhat simple, and does not at all correspond to all nuances of bible and philosophy, a concept of exitus animae seems to be well established in traditional medicine in most parts of the world.
All these events happened in Europe from 1952 to 1960 independently from any reflection on organ donation: The first published transplantation of organs from a patient in coma dépassé occured on June 3rd, 1963, in Leuven/Belgium [15].
At least since the publications of Wertheimer and his group [8,13,14] the entity of brain death is well established and reliablel, until today. Herewith, the first three levels of the hierarchic model of Kurthen and Linke [16] on how to determine death proved to be completely fulfilled. He advised to attend the four questions in a strict follow up:
- Who or what is dead? (1st level: Attribution)
- How is death defined? (2ndlevel: Definition)
- Which criteria must be fulfilled? (3rd level: Criteria)
- Which tests have to be performed? (4th level: Tests)
It is admitted that tests (4th level) may differ to some degree over time, because of new inventions (sonography, computed tomography, nuclear medicine, etc.). But this does not interfere with the essence of the brain death concept.
Present
In 1959, the German penologist Roxin, as cited by Frowein and Firsching [17] postulated to regulate the determination of brain death by law at the 86th meeting of the German Society of Surgery in Munich. In Germany a “decision-making aid” (Entscheidungshilfe) exists since April 9th, 1982. It has been published by the “Federal Medical Association” (FMA; Bundesaerztekammer) by a “Scientific Advisory Board” (SAB; Wissenschaftlicher Beirat). Respective updates came out in 1986, 1991, and 1997. After the “transplantation law” (TPL; Transplantationsgesetz, TPL) came into effect by December 1st, 1997, the FMA had to formulate quasi legal guidelines instead of decision-making aids they were published in 1998. The fourth update of these guidelines is valid in Germany since July 6, 2015 [5].
Whereas the Pope [12] had formulated that it belongs to the very own responsibility of physicians to define and determine death in 1957, one must admit that a time of increasing secularization went by, with a certain loss of authority orthodoxy and some desire of legal codification. Maybe by different reasons, British people don’t favour the legal regulation, until now.
What are actual difficulties to include the complex entity of brain death into law, and language?
1. When discussing the new “designation” for the above mentioned “concept” of brain death in Germany, semiotic basics were at risk to be forgotten: One century ago, the “semiotic triangle” of Plato (object–concept–designation) has been revitalized by Ludwig Wittgenstein [18]. Within his Tractatus he pointed out, that object, concept and designation should be correlated unequivocally, ‘otherwise most fundamental confusion occurs easily (there is plenty of it in philosophy)’. In addition, one could expect this coherency to be part of a physician’s intellectual everyday life at least after the publications of Eco [19] Nevertheless, the President of the FMA [9] declared “brain death” to be a colloquial designation, despite the above unrolled fact, that “brain death” is a serious concept. Both, concept and designation of “brain death” (Hirntod) are well established and funded in the German idiom since 1970 [2]. – Since the 4th update of the guidelines, the German FMA favours the designation “complete, doubtless and irreversible loss of function of telencephalon, brainstem, and cerebellum” (German: Grosshirn, Kleinhirn, Hirnstamm) because this is the wording of TPL §3 [25].
2. In 1840, the jurist Savigny [20] had claimed that death (in contrast to life) is self-evident and needs no definition. As a consequence there is no definition of death in German law, until now. Simply by this reason questions as does brain death mean death of a person?” prove to be unanswerable. It remains open, on which level an answer is expected: physicians have defined brain death well, but there is no definition of death in German law, neither in civil - nor in criminal law. The resulting asymmetry is hardly to solve consistently.
3. In Germany, the concept of “irreversible loss of function of telencephalon, brainstem, and cerebellum” (meaning brain death) is exclusively mentioned within the transplantation law (§3): this fact may induce the incorrect assumption that its determination is only performed in those coma patient, who are eligible for organ transplantation improperly suggesting a primarily targeted interconnection between the determination of brain death and harvesting organs. As it has been pointed out above, this is definitely inappropriate in respect of history and essence of brain death. In so far the concept of brain death is improperly assigned: brain death deserves a self-sufficient reference in German law. Physicians first of all ask for the eventuality of brain death “eo ipso” [5] that means: to clarify the situation of and resulting further procedures for the patients, either maintenance or termination of treatment or whatever else.
4. The text of German TPL [25] does not argue in a positive way, that it is allowed to harvest organs after the determination “irreversible loss of function of telencephalon, brainstem and cerebellum” (meaning brain death).
4a: The text of German TPL § 3 [1] 2 explain positively: “It is allowed to take organs, if the death of an organ donor is determined”. As pointed out above, it is not so easy to treat death and brain death as equivalent by means of German law, because there is no definition of death itself within the law.
4b: Then the text of TPL § 3 [15] 2 explicates in terms of a double negation: “It is not allowed to take organs, unless the ‘irreversible loss of function of telencephalon, brainstem and cerebellum’ is determined”. It remains unclear, whether this double negation in fact means an affirmation. Obviously the legislator did not want to answer the question, whether brain death means death at this point, but to give the minimal condition under which circumstances harvesting of organs means no mayhem and is not punishable.
5. If someone tries to formulate extensively precise mistakes may occur: ´The (German) wording of “irreversible loss of function of telencephalon, brainstem and cerebellum” as a quasi-synonym for brain death implies a propaedeutic inconsistency according to the valid anatomical terminology [21] formally the diencephalon is not mentioned! Without any doubt both, the Scientific Advisory Board of the FMA as well as the legislator had the intention to summarize all parts of the central nervous system above the foramen occipitale magnum. They could have formulated “forebrain” (German: Vorderhirn) instead of “telencephalon” (Großhirn), because the English term “forebrain” means “telencephalon” and “diencephalon”. But they didn’t. Once again, this fact underlines the above mentioned thesis that it is not so easy to consistently weave in the essence of the relatively new concept of brain death in traditional language and law.
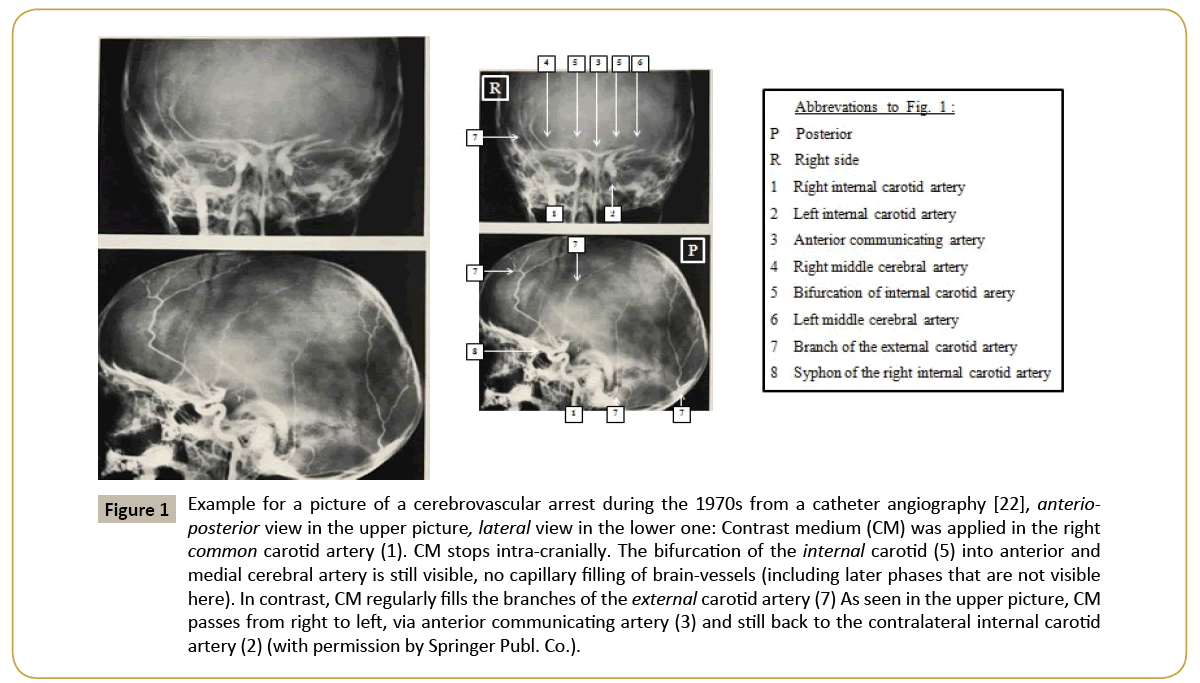
6. Not all citations of the FMA publication [5] are in concordance to what is written in the references itself. This can be exemplified by the implementation of computer tomography angiography (CTA) as an additional tool to verify a cerebrovascular arrest [5] (point 3.2.3/annotation 9). The citations N° 149-152 from the Welschehold group is given as respective reference in the article [5]. But the suggested criteria for the stop of contrast medium in static scans are not identic to the criteria in the text of the FMA [5]. This leads to false negative detection of cerebrovascular arrest. A missing filling of the cerebrovascular capillaries can easily be detected by dynamic catheter angiography despite of some intracranial „stasis filling“. If such intracranial “stasis fillings” are examined by static CTA and described according to the wording of the actual valid German guidelines a false negative result would occur. This absurdity can be demonstrated by a classical example from the textbook of Kautzky et al. [22] (Figure 1), the pictures of a classical cerebrovascular arrest in catheter angiography are depicted with typical intracranial rest filling, but without capillary perfusion. Such a picture could not be judged as “cerebrovascular arrest” according to the wording of the actual German guidelines for CTA, because the contrast medium formally stops too far intracranially – despite the fact, that there is objectively no cerebrovascular perfusion.
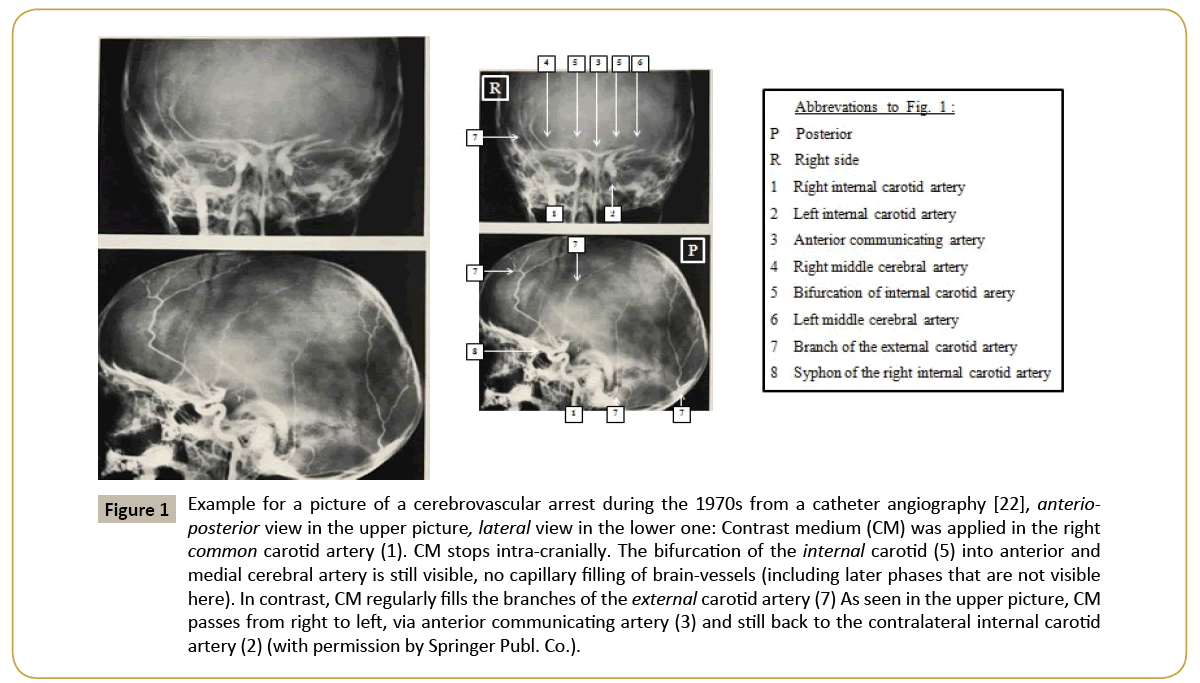
Figure 1: Example for a picture of a cerebrovascular arrest during the 1970s from a catheter angiography [22], anterioposterior view in the upper picture, lateral view in the lower one: Contrast medium (CM) was applied in the right common carotid artery (1). CM stops intra-cranially. The bifurcation of the internal carotid (5) into anterior and medial cerebral artery is still visible, no capillary filling of brain-vessels (including later phases that are not visible here). In contrast, CM regularly fills the branches of the external carotid artery (7) As seen in the upper picture, CM passes from right to left, via anterior communicating artery (3) and still back to the contralateral internal carotid artery (2) (with permission by Springer Publ. Co.).
7. The actual German guideline [5] contains a postulate for physiological margins for which a scientific base in the literature could not be found: Annotation 3 deals with the apnoe test for former healthy patients. It gives the paCO2 window to start with by 35 to 45 mm Hg. The lower limit, 35 mm Hg, could not be validated for such a purpose.
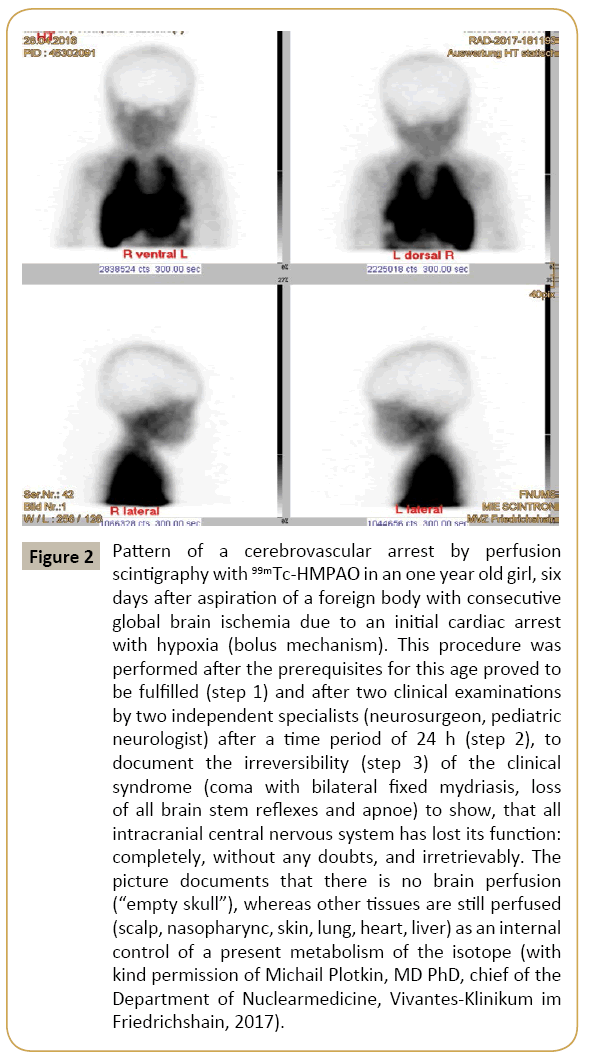
8. This guideline [5] contains different margins for blood pressure (in adults) to exclude arterial hypotonia during the procedure of documentation of a cerebrovascular arrest: To primarily document that the prerequisites are fulfilled, it has to be confirmed on page 1 of the protocol that there is “no shock“ by documentation of the systolic blood level in (mm Hg). Within the text of the guidelines [5] respective preconditions concerning the mean arterial pressure are demanded for CTA, Duplex- and Doppler-sonography 60 mm Hg, for four vessel catheter angiography 80 mm Hg and no respective quantification for the brain perfusion scintigraphy (Figure 2).
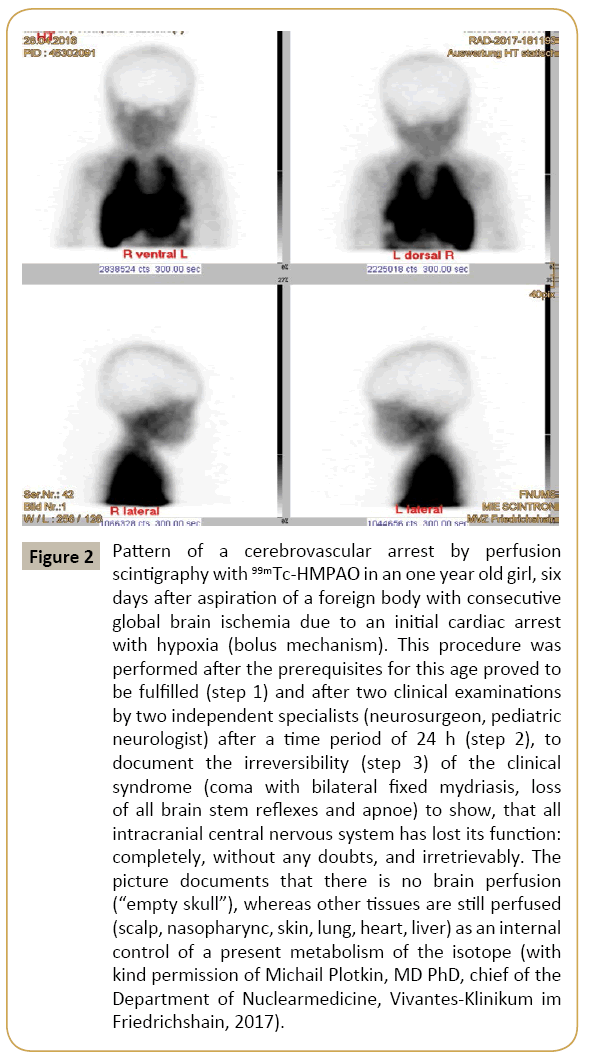
Figure 2: Pattern of a cerebrovascular arrest by perfusion scintigraphy with 99mTc-HMPAO in an one year old girl, six days after aspiration of a foreign body with consecutive global brain ischemia due to an initial cardiac arrest with hypoxia (bolus mechanism). This procedure was performed after the prerequisites for this age proved to be fulfilled (step 1) and after two clinical examinations by two independent specialists (neurosurgeon, pediatric neurologist) after a time period of 24 h (step 2), to document the irreversibility (step 3) of the clinical syndrome (coma with bilateral fixed mydriasis, loss of all brain stem reflexes and apnoe) to show, that all intracranial central nervous system has lost its function: completely, without any doubts, and irretrievably. The picture documents that there is no brain perfusion (“empty skull”), whereas other tissues are still perfused (scalp, nasopharync, skin, lung, heart, liver) as an internal control of a present metabolism of the isotope (with kind permission of Michail Plotkin, MD PhD, chief of the Department of Nuclearmedicine, Vivantes-Klinikum im Friedrichshain, 2017).
9. Both, legislation as well as FMA, have not calculated the consequences of the fourth update of the guideline [5] in full consequence. It is absolutely advisable, that both examiners have to fulfill the criteria of board certification (German: Facharzt) and both have to be independent from organ transplantation. It sounds also reasonable, that for adults one of them is a neurosurgeon or a neurologist (in children up to the 14th birthday: a. neuropediatrician). But as a follow of these conditions, more than 50% of those hospitals, where organs are donated, are unable to define brain death by their own staff [23]. Nevertheless TPL §9a [15] 1 postulates, that brain death has to be diagnosed whenever there is a respective suspicion (even for hospitals without neurosurgery, neurology or pediatric neurology). But it is not anticipated, by which means this could be organized and paid.
Future
The concept of brain death has been validated since 1960. No false positive diagnosis has been published, if the procedure follows the guidelines [5]. Nevertheless it seems to be necessary, to corroborate the essence of brain death for physicians and non-medical people as well. But it has also turned out to be difficult, to succeed in this regard by generating more and more guidelines and formalisms. There is no doubt; the German guideline [5] needs some editorial update for minor and formal inconsistencies. At the moment, there is a respective processing at the level of the FMA.
To guarantee a persistent acceptance of the concept of brain death, it seems advisable, to include more “soft skills”:
A. “The diagnosing physician is personally and indivisibly responsible for the process of determination of brain death“. Such a sentence opened or finished the German guidelines on brain death since 1982; but in the recent one [5] it is omitted incomprehensibly though this is still essential.
B. The protocols need to be filled out carefully with legible signs for date, place, name, specialty, follow up, annotation, consistency, signature so called “old fashioned secondary virtues“ that remind more on customs on higher trade schools of the 1950s than on usual performances in contemporary high schools. But this is indispensable. Nearly all official inquiries concerning brain death deal with the insufficiency of filling out a protocol. Some diligence may be missed in working out these sheets for the new guideline. No clinical trial of applicability has been performed. The impact of potential criticism has been underestimated.
C. The personal handing over of data and protocols from the one team that determines brain death to the other team that takes the organs should be codified within TPL and guidelines. The bulk of misunderstandings on this post-mortal interface grounds in the fact that clinicians are so busy, that they cannot but leaving behind a paper work instead of speaking to the successing group.
D. The author is convinced that both brain death and organ donation should become an essential part of school curricula for biology and ethics. Experienced physicians should realize this and accept a mandate over generations and never stop to explain physiology and pathophysiology of the end of life in an understandable and caring manner, with calm and lucidity in an understandable language: “Don’t expect, that they understand us by the very beginning. But don’t give up to take a stand for a dignified issue” [2] (p. 16).
Potential Conflict of Interest
The author is a Christian and has no conflict of interest concerning this article.
Acknowledgement
The author thankfully acknowledges valuable advices from Heinz Angstwurm (Neurology/Munich), Karsten Fischer (Politology/ Munich), Reinhold Frowein (Neurosurgery/Cologne), Ernst Hauck (Jurisprudence/Muenster), Guenter Jautzke (Pathology/ Berlin), Martin Kurthen (Epileptology/Zuerich), Christoph Lang (Anesthesiology/Erlangen), Mats Moskopp (Physiology/ Dresden), John Pickard (Neurosurgery/Cambridge), László Solymosi (Neuroradiology/Wuerzburg).
References
- (1968) A definition of irreversible coma. Report of the Ad hoc committee of the Harvard medical school to examine the definition of brain death. JAMA 205: 85-88, 337-340.
- Moskopp D (2015) Hirntod. Konzept – Kommunikation – Verantwortung. Stuttgart, Thieme.
- Moskopp D (2017) Das Konzept des Hirntodes wurde in Europa zwischen 1952 und 1960 entwickelt. Eine Uebersicht zur Historie. Nervenheilkunde 36: 423-432.
- Jonas H (1968) Gehirntod und menschliche Organbank - Zur pragmatischen Umdefinierung des Todes. In: Jonas H (ed) Technik, Medizin und Ethik. Praxis des Prinzips Verantwortung. Frankfurt/Main, Suhrkamp, 219: 224, 228.
- (2015) Directive pursuant to Section 16 (1) (1) (1) TPG for the rules for the determination of death pursuant to Section 3 (1) (1) (2) TPG and the procedural rules for determining the definitive, irrevocable Failure of the total function of the cerebrum, the cerebellum, and the brainstem according to § 3 para. 2 no. 2 TPG, fourth update. German Aerzteblatt, Federal Chamber of Physicians.
- Ibsen BA (1954) The anesthetist’s viewpoint on the treatment of respiratory complication in poliomyelitis during the epidemics in Copenhagen 1952. Proc R Soc Med 47: 72-74.
- Riishede J, Ethelberg S (1953) Angiographic changes in sudden and severe herniation of brain stem through tentorial incisure. Report of five cases. Arch Neurol Psychiatry 70: 399-409.
- Wertheimer P, Allègre G (1953) Note sur les comas traumatiques prolongués. Rev Neurol (Paris) 89: 509-511.
- Montgomery FU (2015) Bewaehrtes kombiniert mit aktuellen Erkenntnissen der medizinisch-wissenschaftlichen Forschung. Deutsches Ärzteblatt.
- Scheidegger S (1961) Histopathologie der Bewusstseinsstoerungen. In: Staub H, Thoelen H (edn) Bewußtseinsstoerungen – Symposion Januar 1961, St. Moritz, Schweiz. Stuttgart, Thieme, pp: 38-58.
- Haid B (1958) Religioes-sittliche Fragen betreffend die Wiederbelebung (Resuscitation, Reanimation). Der Anaesthesist 7: 241-243.
- Pius XII (1957) Discours en réponse à trois questions de morale médicale sur la reanimation. Acta Apostolica Sedis 49: 1027-1033.
- Wertheimer P, Jouvet M, Descotes J (1959) À propos du diagnostic de la mort du système nerveux dans les comas avec arrêt respiratoire traités par respiration artificielle. Presse Médicale 67: 87-88.
- Wertheimer P, de Rougemont J, Descotes J, Jouvet M (1960) Données angiographiques relatives à la mort de l’encéphale au cours des comas avec arrêt respiratoire (Coma dites dépassés). Lyon Chirurgical 56: 641-648.
- Anonymus (1963) Deux malades survivent depuis plusiers semaines à la greffe d’un rein prélevé sur un cadaver – Contribution importante d’un jeune chercheur belge. La Libre Belgique 1: 10-11.
- Kurthen M, Linke DB (1994) Vom Hirntod zum Teilhirntod. In: Hoff J, in der Schmitten J (ed) Wann ist der Mensch tot? Organverpflanzung und Hirntodkriterium. Reinbek bei Hamburg, Rowohlt, pp: 82-94.
- Frowein RA, Firsching R (2004) Geschichte der neurochirurgischen Hirntoddiagnostik in Deutschland. Vortrag auf der 55. Jahrestagung der Deutschen Gesellschaft fuer Neurochirurgie. Cologne.
- Wittgenstein L (1918/1921) Tractatus logico-philosophicus 3.32 – especially 3.324.
- Eco U (1977) Zeichen: Einfuehrung in einen Begriff und seine Geschichte. Frankfurt/Main, Suhrkamp.
- Savigny CPV (1840) System des heutigen Roemischen Rechts, Band 2. Berlin, Veit & Co., p: 17.
- (1998) Terminologia anatomica: international anatomical terminology By the Federative Committee on Anatomical Terminology (FCAT), p: 108.
- Kautzky R, Zuelch KJ, Wende S, Taenzer A (1976) Der cerebrale Kreislaufstillstand. In: Neuroradiologie auf neuropathologischer Grundlage. Berlin, Springer, pp: 171-172.
- Blum K (2016) Impact of the amended directive on the detection of irreversible brain function loss in hospitals. A survey commissioned by the German hospital between August 2015 and September 2016.
- Hunt WE, Meagher JN, Friemanis A, Rossel CW (1962) Angiographic studies of experimental intracranial hypertension. J Neurosurg 29: 1023-1032.
- Lilie H (ed) (2012) Gesetz über die Spende, Entnahme und Uebertragung von Organen und Geweben (Transplantationsgesetz – TPG). Halle, Schriftenreihe Medizin-Ethik-Recht. Band 6, 2ed–last modification, p: 2623.
- Mollaret P, Bertrand I, Mollaret H (1959) Coma dépassé et necroses nerveuses centrales massives. Rev Neurol (Paaris) 101: 116-139.