Mini Review - (2017) Volume 0, Issue 0
Victor Domingos Lisita Rosa1*, Fernanda Maris Peria1 and Mariângela Ottoboni Brunaldi2
1Division of Clinical Oncology, Ribeirão Preto Medical School, University Hospital, University of São Paulo, Brazil.
2Division of Pathology, Ribeirão Preto Medical School, University Hospital, University of São Paulo, Brazil.
*Corresponding Author:
Victor Domingos Lisita Rosa
Victor Domingos Lisita Rosa, Division of Clinical Oncology
Ribeirão Preto Medical School, University Hospital
University of São Paulo, Ribeirão Preto, Brazil.
Tel: (55 16)3602-1000
E-mail: victor_lisita@yahoo.com.br
Received date: July 22, 2017; Accepted date: July 29, 2017; Published date: August 03, 2017
Citation: Rosa VDL, Peria FM, Brunaldi MO (2017) Carcinoma of Ampulla of Vater: Carcinogenesis and Immunophenotypic Evaluation. J Clin Epigenet. 3:25. doi: 10.21767/2472-1158.100059
The ampulla of Vater represents the epithelial junction of the main pancreatic duct and the distal bile duct, surrounded by the pancreatic head and duodenum parenchyma. Ampullary carcinoma can arise either from the intestinal epithelium or the epithelium covering the pancreatobiliary ducts. Many tumors develop from pre-existing adenomas, others evolve from precursor intraepithelial neoplasia supporting that two histological subtypes have different carcinogenesis. Thus, the question arises of classifying ampullary adenocarcinomas as the immunophenotypic pattern allowing a better understanding of the clinical implications of this neoplasm.
Keywords
Ampulla of Vater; Adenocarcinoma; Immunohistochemistry; Carcinogenesis; Immunophenotypic
Introduction
Ampullary carcinomas are rare neoplasms that originate within the ampullary complex, distally the confluence of the common bile duct and pancreatic duct. The incidence of ampullary adenocarcinomas is 4 to 6 cases per one million inhabitants per year, with a higher incidence in men (0.7/100,000) than in women (0.45/100,000) [1-3]. It accounts for less than 1% of all gastrointestinal tract tumors [4], and about 6% to 30% of periampular neoplasms [5]. Although better prognosis than other periampullary cancer, it is often difficult to distinguish the primary origin of the tumor in this region before the surgery, leaving the final diagnosis, most often through the pathology of the surgical specimen. It is a transition region between the ductal epithelium of the biliary tract and intestinal epithelium, the main histological subtypes being pancreatobiliary and intestinal. This classification has an important impact on the prognosis of patients and associated with lymph node involvement, histological grade and resectability influence the overall survival of the same [2,6-9].
Carcinogenesis: Genetic and Epigenetic Factors
The ampulla of Vater is a region of encounter of two types of epithelia (intestinal mucosa contiguous to the mucosa of the distal bile ducts), being stimulated by several digestive enzymes and chemical substances that constantly attack it, making it an area more susceptible for the development of neoplasm, that is, a transition epithelium constantly mechanically and chemically affected [10].
This is the most frequent site of adenomas and malignant tumors of the whole small intestine. In the same way, as in the colon, most ampullary carcinomas originate from preexisting adenomas with chromosomal instability, and develop through the process of carcinogenesis known as "adenoma-carcinoma" sequence [11].
This sequence is a model for the development of carcinoma from adenomatous lesions. This sequence is a carcinoma development model from adenomatous lesions. Several studies support this theory for ampullary adenocarcinomas such as, for example, the presence of residual adenoma up to 90% of adenocarcinomas ampullary [12], history of adenoma resection in 30% of patients with carcinoma of the ampulla of Vater [13] and the presence of carcinoma in situ in about 40% of the resected adenomas of this region [4]. Some cases of ampullary adenocarcinoma are related to polypoid syndromes such as Familial Adenomatous Polyposis (FAP), whose risk of developing neoplasia is 100 to 200 times greater than in the general population. The ampulla of Vater is the second region more likely to develop cancer in patients with FAP, behind colorectal region. Patients with ampullary adenocarcinoma associated with FAP usually present the disease earlier, on average in the fifth decade of life [14]. Early screening with endoscopy is an important factor for diagnosis of ampullary lesions in initial stages in patients with FAP.
More rarely, other genetic syndromes are also associated with ampullary adenocarcinoma, as Lynch syndrome (hereditary nonpolyposis colorectal cancer- HNPCC), Neurofibromatosis type I and Muir-Torre syndrome [12,15,16]. Histomolecular changes may occur not only at a specific point, but also over the entire exposed mucosa. Such changes, named "field cancerization" are also discussed in the pathogenesis of ampullary adenocarcinoma [17]. As example, the association of two or more primary tumors (synchronous and metachronous), the presence of neoplasia associated with squamous intraepithelial lesions and also the appearance of a second primary cancer after initial treatment. Therefore, the diagnosis of epithelial malignant lesions should address not only the isolated tumor, but the entire field where developed. A population-based study with database of Survellaince Epidemiology and End Results (SEER) reported data that support this theory for periampullary neoplasms. Ampulla of Vater, pancreas and bile ducts have the same embryonic origin (foregut) and this possibly relates to the coexistence of intraepithelial lesions and cancer in this region as well as association of two primary neoplasms [18]. Three studies showed the presence of pancreatic intraepithelial lesion (PanIN) in patients with ampullary carcinoma. The first study showed high-grade intraepithelial neoplasia in pancreatic ducts 22% of resected tumors [17]. Other found high-grade PanIN in seven of seventeen patients [19]. Lastly, others authors reported that the incidence of PanIN was similar between pancreatic adenocarcinomas and ampullary adenocarcinomas [20].
Although these studies have not been reported histological types it is possible to hypothesize that the pathogenesis of ampullary adenocarcinomas is different according to histology. It is inferred that intestinal-type ampullary adenocarcinomas evolve from the adenoma-carcinoma sequence as occurs in colorectal tumors, while pancreatic-type tumors are thought to evolve from precursor intraepithelial neoplasia as well as from pancreatic neoplasms.
Phenotypic Evaluation
Histologically, most tumors are adenocarcinomas and rarely present differentiation mucinous, papillary or adenoescamosa [1,21].
Ampular large tumors usually involve multiple structures, hindering their classification. Just as large tumors of the head of the pancreas, bile duct or duodenum may grow and involve the ampulla of Vater resembling a primary neoplasm ampullary [22].
The ampullary carcinoma can originate from the epithelium of the confluence of bile and pancreatic ducts, as well as the epithelium of the duodenal mucosa. Histopathologic evaluation may vary depending on the protocols adopted by the institutions and also depending on the individual experience of the pathologist (interobserver variability). The report assessed the pathologist about periampullary cancer is extremely important to confirm the diagnosis, determining prognosis, selection of potential patients for clinical trials of adjuvant treatment, as well as providing radiological and surgical correlation and collect data for records of population-based epidemiology and câncer [22].
Kimura et al described two histopathological patterns of ampulla of Vater adenocarcinomas: intestinal type and pancreaticobiliary type (Figure 1) [23]. The intestinal type is similar to the tubular adenocarcinoma of the colon or stomach, and probably has its origin in the duodenal mucosa. In contrast, pancreaticobiliary type appears to originate from the epithelium of the same name, given the frequent papillary arrangements found in this tissue type [23]. Albores-Saavedra et al. reviewed these criteria and classified the ampullary tumors according to histological findings [1].
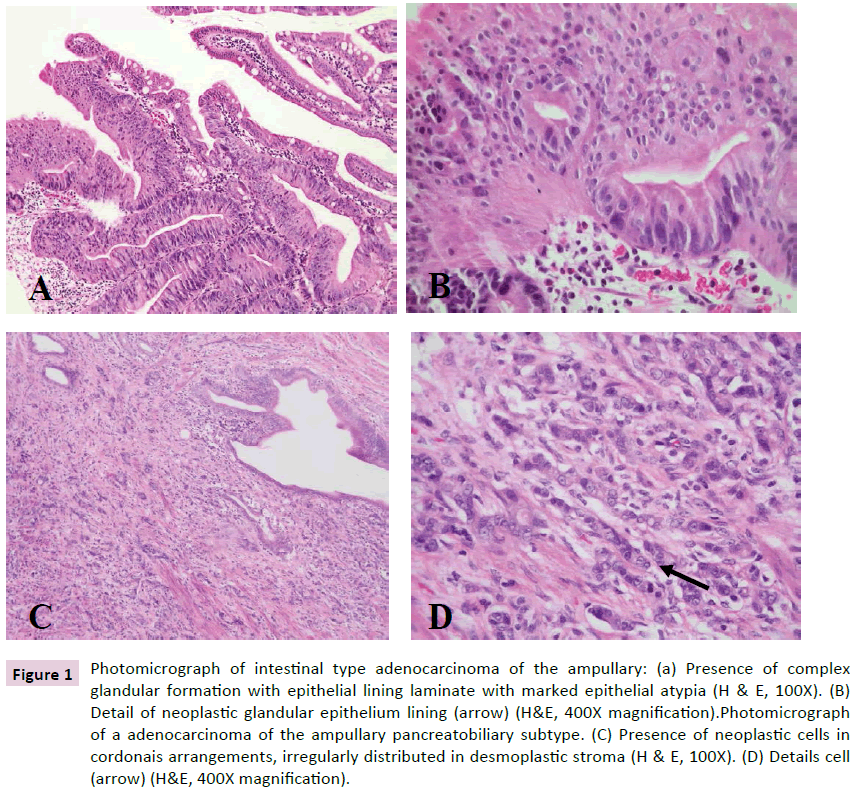
Figure 1: Photomicrograph of intestinal type adenocarcinoma of the ampullary: (a) Presence of complex glandular formation with epithelial lining laminate with marked epithelial atypia (H & E, 100X). (B) Detail of neoplastic glandular epithelium lining (arrow) (H&E, 400X magnification).Photomicrograph of a adenocarcinoma of the ampullary pancreatobiliary subtype. (C) Presence of neoplastic cells in cordonais arrangements, irregularly distributed in desmoplastic stroma (H and E, 100X). (D) Details cell (arrow) (H&E, 400X magnification).
Intestinal adenocarcinoma is the most prevalent among the usual types of ampullary neoplasia. Several studies have associated clinical and biological behavior of the ampullary carcinoma intestinal tumors [1,23-30]. Among the reasons are: the highest frequency of intestinal type in most studies (Table 1), the process of carcinogenesis by chromosomal instability (“adenomacarcinoma” sequence), as is observed in colorectal cancers. Furthermore, patients with FAP has a significant increase in the incidence of ampullary carcinoma in the general population, suggesting that the mechanism of carcinogenesis similar to intestinal tumors [31]. Other similarities between the neoplasms are: frequency K-ras mutation approximately 37% [32] and the consistent expression of cyclooxygenase-2 (COX-2) in 78% of cases [33].
| Year | N | Intestinal (%) | Pancreatobiliary (%) | Outhers (%) |
|---|---|---|---|---|
| 1994 | 51 | 25 | 75 | - |
| 2000 | 140 | 49 | 21 | 30 |
| 2004 | 55 | 27 | 44 | 29 |
| 2008 | 34 | 73.5 | 26.5 | - |
| 2008 | 118 | 46 | 45 | 9 |
| 2008 | 41 | 68.3 | 31.7 | - |
| 2009 | 170 | 47 | 24 | 21 |
| 2010 | 43 | 73 | 20 | 24 |
| 2014 | 313 | 22 | 55 | 23 |
| 2016 | 106 | 47.2 | 28.3 | 24.5 |
Table 1: Ampullary adenocarcinoma: distribution according histopathological type.
The pancreatobiliary type is also associated with advanced disease than the intestinal type [23] and also a higher incidence of perineural invasion. Long-term survival after surgical treatment is reported as being significantly higher in patients with intestinal type than pancreatobiliary type [1,26-28].
It should be taken into account that the isolated histological analysis is subjective with considerable interobserver variability. Although morphologic definitions for typing ampullary are established, the presence of mixed forms often presents a challenge in the application of definitions. In addition, in cases of undifferentiated or poorly differentiated tumors, the distinction of the histological type may cause confusion [34]. Thus, to avoid bias in studies evaluating treatment and prognosis of ampullary carcinoma, a rigorous methodology should be established to control interobserver variability and to obtain reliable data, such as immunohistochemical evaluation.
Immunohistochemical analysis has potential utility in ampullary carcinoma classification as the different immunophenotypes. The ampullary tumors typically exhibit the same profile immunohistochemical markers of epithelial tissue which originated. Potentially useful markers to define intestinal versus pancreatobiliary differentiation are cytokeratin 7, cytokeratin 20, Mucin 1, Mucin 2 and CDX2.
Indeed, markers of intestinal and pancreatobiliary lineage individually have no ability to discriminate histological types of ampullary carcinomas, therefore combination immunohistochemical panels have been proposed for these types. The main and most panels used are described by Chang et al. [35] and Ang et al. [34].
Five markers (CDX2, MUC1, MUC2, CK7, and CK20) were evaluated in the panel proposed by Chang et al. However, only two markers (CDX2 and MUC1) were used in the histological classification and prognostic evaluation using three independent patient cohorts. In this study, pancreaticobiliary phenotype (defined to MUC1 and CDX2) was associated with a worse clinical outcome [35].
Ang et al. proposed a panel of four immunohistochemical markers (MUC1, CK20, CDX2 and MUC2) for evaluation of ampullary adenocarcinomas and they found that with this panel, confirmation of histological typing in most cases it was possible, especially in cases whose histology was mixed and poorly differentiated carcinomas. In this study did not evaluate the clinical behavior and development of these tumors, histological conducted only immunohistochemical and correlation [34].
For these reasons, the support immunohistochemistry for morphological classification of ampullary carcinoma is highly desirable, especially for tumors with lower differentiation. The combination of several markers panels are useful to better delineate these tumor cell line.
Conclusion
Differences in histolomorphological classifications make it difficult to evaluate and compare clinical studies of ampullary carcinomas. This fact, the histological division into two main types is necessary for therapeutic and prognostic comparison of this neoplasia. The immunohistochemical panels were then developed to establish the intestinal versus pancreatobiliary histological patterns in order to better stratify the ampullary adenocarcinomas and establish appropriate management protocols. We believe that the better characterization of the molecular mechanisms of different ampullary carcinoma phenotypes will provide not only a better understanding of this disease, but also the possibility of discovering new therapeutic targets.