Original Article - (2017) Volume 18, Issue 5
Department of Surgery, Showa Inan General Hospital, Akaho 3230, Komagane, Nagano 399-4117, Japan
Received July 04th, 2017-Accepted July 27th, 2017
Introduction Although some authors have reported that retrograde infection by longterm placement of prophylactic drain may be the main cause of organ/space surgical site infection after pancreaticoduodenectomy. Materials and Methods The study included 93 patients who underwent pancreaticoduodenectomy. We assessed the risk factors for organ/space surgical site infection and examined the microorganisms detected at organ/space surgical site infection to determine the origin of microorganisms. Results Of the 93 patients, 29 were included in the organ/space surgical site infection+ group. The risk factors for organ/space surgical site infection on univariate analysis were blood transfusion (OR, 2.70; p <0.05), the amount of peritoneal lavage <5,000 mL (OR, 3.08; p<0.05), open type of prophylactic drain (OR, 2.92; p<0.05), and the incidence of pancreatic fistula (OR, 7.54, p<0.001). The microorganisms, detected in cultured specimen from prophylactic drain at organ/space surgical site infection, belonged to intestinal flora in 22 out of 29 patients (75.9%), and 30 of all 48 detected microorganisms (62.5%) were occupied by those of intestinal flora. Conclusion We confirmed that pancreatic fistula was the most significant risk factor. Based on the microorganisms identified, retrograde infection via drain placement could not be confirmed; therefore, the time of the drain removal should be carefully considered.
Pancreaticoduodenectomy; Pancreas
o/s-SSIs organ/space surgical site infection; PD pancreaticoduodenectomy
Surgical site infection (SSI) after abdominal gastrointestinal surgery extends hospital stay and increases medical costs. Additionally, it has a negative impact on not only patients but also hospital management [1, 2, 3]. Therefore, techniques should be identified to avoid and appropriately treat SSI.
Many studies have reported that a prophylactic drain is not required for gastrointestinal surgery [4, 5], and one study concluded that the drain was needed only at esophagectomy and total gastrectomy [6]. However, other studies have advocated the requirement of a prophylactic drain in cases of pancreatic resection, including pancreaticoduodenectomy (PD) [7, 8, 9]. Several studies have reported that long-term dwelling of the drain can cause pancreatic fistulas and increase the incidence of organ/space SSIs (o/s-SSIs) [10, 11]. Because clinicians often have the impression that complications such as o/s- SSI and pancreatic fistulas would be more serious without a drain than complications with a drain [7], these beliefs may contradict the findings of many previous studies.
The present study analyzed the risk factors for o/s- SSI after PD and examined the relationship between prophylactic drain placement and the occurrence of o/s- SSI according to the classification of microorganisms detected in samples cultured from the drain at the time of o/s SSI.
A total of 97 consecutive patients who underwent PD were considered for inclusion in this retrospective study. However, four patients were excluded because of lack of data. Therefore, 93 patients were finally enrolled between 2001 and 2014. These patients were divided into either the o/s-SSI-positive (o/s-SSI+) group, which had a positive bacterial culture of the drainage fluid, or the o/s-SSI-negative group (o/s-SSI−), which had a negative bacterial culture of the fluid. The risk factors for o/s-SSI were examined by comparing the following variables between the two groups: age; sex; body mass index (BMI); indication for operation; laboratory data at first visit, including total bilirubin level, albumin level, hemoglobin A1c (HbA1c) level, white blood cell (WBC) count, and C-reactive protein (CRP) level; preoperative biliary stent placement; American Society of Anesthesiologists physical status (ASA-PS) classification; operation time; operative blood loss; blood transfusion; quantity of peritoneal lavage during operation; type of prophylactic drain used (open or closed); duration of prophylactic drain placement; duration of prophylactic antibiotic administration; and pancreatic fistula development.
Additionally, by differentiating the bacteria detected in the drainage fluid and by identifying the relationship between the bacteria from the drainage fluid at the time of o/s-SSI and the bacteria from bile samples obtained preor intra-operatively, we determined whether the causative bacteria of o/s-SSI were present in the abdominal cavity or outside the body.
The preoperative biliary stents were selected from the following: endoscopic biliary stent, endoscopic nasobiliary drainage tube, and self-expandable metallic stent, according to the preference of the endoscopic physician and the quality of the existing cholangitis.
Prophylactic peritoneal drains were placed in all patients. The types of prophylactic drains were “open” and “closed.” The former was used from 2001 to 2007, and the latter was used thereafter. The closed drain was maintained with vacuum at low pressure. o/s-SSI was suspected by the property of the drain fluid and diagnosed from results of the bacterial culture of the fluid.
The severity of the pancreatic fistulas was classified according to International Study Group on Pancreatic Fistula definitions [12].
Data are expressed as means ± standard deviation (SD). Patient characteristics and perioperative and postoperative variables were compared between the o/s- SSI+ and o/s-SSI− groups using the χ2 and Fisher exact tests. Variables with p-values<0.05 were incorporated into a logistic regression model in order to determine the independent risk factors for o/s-SSI. The independent risk factors were expressed as odds ratios (ORs) and 95% confidence intervals (CIs). All statistical analyses were performed using JMP, version 12 (SAS Institute, Cary, NC, USA). P-values <0.05 were considered statistically significant.
The mean age of the patients was 72.6±9.3 years (range, 52–92 years). Of the 93 patients, 58 were male and 35 were female. The indications for operation were pancreas head tumors in 44 patients (pancreatic head cancer in 36, intraductal papillary mucinous neoplasm in seven, and serous cystadenoma in one), bile duct tumors in 34 patients (bile duct cancer in 33, and gall bladder cancer in one), tumors of the papilla of Vater in seven patients (cancer in five and adenoma in two), duodenal tumors in five patients (cancer in three, gastrointestinal stromal tumor in one, and lymphoma of mucosa-associated lymphoid tissue in one), and others in two patients (fibrosing cholangitis in one and gastric cancer recurrence in one).
Comparison of Perioperative Variables between the o/s-SSI+ and o/s-SSI− Groups
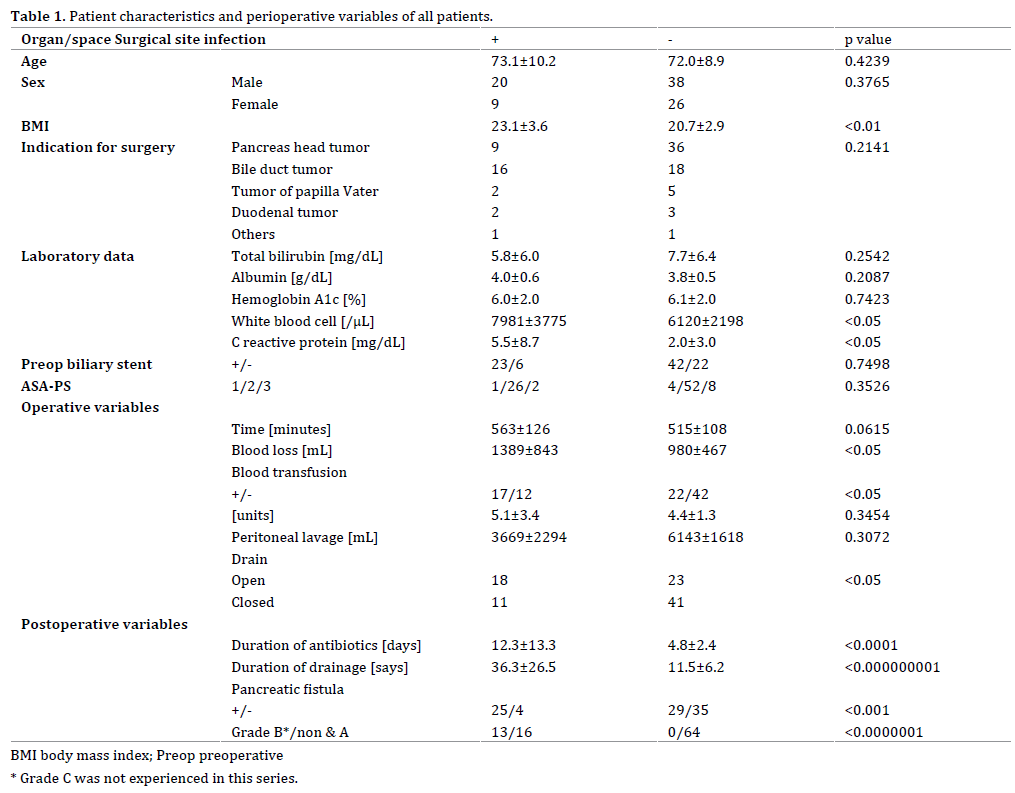
Of the 93 patients, 29 and 64 were included in the o/s- SSI+ and o/s-SSI− groups, respectively. The comparison of variables between the o/s-SSI+ and the o/s-SSI− groups are presented in Table 1. Age and sex did not differ significantly between the groups. However, BMI was significantly higher in the o/s-SSI+ group than in the o/s- SSI− group (23.1±3.6 kg/m2 vs. 20.7±2.9 kg/m2, p<0.01). The number of patients with pancreas head tumors was higher in the o/s-SSI− group than in the o/s-SSI+; however, the difference was not statistically significant. The total bilirubin, albumin, and HbA1c levels did not differ significantly between the two groups. The WBC counts (7981±3775/mL vs. 6120±2198/mL, p<0.05) and CRP levels (5.5±8.7 mg/dL vs. 2.0±3.0 mg/dL p<0.05) were significantly higher in the o/s-SSI+ group than those in the o/s-SSI− group. The incidence of preoperative biliary stent placement and ASA-PS classifications did not differ significantly between the two groups. Among operative variables, blood loss was significantly higher in the o/s- SSI+ group than that in the o/s-SSI− group (1389±843 mL vs. 980±467 mL, p<0.05), and blood transfusions were performed more frequently in the o/s-SSI+ group than in the o/s-SSI− group (17/29 vs. 22/64, p<0.05); however, operative time and volume of peritoneal lavage did not differ significantly between the two groups. The open drain induced o/s-SSI significantly more frequently than the closed drain (18/41 vs. 11/52, p<0.05). The duration of prophylactic antibiotic administration was significantly longer in the o/s-SSI+ group than in the o/s-SSI− group (12.3±13.3 days vs. 4.8±2.4 days, p<0.0001). The duration of drain placement was significantly longer in the o/s- SSI+ group than in the o/s-SSI− group (36.3±26.5 days vs. 11.5±6.2 days, p <0.000000001). All grades of pancreatic fistulas occurred in 54 of 93 patients, and they were significantly more common in the o/s-SSI+ group than in the o/s-SSI− group (25 of 29 patients vs. 29 of 64 patients, p <0.001). High-grade (grades B and C) pancreatic fistulas were not observed in the o/s-SSI− group (13 of 29 patients vs. 0 of 64 patients, p <0.0000001).
Risk Factors for o/s-SSI
The risk factors for o/s-SSI in univariate analysis are presented in Table 2. The risk factors included blood transfusion (OR, 2.70; p<0.05), peritoneal lavage volume<5,000 mL (OR, 3.08; p<0.05), open type of prophylactic drain (OR, 2.92; p<0.05), and the incidence of pancreatic fistula (OR, 7.54, p<0.001).
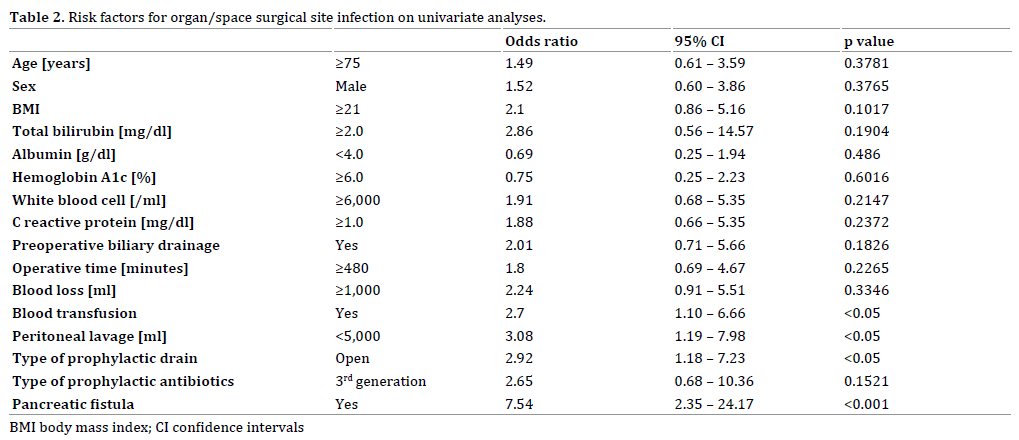
Multivariate logistic regression analysis did not reveal an independent risk factor among the risk factors for o/s-SSI.
Microorganisms Related to o/s-SSI
Twenty-nine of the 93 patients were diagnosed with o/s-SSI. Table 3 shows the microorganisms detected in cultured fluid from the prophylactic drain when o/s-SSI was clinically suspected. The microorganisms belonging to intestinal flora were isolated from the drained fluid sampled from 22 out of the 29 patients (75.9%). The postoperative period, when microorganisms were detected in the drained fluid, was 9.4±4.5 days (2 – 22 days, median 9 days). There was not a significant difference in this period between patients with open drains (8.4±5.1 days, 2 – 22 days, median 7 days) and those with closed drains (11.1±3.0 days, 7 – 16 days, median 12 days) (p = 0.1300).
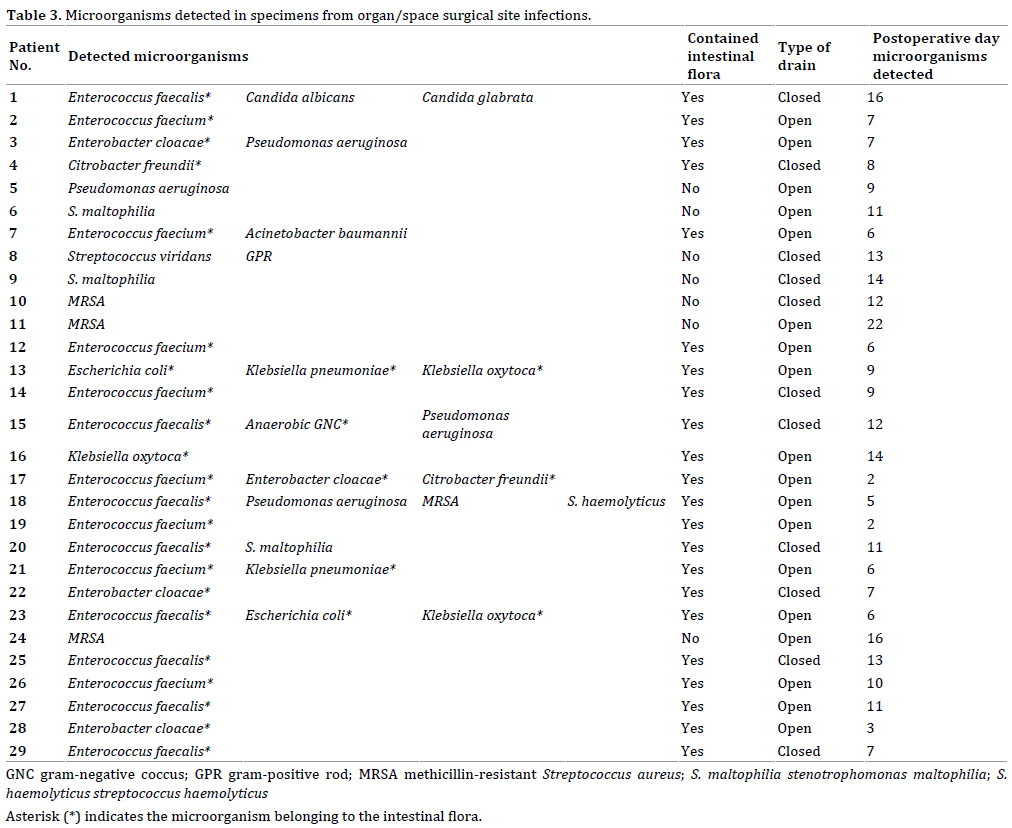
The 48 detected microorganisms included 30 (62.5%) typically observed in intestinal flora, 7 (14.6%) from environmental flora, 7 (14.6%) from skin flora, 1 (2.1%) from oral flora, 2 (4.3%) from fungi, and 1 (2.1%) from unclassified gram-positive rod. Bacteria of intestinal flora were the most common cause of o/s-SSI (Table 4).
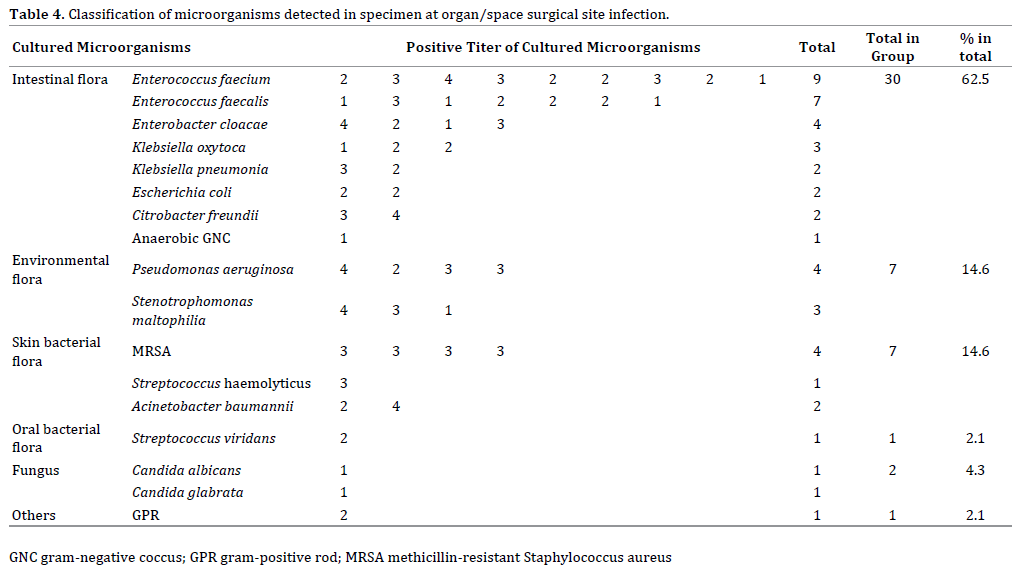
When classified by the type of drain, intestinal flora were identified in samples from 21 patients (67.7%), environmental flora in four patients (12.9%), and skin flora in six patients (19.4%) with open drains, while intestinal flora were identified in samples from nine patients (52.3%), environmental flora in three patients (17.6%), skin flora in two patients (11.8%), fungus in two patients (11.8%), and unclassified gram-positive rod in one patient (5.9%) with closed drains. These results indicated that there was not a significant difference between the two types of prophylactic drain.
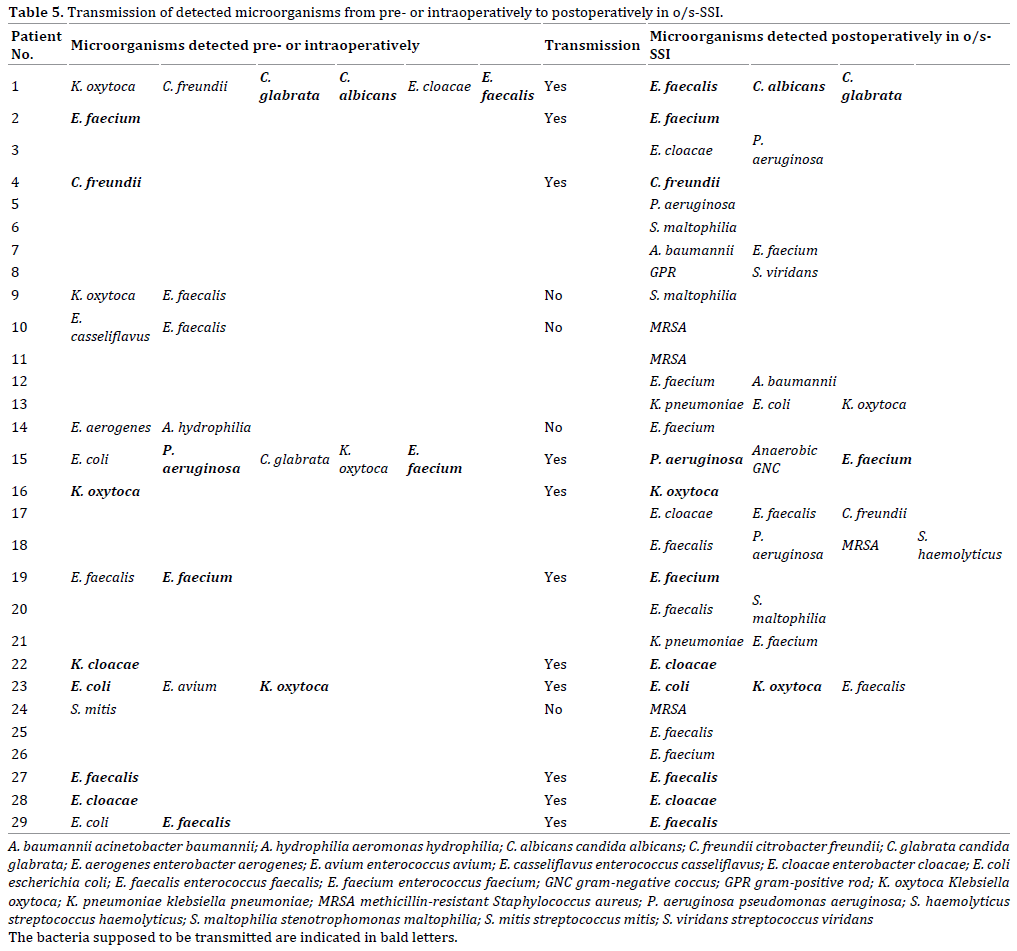
Microorganisms were identified in preoperatively sampled bile or intra-operatively collected biliary stent from 15 of 29 patients with o/s-SSI. In 11 of the 15 patients (73.3%), these microorganisms were the same kind as those detected at the site of the o/s-SSI. Pre- and intraoperative samples from the remaining 14 patients were free from biliary microorganisms; in 10 of these patients (71.4%), the microorganisms detected in the o/s-SSI samples belonged to intestinal bacterial flora (p = 0.1729).
SSI is the most common type of nosocomial infection, which is defined as an operation-related infection that occurs at or near the incision site within 30 days, according to the criteria from the United States Centers for Disease Control and Prevention (CDC) [13].
The reported incidence rates of o/s-SSI after colorectal surgery, and hepatectomy are 2.8–10% [5, 14, 15] and 4.0–8.6% [16, 17]. In comparison, the reported incidence rates of o/s-SSI after PD are 47.8% (195 of 408 cases) [9] and 45.0% (27 of 60 cases) [18]. In the present study, the incidence of o/s-SSI after PD was 31.2% (29 of 93 cases), which was much higher than that after any other type of abdominal operation.
The relationship between prophylactic abdominal drains and o/s-SSI has become the subject of debate. Kato et al. reported that intra-abdominal abscesses after PD were found in the open-drain group only [19], and Sugiura et al. showed in multivariate analysis that the use of semiclosed drain system was significantly associated with o/s- SSI [9]. Also in our series, open drains were picked up as a risk factor for o/s-SSI. The superiority of closed-type drains has been confirmed for the suppression of o/s-SSI.
Only one paper was found, which concluded that perioperative transfusions were associated with increased risk factors of surgical site infections in newborns [20]. Also in our analyses, intraoperative blood transfusion was one of the risk factors of o/s-SSI. Because the necessity of blood transfusion depends on the condition of the patients, our efforts not to transfuse are limited.
There have been several reports of pancreatic fistulas as a risk factor for o/s-SSI after PD. Sugiura et al. emphasized that the presence of pancreatic fistulas was the strongest risk factor for o/s-SSI [9], and Nanashima et al. reported the results of multivariate analysis indicating that only postoperative pancreatic fistulas were significantly associated with SSIs [21]. Because there is a report that infection control could effectively prevent pancreatic fistulas [22], it is clear that there may be a close relationship between pancreatic fistulas and o/s-SSI.
To our knowledge, no reports have concluded that prophylactic drain placement after PD is meaningless for the prevention of o/s-SSI. Many authors [23, 24, 25] concluded that prophylactic drainage after pancreatic resection did not decrease the frequency and severity of postoperative complication; however, they did not always deny drain placement. Wang et al. [23] concluded that the necessity of drain placement was controversial, and Dou et al. [8] stated in their systematic review and meta-analysis that, although prophylactic drain placement did not have a beneficial effect on the clinical outcome, it did not significantly increase the risk of abdominal abscess formation and that the elimination of prophylactic abdominal drainage after PD led to a significantly increased mortality rate (OR, 2.39; p = 0.01). Based on the literature, it is impossible to deny the requirement of prophylactic drain placement after PD.
Kawai et al. reported that drain removal on postoperative day 4 was an independent factor in reducing the incidence of intra-abdominal infection [10]. Bassi et al. also reported that a prolonged period of drain insertion was associated with a higher rate of postoperative complication, and that, in patients at low risk of pancreatic fistula, drains could be safely removed on post-operative day three [11].
Thus, although the propriety of prophylactic drain placement is controversial, there appears to be a consensus that o/s-SSI may be less of a concern if the drain were to be removed within term three to four days. However, this consensus is inconsistent with the actual clinical course after PD.
Sugiura et al. concluded that bacterial contamination during PD had an adverse impact on the development of o/s-SSI [26]. Horzog et al. also concluded that SSI was often caused by the same microorganisms that were present in intraoperative bile duct cultures [27]. In addition, we showed intraoperative peritoneal lavage volumes <5000 mL to be a significant risk factor by univariate analysis for the occurrence of o/s-SSI; furthermore, the use of the antibiotics effective against the bacteria detected in the perioperative bile samples inhibit the occurrence of postoperative peritoneal infections [28, 29, 30]. Thus, microorganisms derived from the bile may contaminate the abdominal cavity intra-operatively, and induce o/s- SSI.
In our analyses, intestinal bacterial flora was detected in 75.9% patients with o/s-SSI (Table 3), and comprised 62.5% of all detected bacteria in patients with o/s-SSI (Table 4). Herzog et al. [27] and Sugiura et al. [9] also reported gut-derived microorganisms to be the predominant bacterial species in SSI foci. Because biliary bacteria are gut-derived and bile contamination may be the main cause of o/s-SSIs and intestinal bacteria were identified in o/s-SSI in patients with both open and closed drains, there is no contradiction in the conclusion that the origin of most o/s-SSI after PD was the intra-peritoneal space or organs and that retrograde infection through prophylactic drains is not the main cause of o/s-SSI (Table 5).
The results of the current study confirm that pancreatic fistulae are the most significant risk factor of o/s-SSI after PD; in addition, based on our analysis of the microorganisms detected in patients with o/s-SSI, the main causative microorganisms of o/s-SSI originate in the peritoneal space or organs. Several authors have recommended early removal of prophylactic drain in order to prevent retrograde infection through the drain, which could make o/s-SSI worse; therefore, it is necessary to analyze and investigate the various aspects related to drain management after PD.
The authors have no financial conflicts of interest concerning the manuscript to disclose.