- (2008) Volume 9, Issue 3
Mehmet Fatih Yuzbasioglu1, Mesut Ozkaya2, Erman Cakal3, Mustafa Goksu1
Departments of 1General Surgery and 2Endocrinology and Metabolism, Faculty of Medicine,
Kahramanmaras Sutcuimam University. Kahramanmaras, Turkey
3Department of Endocrinology and Metabolism, Yuksek Ihtisas Hospital. Ankara, Turkey
Received December 25th, 2007 - Accepted April 4th, 2008
Folic Acid; Homocysteine; Pancreatitis, Acute Necrotizing; Vitamin B 12
Homocysteine is a sulphur-containing amino acid which plays a major role in the metabolism of methionine and folate [1]. Elevated plasma homocysteine concentrations have been correlated with the development of arterial thrombosis and atherosclerosis and have now been recognized as an independent risk factor for atherosclerosis in the coronary, cerebral and peripheral vasculature [2]. Some researchers suggest that there is a relationship between pancreatitis and homocystinuria, possibly being secondary to occlusive vascular disease of the pancreas [3]. High homocysteine levels may be the cause of acute pancreatitis with endothelial dysfunction and impaired microvascular circulation. Pancreatic microvascular perfusion failure may be a primary reason for clinical and experimental acute pancreatitis [4, 5].
We aimed to analyze the homocysteine status in patients with acute pancreatitis and the changes of the plasma homocysteine level at the acute phase of acute pancreatitis and after hospital discharge.
Methods
Fourteen patients with acute pancreatitis who had been admitted to Kahramanmaras Sutcu Imam University, Research Hospital, Kahramanmaras, Turkey (mean age 60.3±12.2 years, range 45-84 years; male/female ratio 5/9; BMI 31.9±3.6 kg/m2) were enrolled in this study. The control group consisted of 14 healthy subjects (mean age 59.8±4.9 years, range 53-70 years; male/female ratio 4/10, BMI 30.4±3.2 kg/m2; P=0.888, P=1.000, and P=0.249 vs. acute pancreatitis patients for age, gender and BMI, respectively). The diagnosis of acute pancreatitis was based on the typical clinical signs of abdominal pain, vomiting or nausea, serum amylase of more than 3 times the upper reference limit, and/or positive ultrasonography or computed tomography scan. The severity of acute pancreatitis according to the Atlanta criteria was mild in all patients. After detailed physical examination, blood was taken within 24 hours from admission to the hospital in order to evaluate plasma homocysteine and serum vitamin B12, folate, amylase, lipase, C-reactive protein (CRP), total, HDL and LDL cholesterol, triglycerides, blood urea nitrogen (BUN), white blood cells (WBC) and creatinine. The results of the clinical laboratory measurements were obtained from patient records. Vitamin B12 and folic acid levels were assessed in order to exclude cases of vitamin deficiency. All parameters were measured again at least six months after discharge from hospital.
Creatinine clearance was calculated using the Cockroft and Gault formula: creatinine clearance (mL/min) = (140 - age (year) ) x weight (kg) / (0.81 x serum creatinine (μmol/L) ). For women this value was multiplied by 0.85. In the literature, this formula has been shown to have a significant correlation to the glomerular filtration rate [6, 7]. Serum folate and vitamin B12 were measured by radioassay. Total homocysteine concentrations were determined in EDTA plasma by high performance liquid chromatography. Immediate plasma seperation was carried out after blood sampling, and the plasma was kept at 4°C.
Ethics
Informed consent was obtained from both the patients and the control subjects and the ethical committee of the hospital approved the blood sampling.
Statistics
The results were expressed as means, standard deviations and ranges. Two-tailed P values less than 0.05 were considered statistically significant. All data were entered into and processed by the SPSS 11 for Windows statistical package. Differences between acute pancreatitis patients and the control subjects were analyzed using the unpaired t test and the Fisher’s exact test (gender distribution). The differences between the acute phase and the follow-up values were analyzed by using the paired t test.
The results are shown in Table 1. The plasma levels of homocysteine were significantly higher in acute pancreatitis patients than in healthy subjects while no significant differences were detected in vitamin B12 and folate. There were no significant differences in serum total, HDL, and LDL cholesterol concentrations between the two groups of subjects while trygliceride, BUN and WBC counts were significantly higher in acute pancreatitis patients. Moreover, the acute pancreatitis patients had serum creatinine levels significantly higher than the control subjects. The creatinine clearance was also impaired in these patients but it did not reach statistical significance. Finally, amylase, lipase, and CRP were significantly higher in acute pancreatitis patients than in control subjects.
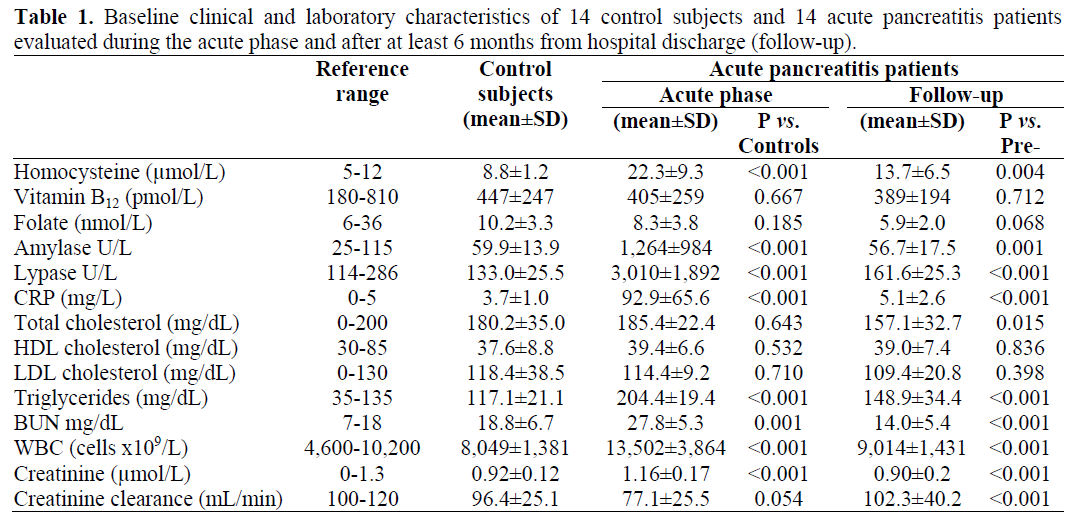
In the follow-up period of the acute pancreatitis patients, a significant reduction of plasma homocysteine and serum creatinine as well as a significant increase in cretinine clearance, were observed. A reduction of folate was also observed, but it did not reach statistical significance. In this period, a significant reduction of serum amylase, lipase, CRP, total cholesterol, triglyceride, BUN and WBC also occurred.
Acute pancreatitis is an inflammatory disease associated with autodigestion of the pancreas due to intrapancreatic activation and the release of digestive enzymes, but there is increasing evidence that pancreatic ischemia plays an important role in this disease. Pancreatic microvascular perfusion failure may be a reason for clinical [8, 9, 10] and experimental acute pancreatitis [4, 5]. Reduction in the pancreatic circulation aggravates pancreatic damage in the course of acute pancreatitis [5]. It is well-known that a disturbance of pancreatic microcirculation leads to the formation of thrombi in capillaries, the activation of leukocytes, the release of proteolytic enzymes and the formation of oxygen-derived free radicals and proinflammatory cytokines.
Makins et al. suggest that there is a relationship between pancreatitis and homocystinuria, possibly being secondary to occlusive vascular disease of the pancreas [11]. High homocysteine levels may be a cause of acute pancreatitis with endothelial dysfunction and impaired microvascular circulation. In addition, it may lead to complications as Sircar et al. [12] report cardigenic shock due to acute pancreatitis after hyperhomocysteinemia
In our study, we found that the plasma homocysteine level was increased in patients with acute pancreatitis as compared to normal controls. The hyperhomocysteinemia was probably due to disturbed methylation. A relationship between hyperhomocysteinemia and acute pancreatitis has not been studied previously. However, Sundeep Batra suggested that homocystinuria is an uncommon metabolic cause of pancreatitis, and pancreatitis is an unusual manifestation of homocystinuria [13]. Mark Lowenheim (commenting in the above-mentioned paper) suggested that pancreatic disease in homocystinuria is preventable and that recurrent disease is amenable to therapy which reduces homocysteine concentrations. They would recommend that homocysteine concentrations be included in the metabolic workup of chronic relapsing pancreatitis [13]. We agree with Lowenheim in suggesting that, in acute pancreatitis, recurrent acute pancreatitis may be related to hyperhomocysteinemia in the presence of normal folate and vitamin B12 levels.
Another explanation for high homocysteine levels was insufficient renal function. The healthy kidney plays a major role in homocysteine clearance and metabolism, as it does with other amino acids. Hyperhomocysteinemia in renal disease is related to reduced plasma homocysteine clearance. The underlying cause of this reduction is unknown but involves a defect in renal and/or extrarenal clearance [14]. In our study, BUN and serum creatinine values were significantly higher in acute pancreatitis patients than in the control group. Plasma homocysteine levels in acute pancreatitis subjects increased with a decrease in creatinine clearance when compared to the control subjects; a decrease in plasma homocysteine and an increase in creatine clearance were also found during the follow-up of these patients. The inverse relationship between homocysteine levels and the glomerular filtration rate is related to reduced renal function suggesting that increased plasma homocysteine levels may be useful as a marker of decreased glomerular filtration rate when assessing high risk patients.
Lien et al. observed a close relationship between total plasma homocysteine and serum creatinine in iatrogenic hypothyroidism [15]. They found a progressive and parallel increase in total homocysteine and serum creatinine in hypothyroidism. Homocysteine and serum creatinine responses were explained by the hypodynamic circulation and renal failure in hypothyroidism. And acute pancreatitis also decreases the glomerular filtration rate as in hypothyroidism, which is related to serum creatinine, but also closely associated with plasma homocysteine.
We observed higher plasma homocysteine and lower creatinine clearance (although not significant) in acute pancreatitis patients as compared to healthy subjects. After acute pancreatitis therapy, homocysteine levels decreased and creatinine clearance increased significantly. In conclusion, a decreased glomerular filtration rate in acute pancreatitis is related to decreased renal homocysteine clearance.
This study shows that plasma homocysteine is significantly increased in patients with acute pancreatitis and a decreased (although not significant) creatinine clearance was found in these patients. This is the first report showing that patients with acute pancreatitis have higher plasma homocysteine levels than healthy subjects. Moreover, our data show a significant reduction in plasma homocysteine levels after a 6-month follow-up of acute pancreatitis patients. additional research is needed to better understand the effect of homocysteine levels in acute pancreatitis
The authors have no potential conflicts of interest