Pham Nhu Hung1*, Nguyen Van Dan2, Nguyen Xuan Tuan2, Pham Van Tung2 and Nguyen Quang Tuan2
1Consultant of Cardiology and
Electrophysiology, Director of
Electrophysiology Laboratories, Hanoi
Heart Hospital, Vietnam
2Consultant of Cardiology, Hanoi Heart
Hospital, Vietnam
- *Corresponding Author:
- Pham Nhu Hung
Consultant of Cardiology and Electrophysiology,
Director of Electrophysiology Laboratories,
Hanoi Heart Hospital, Vietnam
Tel: 84913225648
E-mail: phamnhuhung@hotmail.com
Received: February 13, 2020; Accepted: March 13, 2020; Published: March 20, 2020
Citation: Hung PN, Dan NV, Tuan NX, Tung
PV, Tuan NQ (2020) Catheter Ablation of
Cardiac Arrhythmias in Pregnancy with
Limited Fluoroscopy. Interv Cardiol J Vol.6
No.1:89
Objective: This study sought to evaluate the feasibility and safety of catheter ablation in pregnancy with limited fluoroscopy.
Method: A case-control retrospective study.
Results: Ten patients with tachycardia in pregnancy (age 26, 30 ± 4, 52 years; gestational age 26, 90 ± 2, 88 weeks) successfully underwent radiofrequency catheter ablation procedures with limited fluoroscopy. Type of tachycardia consisted of 2 patients with atrial tachycardia; 2 patients with ventricular tachycardia; 4 patients with atrioventricular reentrant tachycardia; 2 patients with atrioventricular nodal reentrant tachycardia. Procedure time, fluoroscopy time, total dose area product were 66, 50 ± 19, 86 minutes; 118, 80 ± 64, 38 seconds; 0, 73 ± 0, 64 Gy-cm2 respectively. There were not any complications during and after procedures. All pregnancy normally delivered healthy babies.
Conclusion: Catheter ablation with limited fluoroscopy can be performed safely and with good outcomes in pregnancy.
Keywords
Tachycardia; Radiofrequency catheter ablation; Atrioventricular
reentrant tachycardia; Fluoroscopy time; Catheter ablation
Introducción
During pregnancy, the cardiovascular system is faced with
significant changes which can precipitate the occurrence of
arrhythmias. The hyperdynamic state and altered hormonal
status is possibly predisposing pregnant women to arrhythmias.
Cardiac arrhythmias during pregnancy pose a serious threat to
the health of both mother and fetus. Tachyarrhythmia, including
both supraventricular and ventricular tachycardia, is the most
common cardiac complication observed during pregnancy. The
paroxysmal supraventricular tachycardia during pregnancy is
the most frequently observed arrhythmias with an incidence
of 24 per 100,000 pregnancies [1]. The recurrence rates
during pregnancy in women with a history of supraventricular
tachycardia and ventricular tachycardia have been described in
50% and 27%, respectively [2]. Adverse fetal events occurred
in 20% [2]. Catheter ablation is the first choice and safety for
cardiac arrhythmias in patients without pregnancy. Some authors
suggested that pregnant women should not undergo an ablation
procedure because of the radiation risks to the fetus [3,4]. There
are very limited data available for the effects and safety of
catheter ablation in pregnancy. We investigate the feasibility and
safety of catheter ablation in pregnancy with limited fluoroscopy.
Patients and Methods
Patients
We studied 10 consecutive patients referred to Hanoi Heart
Hospital, Hanoi, Vietnam from September 2015 to August 2019
for tachycardia in pregnancy. All patients underwent catheter
ablation with limited fluoroscopy.
Study methods
A case-control retrospective study
Ablation Procedure
All patients were rolled around the abdomen with an X-ray
protective apron. In general, three catheters (4–6F) were
positioned at the right ventricular apex, His bundle region,
and right atrium using the femoral vein approach and the
coronary sinus using the left subclavian vein approach. In the electrophysiological study, it was done using standard protocols.
Heparin was used in all of the cases after the vein approach. During
all of the procedures, we tried to reduce fluoroscopy as much as
possible. X-ray was used only in the coronary sinus position and
across the aortic valve. The fluoroscopy was set at a minimum
of 3 frames/second. The non-fluoroscopic mapping system used
Ensite Velocity (St Jude Medical) during the entire procedure. An
ablation catheter (7F, 4-mm tip) was typically introduced using
the right femoral vein or artery approach. Mapping and ablation
were performed using established methods. The Radiofrequency
(RF) energy delivered was 30–50 W, and the temperature limit
was individually set to 50–70oC.
Follow up
The patients underwent follow-up by cardiologists in the hospital
outpatient clinic at least from post-procedure to delivery.
All of the pregnant women gave their permission for ablation and
accepted the possibility of using an X-ray if necessary. The study
protocol was approved by the Ethics Committee of the Hanoi
Heart Hospital.
Results
Ten patients with tachycardia in pregnancy underwent RF
catheter ablation. The mean age was 26, 30 ± 4, 52 years of
age (from 19 to 34 years old). The gestational age at the time
of ablation procedure was 26, 90 ± 2, 88 weeks of age (from 21
to 31 weeks old). All patients had no history of heart failure and
structural heart diseases. All patients had at least one tachycardia
during their pregnancies. Two of 10 patients had a history of
dysrhythmia before pregnancy. The characteristics of our studied
group present in Table 1.
| No |
Age |
Type of Tachycardia |
Gestational weeks |
Parity |
History of dysrhythmia |
LVDd (mm) |
LVEF (%) |
| Mean ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ SD |
26,30 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 4,52 |
|
26,40 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 2,71 |
|
|
44,70 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 5,07 |
68,10 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 7,43 |
| 1 |
27 |
AT |
31 |
1 |
No |
45 |
69 |
| 2 |
19 |
AT |
28 |
1 |
No |
49 |
52 |
| 3 |
34 |
VT |
26 |
3 |
No |
45 |
65 |
| 4 |
32 |
NSVT |
28 |
2 |
No |
43 |
76 |
| 5 |
21 |
WPW |
24 |
1 |
No |
51 |
68 |
| 6 |
25 |
AVRT |
21 |
1 |
No |
42 |
77 |
| 7 |
24 |
WPW |
27 |
1 |
No |
53 |
72 |
| 8 |
27 |
WPW |
25 |
2 |
Yes |
43 |
65 |
| 9 |
28 |
AVNRT |
26 |
1 |
No |
37 |
74 |
| 10 |
26 |
AVNRT |
28 |
1 |
Yes |
39 |
63 |
|
AT: Atrial Tachycardia; VT: Ventricular Tachycardia; NSVT: Non-Sustained Ventricular Tachycardia; WPW: Wolff-Parkinson-White Syndrome; AVRT: Atrioventricular Reentrant Tachycardia; AVNRT: Atrioventricular Nodal Reentrant Tachycardia; LVDD: Left Ventricular Diastolic Diameter; LVEF: Left Ventricular Ejection Fraction; SD: Standard Deviation |
Table 1 Baseline characters of the studied patients.
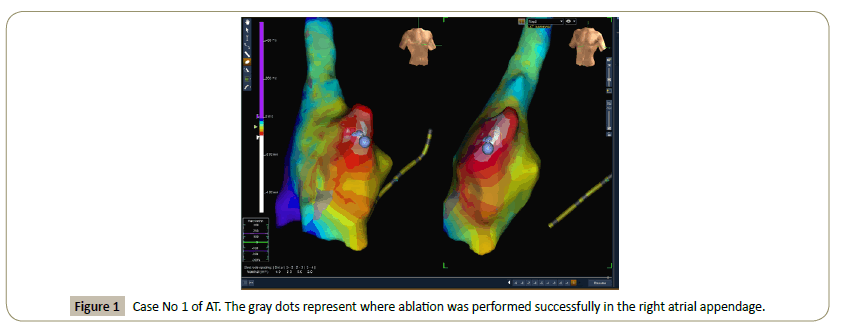
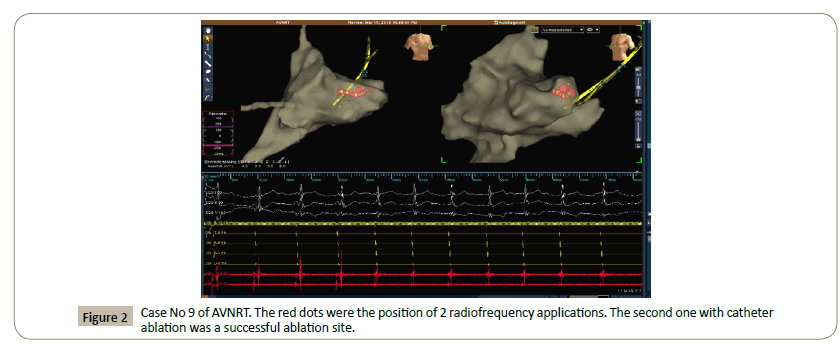
All patients were ablated successfully. In our studied group,
there were 2 patients with AT, 2 patients with VT, 4 patients with
AVRT, 2 patients with AVNRT. In 2 patients with AT, locations of
ablation were one of under right atrial appendage (Figure 1) and
one of the coronary sinus ostium. Both patients with VT, location
of ablation were right ventricular outflow tract. In 4 patients of
AVRT, locations of ablation were 2 of the left free wall accessory
pathway, one of the left septal accessory pathways and one of
the right posterior free wall accessory pathways. We ablated the slow pathway in 2 patients with AVNRT (Figure 2). The timing
of the procedure was 66, 50 ± 19, 86 minutes. The timing of
fluoroscopy was 118, 80 ± 64, 38 seconds. The total dose area
product was 0, 73 ± 0, 64 Gy-cm2). Data related to catheter
ablation procedures is presented in Table 2.
Figure 1: Case No 1 of AT. The gray dots represent where ablation was performed successfully in the right atrial appendage.
Figure 2: Case No 9 of AVNRT. The red dots were the position of 2 radiofrequency applications. The second one with catheter ablation was a successful ablation site.
| No |
Age |
Type of Tachycardia |
Location |
Procedure time (m) |
RF application |
fluoroscopy time (s) |
Total dose area product
(Gy-cm2) |
| Mean ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ SD |
26,30 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 4,52 |
|
|
66,50 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 19,86 |
|
118,80 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 64,38 |
0,73 ÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâñ 0,64 |
| 1 |
27 |
AT |
RAA |
100 |
8 |
144 |
1,05 |
| 2 |
19 |
AT |
CSO |
90 |
5 |
175 |
0,54 |
| 3 |
34 |
VT |
RVOT |
75 |
4 |
35 |
0,03 |
| 4 |
32 |
NSVT |
RVOT |
70 |
5 |
104 |
0,46 |
| 5 |
21 |
WPW |
LFW |
45 |
1 |
125 |
1,01 |
| 6 |
25 |
AVRT |
LFW |
40 |
1 |
204 |
1,93 |
| 7 |
24 |
WPW |
LS |
50 |
3 |
193 |
1,57 |
| 8 |
27 |
WPW |
RPFW |
80 |
12 |
132 |
0,54 |
| 9 |
28 |
AVNRT |
SP |
55 |
2 |
49 |
0,2 |
| 10 |
26 |
AVNRT |
SP |
60 |
3 |
27 |
0,02 |
|
RAP: Right Atrial Appendage; CSO: Coronary Sinus Ostium; RVOT: Right Ventricular Outflow Tract; LFW: Left Free Wall accessory pathway; LS: Left Septal accessory pathway; RPFW: Right Posterior Free Wall accessory pathway SP: Slow Pathway; M: minutes; S: seconds; SD: standard deviation |
Table 2 Data related to the catheter ablation procedure.
Patient’s outcome: There were not any complications during
and after procedures. All pregnancy normally delivered healthy
babies. Only one pregnancy needed cesarean surgery, but not
due to cardiovascular problems.
Discussion
The use of anti-arrhythmic drugs during pregnancy is challenging
due to potential fetal teratogenic effects. Moreover, many of the
currently available anti-arrhythmic drugs have arrhythmogenic
effects and could even increase mortality [5]. Although, the
anti-arrhythmic drugs sometimes could not terminate the
tachycardia episodes. It may cause hemodynamic deterioration
in both the fetus and the mother [6]. Nowadays, there are no
major studies guiding the selection of the safest and most
effective anti-arrhythmic drugs for pregnancy. The most popular anti-arrhythmic drugs use in practice to be beta-blockers and
calcium channel blockers. However, it is not recommended
because both of them are classified as category C by the US Food
and Drug Administration [7]. In fact, anti-arrhythmic drugs are
not warranted to assure during pregnancy and baby delivery.
Catheter ablation may be definitive therapy for these patients.
However, convention catheter ablation requires use fluoroscopy
and we do not control the fluoroscopy time during procedures.
Because of the potential risk for fetal, catheter ablation is not
strongly recommended in previous guidelines with class II b
(level of evidence C) for supraventricular tachycardia [8] and
with class II a (level of evidence B) for ventricular tachycardia [9].
Our study showed that the X-ray exposure was very low in the
non-fluoroscopic mapping age. Radiofrequency catheter ablation
using a non-fluoroscopic mapping system is feasible and with
limited radiation exposure in pregnancy. The more widespread
use of non-fluoroscopic mapping system, the radiation risks
for fetal may be reduced even further ionizing radiation will
not be required at all with supplementary modalities such as
intracardiac echocardiography to facilitate catheter navigation.
Up to now, the radiation exposure is not a reason to eliminate catheter ablation for pregnancy. Another reason to limit the
catheter ablation for pregnancy may play a role of challenges
performing pericardiocentesis and resuscitation in the event of
a complication [10]. However, the complication of pericardial
effusion and another complication in catheter ablation for
tachycardia (not atrial fibrillation) are very rare [11]. In literature,
mostly single cases of ablation during pregnancy [12-16]. In
almost all cases, indication for catheter ablation is due to severe
drug-resistant tachyarrhythmia. With an experienced operator,
we could do ablation in almost common tachycardia for
pregnancy with limited fluoroscopy. Our study also showed that
catheter ablation procedures produced safe and good outcomes
in pregnancy. The new ESC Guideline for supraventricular
tachycardia recommended flourless catheter ablation in cases of
drug-refractory or poorly tolerated supraventricular tachycardia
at the experienced centers with class II a [17].
In our daily practice, heparin was used in case of access to the
left side of the heart and for procedures of longer duration. In catheter ablation for pregnancy, we used prophylactic heparin for
all cases. Pregnancy is associated with a hypercoagulable status
and venous congestion [18]. During procedures, the patients
underwent catheter ablation which is known to increase the
thrombogenicity, and catheter movement through the femoral
vein might embolize the venous thrombosis. Therefore, prophylactic
heparin is strongly recommended to prevent thromboembolic
events in pregnancy undergoing catheter ablation.
Conclusion
Catheter ablation with limited fluoroscopy can be performed
in pregnancy with a high success rate. The catheter ablation
procedures produced safe and good outcomes in pregnancy.
Conflict of Interest
The authors declare that the research was conducted in the
absence of any commercial or financial relationships that be
construed as a potential conflict of interest.
References
- Li JM, Nguyen C, Joglar JA, Hamdan MH, Page RL, et al. (2008) Frequency and outcome of arrhythmias complicating admission during pregnancy: experience from a high-volume and ethnically-diverse obstetric service. Clin Cardiol 31:538-541.
- Silversides CK, Harris L, Haberer K, Sermer M, Colman JM, et al. (2006) Recurrence rates of arrhythmias during pregnancy in women with previous tachyarrhythmia and impact on fetal and neonatal outcomes. Am J Cardiol 97:1206-1212.
- Lindsay BD, Eichling Jo, Ambos HD, Cain ME (1992) Radiation exposure to patients and medical personnel during radiofrequency catheter ablation for supraventricular tachycardia. Am J Cardiol 70:218-223.
- Damilakis J, Theocharopoulos N, Perisinakis K, Manios E, Dimitriou P, et al. (2001) Conceptus radiation dose and risk from cardiac catheter ablation procedures. Circulation 104:893-897.
- Regitz-Zagrosek V, Lundqvist LC, Borghi C, Cifkova R, Ferreira R, et al. (2011) ESC Guidelines on the management of cardiovascular diseases during pregnancy: The task force on the management of cardiovascular diseases during pregnancy of the european society of cardiology (ESC). Eur Heart J 32:3147-3197.
- Sommerkamp SK, Gibson A (2012) Cardiovascular disasters in pregnancy. Emerg Med Clin North Am 30:949-959.
- Ghosh N, Luk A, Derzko D, Dorian P, Chow CM, et al. (2011) The acute treatment of maternal supraventricular tachycardias during pregnancy: A review of the literature. J Obstet Gynaecol Can 33:17-23.
- Page R, Joglar JA, Caldwell MA, Conti JB, Deal BJ, et al. (2016) 2015 ACC/AHA/HRS guideline for management of adult patients with supraventricular tachycardia. Heart Rhythm 13:e136-e221.
- Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, et al. (2018) 2017 AHA/ACC/HRS Guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation 138:e272-e391.
- Enriquez AD, Economy KE, Tedrow UB (2014) Comtemporary management of arrhthmias during pregnancy.Cir Arrhythm Electrophysiol 7:961-967.
- Bohnen M, Stevenson WG, Tedrow UB, Michaud GF, John RM, et al. (2011) Incidence and predictors of major complications from contemporary catheter ablation to treat cardiac arrhythmias. Heart Rhythm 8:1661-1666.
- Szumowski L, Szufladowicz E, Orczykowski M, Bodalski R, Derejko P, et al. (2010) Ablation of severe drug-resistant tachyarrhythmia during pregnancy. J Cardio-vasc Electrophysiol 21:877-882.
- Wu H, Ling LH, Lee G, Kistler PM (2012) Successful catheter ablation of incessant atrial tachycardia in pregnancy using three-dimension-al electroanatomical mapping with minimal radiation. Intern Med J 42:709-712.
- Kozluk E, Piatkowska A, Kiliszek M, Lodzinski P, Malkowska S, et al. (2017) Catheter ablation of cardiac arrrhythmias in pregnancy without fluoroscopy: A case control restrospective study. Adv Clin Exp Med 26:129-134.
- Omaygenc MO, Karaca IO, Guler E, Kizilirmak F, Cakal B, et al. (2015) Radiofrequency catheter ablation of supreventricular tachycardia in pregnancy: Ablation without fluoroscopic exposure. Heart Rhythm 12:1057-1061.
- Kaspar G, Sanam K, Gundlapalli S, Shah D (2018) Successful fluoroless radiofrequency catheter ablation of supraventricular tachycardia during pregnancy. Clin Case Rep 6:1334-1337.
- Brugada J, Katritsis DG, Arbelo E, Arribaset F, Bax JJ, et al. (2019) 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. European Heart Journal 41:655-720.
- James AH (2009) Venous thromboembolism in pregnancy. Arterioscler Thromb Vasc Biol 29:326-331.