Keyword
Catheter-induction; Coronary artery dissection; Contemporary practice; Percutaneous intervention
Introduction
Left main coronary artery dissection is a rare but devastating complication of selective coronary angiography or percutaneous intervention. Individual cases, their conservative, surgical or percutaneous management and immediate outcomes are not infrequently described in the literature [1-4]. The incidence of this complication in contemporary practice however is poorly documented and the evidence to support each of the management strategies is lacking. Consequently, when faced with an iatrogenic LMS dissection important management decisions are unlikely to be made in a clear and pre-determined fashion.
In this study we sought to determine the incidence of iatrogenic dissection in a single high volume interventional centre and to highlight any predisposing patient or procedural factors. In this centre the usual strategy for treating iatrogenic coronary artery dissection is by immediate PCI. All patients with LMS dissection were contacted in order to determine both immediate and longer-term outcomes following this strategy.
Methods
All catheter based procedures performed in our institution during eight years in succession were reviewed. For any case resulting in iatrogenic left main stem dissection angiographic films were reviewed, clinical and procedural details were documented and clinical notes were obtained. All patients were then contacted by telephone or clinic visit, except in the case of those deceased where information was obtained from both the clinical notes and responsible physician.
Statistical analysis
All results are expressed as mean or percentages. Chi-squared and students t-test was performed for comparison between groups. A P value of less than 0.05 was considered significant.
Results
During this 8-year period a total of 24,995 coronary procedures were performed: 18,976 diagnostic coronary angiograms and 6019 PCI.
Catheter-induced LM dissection occurred in 20 patients (0.08 % of all procedures). Of these, 16 events occurred during PCI representing 0.2% of all PCI procedures, and 4 during coronary angiography representing a 0.024% of all diagnostic procedures.
Patient data
Characteristics of the patients concerned and a comparison with the population of patients undergoing coronary procedures during the time period studied is given in Table 1.
| Parameters |
Patients with Iatrogenic dissection |
All patients undergoing procedures |
P |
| Patients (n) |
20 |
24,995 |
- |
| Age (years) |
72+/-9 |
67+/- 5 |
- |
| Male gender (%) |
60 |
75.1 |
NS |
| Diabetes (%) |
31 |
23.3 |
NS |
| Hypertension (%) |
49 |
54.55 |
NS |
| Dyslipidemia (%) |
15 |
12.28 |
NS |
| Smoker (%) |
50 |
43.25 |
NS |
| Family history (%) |
05 |
17.62 |
NS |
| PVD (%) |
05 |
8.28 |
NS |
| Renal failure (%) |
00 |
5.97 |
NS |
Table 1: Patient demographics
No specific patient characteristics were found to be significant risk factors for iatrogenic dissection.
Angiographic and procedural data
Significant LM stenosis (angiographic narrowing ≥50% at baseline) was present in 7/20 (35%) patients who subsequently had a dissection (Table 2A-C). The transracial approach (TRA) was used in 65% of cases with iatrogenic dissection compared with 68% of cases overall. As such, use of radial versus femoral access had no apparent bearing on the frequency of catheter induced LMS dissection. Dissection occurred more often in PCI with use of 6F guiding catheters than in angiography with 5F diagnostic catheters; however no specific shape of guiding catheter was implicated.
| Parameters |
Dissection Group |
Whole population |
P |
| Radial (%) |
65 |
67.8 |
NS |
| Femoral (%) |
35 |
32.2 |
NS |
| Pathological Left main artery |
35 |
NA |
- |
Table 2A: Angiographic Data
| EBU 3.5 6F |
9 |
| EBU 4 6F |
2 |
| EBU 5 6F |
1 |
| AL2 6F |
3 |
| AL1 6F |
1 |
| JL 3.5 5F |
3 |
| JL 4 5F |
1 |
Table 2B: Data of catheter induced LM dissection
| Patient |
Culprit vessel PCI |
Culprit catheter |
| 1 |
First marginal (Cx) |
AL2 6F |
| 2 |
Medial LAD |
EBU 3.5 6F |
| 3 |
Medial LAD |
AL2 6F |
| 4 |
Distal LM |
EBU 3.5 6F |
| 5 |
Proximal LAD |
EBU 3.5 6F |
| 6 |
LM |
EBU 4 6F |
| 7 |
LM |
EBU 3.5 6F |
| 8 |
Medial LAD |
EBU 5 6F |
| 9 |
Proximal Cx |
EBU 3.5 6F |
| 10 |
Distal LM |
EBU 3.5 6F |
| 11 |
Proximal LAD |
AL2 6F |
| 12 |
Proximal LM |
EBU 3.5 6F |
| 13 |
Medial LM |
EBU 4 6F |
| 14 |
Distal LAD |
AL1 6F |
| 15 |
Distal LAD |
EBU 3.5 6F |
| 16 |
Proximal LAD |
EBU 3.5 6F |
Table 2C: Data of involved vessel with PCI catheter induced LM dissection
Characteristics of dissection
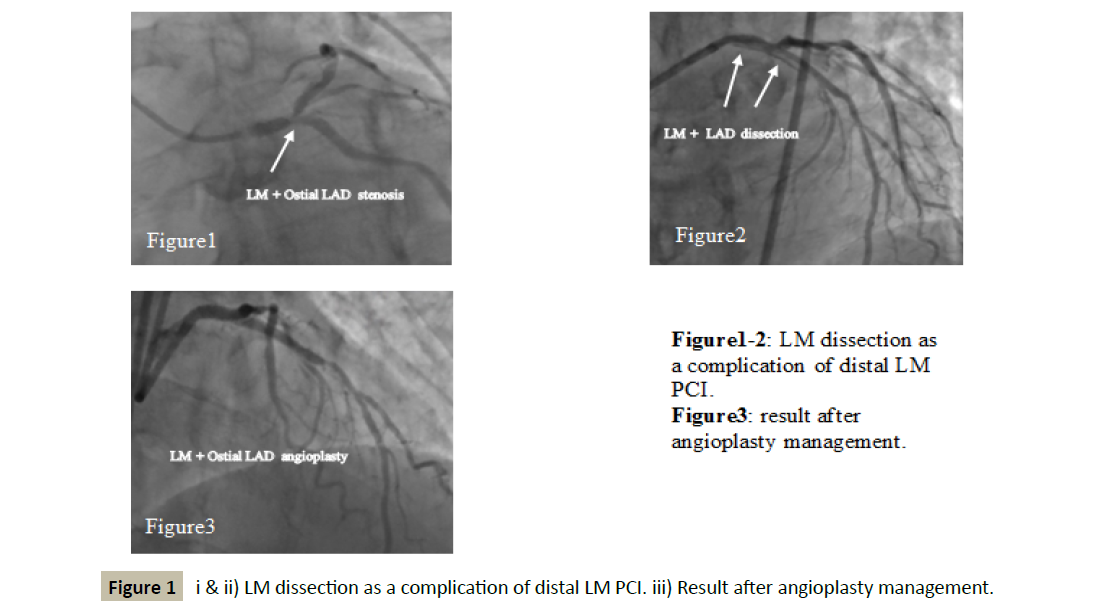
Rather than on initial canulation of the LMS, the majority of iatrogenic dissections occurred, or at least became apparent, later during the procedure (65%). LM dissection was occlusive in 5 patients (20%) and involved the distal LM in 70% of cases (Table 3 and Figure 1).
| |
% |
| Dissection with initial catheter Introduction |
35 |
| Dissection during procedure |
65 |
| Antegrade Dissection (fig 1-2) |
85 |
| Retrograde Dissection |
15 |
| Gp IIb/IIIa inhibitors used |
10 |
| Inotropes required |
55 |
| IABP support used |
45 |
| No hemodynamic support required |
45 |
| Distal LMS bifurcation treated |
80 |
| Provisional T stenting strategy |
80 |
| Final Kissing inflation |
80 |
| Final POT |
65 |
| Angiographic success |
90 |
Table 3: Details of complication and management strategy
Figure 1: i & ii) LM dissection as a complication of distal LM PCI. iii) Result after angioplasty management.
In 4 patients there was retrograde extension of the dissection to the aortic root; one of these patients died in-hospital (25%).
Management
All patients with iatrogenic LMS dissection in our centre during this time period were treated by immediate LMS PCI that is by DES implantation to the LMS.
With iatrogenic LM dissections during diagnostic angiography or at the start of a planned PCI the strategy was to immediately change the culprit catheter and proceed with wiring of both LAD and LCX branches. We performed LM PCI with a provisional T stenting strategy and used a final kissing inflation in 90% cases, whether or not a second (‘side branch’) stent was deployed. When the complication occurred during PCI we always proceeded with the same catheter and never tried to pull back the guiding catheter and proceeded with provisional T stenting. Intra-aortic balloon counter pulsation (IABP) was used only in thermodynamically unstable cases.
Angiographic success, that is normalized (TIMI III) flow in both branches and absence of significant (>30%) residual stenosis, was achieved in 90% (all but 2) patients.
One patient who died developed left main occlusive dissection with retrograde extension to aorta during diagnostic angiogram with a 5F amplatz catheter.
The second patient was an elderly female referred following ACS. The right coronary was small; the LM was heavily calcified and dissected following balloon predilatation. Further stent placement was impossible and the patient deteriorated rapidly and died in the cath lab.
Immediate hemodynamic compromise occurred in 11 patients (55%). In these cases, IABP and or inotropes were used whilst 45% patients required no hemodynamic support.
In-hospital outcome
Medium term outcome
At follow-up (range [6 to 40 months]), all 18 hospital survivors were alive with no new occurrence of either Q or non-Q wave MI. Repeat revascularization was required in 2/18 patients, in one patient CABG was undertaken at 6 months for restenoses of ostial LAD and circumflex with severe Aortic Stenosis, and in the other patient repeat PCI was performed at 6 months for restenosis of the LAD ostium.
Discussion
In this observation of contemporary practice, the rate of iatrogenic LMS dissection was low at 0.08% and the majority of patients were successfully managed by emergency PCI with DES without further adverse consequence during medium term follow-up.
Previous reports [5,6] have quoted an incidence of between 0.03 and 0.1% although these are estimates and not derived from systematic studies, they are consistent with our findings.
This low incidence suggests that on average a high-volume operator doing for example 400 invasive procedures per year is likely to face LMS dissection only once every 3 years. As such, to maintain a clear management strategy when faced with this emergency situation, and a hemodynamically unstable patient, (in at least half of all cases), is challenging.
The most effective management strategy for any serious procedural complication is of course to put all possible measures in place to avoid its occurrence
In our series, in such a small number of cases, when comparing to a cohort of 24,000 patients undergoing procedures, no specific patient risk factors could be identified. Moreover neither arterial access route nor guiding catheter could be held responsible. In a previously published report [6-11] RCA dissection seemed to be associated more frequently with use of the Amplatz Left guiding catheter although the cases in which a more supportive guide is chosen may of course be those already at higher risk. Specific guiding catheters have not previously been recognized in the literature concerning iatrogenic LMS dissection although an unusual location or anatomy of the LM that necessitates extensive catheter manipulation or deep engagement of guiding catheter may be associated [7,8].
That disease in the LMS prior to left coronary intubation is a risk factor seems intuitive and an association has previously been described [7,9]. Moreover one investigator reported that 90% of deaths associated with LM intervention were related to dissection, in 93% of which the catheter tip abutted the lesion on the first injection. [6,12]. The finding in our study that over 1/3 patients concerned had angiographic evidence of LMS disease strongly supports the hypothesis that patients with a diseased LMS must be considered at higher risk of iatrogenic dissection. The possibility that LMS plaque or calcification not demonstrated angiographically was a factor in our other patients cannot be ruled out.
As no modifiable patient or catheter factors can be identified in these cases emphasis must remain on avoidable operator errors. Contrast injection against an occlusive or ventricularized pressure is usually implicated in coronary artery dissection and must be avoided by close attention whether using hand or automated injecting systems. Other technical errors include forceful manipulation of the guiding catheter and proceeding with intervention passing wires, balloons and stents via a nonco- axial guide.
When LMS dissection does occur, according to the results described here, emergency PCI with DES is an effective management strategy and avoids delays associated with transfer and preparation for emergency surgery. In order to treat the LMS percutaneous in a manner that will be immediately safe and maintained in the long term, a certain amount of operator and team experience are required. In our centre, all operators are experienced in LMS intervention. While we feel that immediate PCI is the fastest technique to restore coronary artery patency, the first experiences of an operator in LMS PCI should not be in an emergency situation. As such in centres where LMS PCI is not routinely performed an effective alternative strategy for rapid transfer to surgery or another catheter laboratory should be predetermined.
Whilst the principles of stent deployment in the LMS are not different from that of intervention in more distal bifurcation lesions it has been demonstrated that close attention to stent sizing, stent apposition (Kissing and POT) and coverage of the LMS osmium is essential to minimize the serious consequences of LMS restenosis or stent thrombosis. Even in the emergency situation, once the patient has been stabilized, these considerations must not be forgotten. Regarding the distal LMS bifurcation, in this centre a provisional side-branch T-stenting strategy followed by proximal optimization technique (POT) was used. This strategy is associated with a low rate of major adverse cardiac events in follow-up. Moreover in the context of a dissection, the deployment in the first instance of a single stent from the LMS to the main vessel is practical in gaining rapid control of the coronary circulation, providing a guide wire is maintained in the second branch. More complex two stenting strategies may delay immediate rectification of the problem.
A further important consideration in any centre that doesn’t electively treat LMS disease is the availability of drug-eluting stents of the appropriate sizes. The availability of a coronary intensive care unit for post-procedural management with an intra-aortic balloon pump in-situ is clearly essential and the support of an experienced anaesthetist is valuable [13].
Conclusion
Catheter-induced left main coronary artery dissections are rare. The overall incidence was less than 1 in 1000 for coronary procedures and 2 in 1000 for PCI. No modifiable risk factors can be determined and thus to minimize occurrence, care with contrast injection and catheter manipulation remain the most important strategies. In experienced centres this complication can be safely and effectively managed in the catheter laboratory with immediate LMS PCI and appropriate hemodynamic support. We have shown that PCI with DES in this situation has an acceptable immediate and sustained outcome. Comparative trials are unlikely to be undertaken but in this setting PCI seems to be a satisfactory alternative to emergency surgery. In any centre undertaking coronary angiography or PCI a management strategy should be pre-determined such that the protocol is clear on the rare occasion that an operator is faced with this emergency situation.
References
- Mulvhill NT, Marco B, Fajadet J, Marco J (2003) Catheter induced left main dissection: A treatment dilemma. Cath Cardiovasc Intervent 58: 214-216.
- Wykrzykowaska JJ, Carrozza J, Laham RJ (2006) Aortocoronary dissection with left main artery occlusion: successful treatment with emergent stenting. J Inv Cardiol 18: E217-20.
- Goldstein JA, Casserly IP, Katsiyiannis WT, Lasala JM, Taniuchi M (2003) Aortocoronary dissection complicating a percutaneous intervention. J Inv Cardiol 15: 89-92.
- Boyle AJ, Chan M, Dib J, Resar J (2006) Catheter-Induced Coronary artery dissection: Risk factors, Prevention and management. J Invasive Cardiol 18: 500-503.
- Cameron J (2000) Left main coronary artery dissection during coronary angioplasty or angiography treated by stent insertion without requirement for emergency bypass graft surgery. Aust NZ Med 20: 726-728.
- Lee SW, Hong MK, Kim YH, Park JH, Rheeet KS, et al. (2004) Bail-out stenting for left main coronary artery dissection during catheter-based procedures: acute and long-term results. Clin cardiol 27: 393-395.
- Devlin G, Lazzam L, Schwartz L (1997) Mortality related to diagnostic cardiac catheteriztion. Int J Cardiovasc Imaging 13: 379-384.
- Slack JD, Pinkerton CA, Van Tassel JW, Orr CM (1986) Left main artery dissection during percutaneous coronary angioplasty. Catheter Cardiovasc Diag 12: 255-260.
- Kovac JD, De Bono DP (1996) Cardiac catheter complications related to left main stem disease. Heart 76: 76-78.
- Dunning DW, Kahn JK, Hawkins ET, O’Neill WW (2000) Iatrogenic coronary artery dissections extending into and involving the aortic root. Cath Cardiovasc Intervent 51: 387-393.
- Delvin GD, Lazzam L, Schwartz L (1997) Mortality related to diagnostic cardiac catheterization. Int J cardiac Imaging13: 379-384.
- Pavei A, Marco J (2010) Tools & techniques: choice and use of guiding catheters. EuroIntervention 6: 543-544.
- Yiangou AA, Panayiotis CA, Tereza A, Stasinos T, Chrisostomos M, et al (2016) Iatrogenic left main coronary artery dissection: mind the catheter tip. Cardiovascular Medicine 19: 264-271.