- (2014) Volume 15, Issue 4
Natalya B Gubergrits1, Aleksandr Zubov2, Oksana Golubova1, Pavel Fomenko1, Nadezhda Byelyayeva1
1Department of Internal Medicine, Donetsk National Medical University, Donetsk, Ukraine
2Donetsk Regional Clinical Territorial Medical Union, Donetsk, Ukraine
Received May 12th, 2014 – Accepted June 24th, 2014
Context Article analyzes current data on macroamylasemia and splenosis, their etiology and diagnostics in particular. Case Report Authors presented their own clinical observation of a young woman who was diagnosed to have macroamylasemia on the background of splenosis due to the splenectomy after blunt abdominal injury. Conclusion This is the first time such a combination of macroamylasemia on the background of splenosis has been described in the literature.
Hyperamylasemia; Pancreatitis, Chronic; Splenectomy; Splenosis
MA: macroamylase; MAE: macroamylasemia
Macroamylasemia (MAE) arises due to the enzymatically active macro-molecular amylase complexes in blood flow. Large size of these complexes precludes their excretion by the kidneys and provokes their retention in blood. It’s proved by the increased amylase activity in blood and decreased activity of this enzyme in urine [1].
Macroamylase (MA) is represented by large molecules with molecular weight ranging from 150,000 to 2,000,000 (molecular weight of normal human amylase is equal to 50,000-55,000) [2].
Macroamylase can be the complex of normal serum amylase with serum proteins or carbohydrates upon MAE [1]. Upon MAE, amylase in blood is more frequently bound with such substances as high molecular weight proteins - particularly, immunoglobulin A and, rarely, immunoglobulin G [1].
Splenosis is a posttraumatic focal ("nodular") implantation of splenic tissue, occurring more frequently in the abdominal cavity [3].
Both states are rare ones, their combination not being described in the literature.
In June 2012, 21 years old woman was directed to the clinic of internal medicine of Medical University hospital for more precise diagnosis. At the moment of visit she had no complaints.
Considers herself a patient for 2-3 years, when the aching pain in the right hypochondrium emerged after the intake of fatty, fried foods.
Examination revealed a slight decrease in hemoglobin level to 11.7 g/dL (norm 12.0-16.0 g/dL), increase in platelet level to 366×103/mm3 (norm 180-320×103/mm3), increased activity of blood amylase to 147.1 U/L (norm 3.6-100.0 U/L).
Re-examination in 3 months revealed IgG antibodies to CMV and EBV-NA. In July 2011, ultrasound detected isoechogenic formation 1.96×1.72 cm in size, with smooth, clear circuits, close to the splenic parenchyma by its structure, in the projection of bed of the rejected spleen.
In July 2011, spiral CT of abdomen and retroperitoneum with preliminary per os contrast (Figure 1) showed softtissue formation with clear, irregular circuits 3.6×2.0 cm in size in the projection of bed of the rejected spleen; rounded soft-tissue formations, with smooth, clear circuits, up to 0.9-1.3 cm in size were detected parasagittally in abdomen, under the anterior abdominal wall at the level of L2-L4. Conclusion: formations in abdomen of abovedescribed localization may appear due to the enlarged lymph nodes? Remaining slices of the rejected spleen? CT with intravenous bolus enhancement is recommended in order to exclude neoplastic genesis.
Lymphadenopathy has been marked since the age of 4. At the age of 7 a laparotomy, splenectomy concerning blunt abdominal injury (fall from a height), traumatic splenic rupture, intraperitoneal bleeding was performed.
In blood analysis: platelets - 348×103/mm3, amylase - 144.6 U/L, pancreatic amylase - 21.30 U/L (norm 13.0-53.0 U/L), lipase - 28.60 U/L (norm 0.0-60.0 U/L).
Urine α-amylase - 60.10 U/L (norm 0.0-460.0 U/L).
Viral markers: anti-CMV of IgG class- 24.2 U/ml (norm <3.0 U/ml), antibodies of IgG class to nuclear AG EBV-NA - 57.8 U/ml (norm <3.0 U/ml), DNA EBV in blood - found (++).
Antibodies to toxoplasma of IgM class - not found, class IgG - 3.2 IU/ml (norm <10 IU/ml), DNA of toxoplasma - not found. Antibodies of IgG class to toxocara, to antigens of Trichinella, to antigens of Opisthorchis, to antigens of Echinococcus - not found.
HIV-test - negative.
Tumor markers: CA 19-9, CA 125 - within the normal range.
Ig A, M, G levels in the blood serum - within the normal range.
Ultrasound diagnostics (Figure 2a, b): no free fluid in the abdominal cavity and pleural sinuses. Liver: total size (left and right lobe) - not increased, smooth circuit, capsule is not thickened, no signs of hepatoomentopexy, total echogenicity - normal, no focal changes. Portal vein - 0.9 cm in diameter, blood velocity 24.0-30.0 cm/s, hepatopetal undulating blood flow. Hepatic artery: blood velocity - to 80.0 cm/s, low-resistant type of blood flow. Induration of the round ligament of the liver with the presence of effect of distal attenuation from it, without signs of recanalization. Gall bladder - common anatomical location, form, circuit, volume; wall - not thickened. Choledochus - 0.3 cm in diameter. No concrements. Pancreas - no liquid collectors in the projection of omental bursa, total volume is not increased, smooth circuit, echogenicity is slightly increased, in the projection of the cervix - body not dilated Wirsung’s duct is visualized (0.2 cm in diameter). Spleen - rejected. Closer to the anterior abdominal wall, near the border of the parietal peritoneum - 3 solid rounded formations, transversely located in the epigastrium, at the distance of up to 2.0 cm apart from each other, hypoechoic, with a smooth circuit, homogeneous structure, upon energy mapping at the "noise" border - with single loci of blood flow, moderately movable during instrumental palpation, movable upon respiratory excursion. Kidneys, adrenal glands - without visible pathological changes.
Submandibular and parotid salivary glands on the left and right are uniformly increased in volume, including retroauricular portion. Thickened capsule, parenchyma - inhomogeneous, with slightly increased echogenicity, lobed, with minor linear echo-positive inclusions. No focal changes in the parenchyma. Excretory ducts are visualized without evidence of sialolithiasis and dilatation. Relative dilatation of outlet veins. Upon EC - vascularization closer to the increased one. Tumor formations - not detected. Near the left angle of the mandible - a single lymph node 1.6×0.8 cm with a smooth circuit and relative violation of differentiation of cortex medulla (echo-signs of lymphadenitis). Other groups of lymph nodes - within the normal range.
Multislice CT of the abdomen, retroperitoneum with intravenous bolus enhancement: liver - diffusely enlarged, with smooth, clear contours, homogeneous structure, additional formations and foci of pathological density are not visualized in it. Size of the pancreas is not changed, homogeneous structure, additional formations are not found. Rounded formation with a homogeneous structure, clear and smooth contours of 2.1 cm in diameter (probably, additional slice) is detected in the bed of the rejected spleen. Adrenal glands are of normal shape, size, structure, without any additional formations. Kidneys are of normal shape, size, position, without any additional formations. Cavity systems are not expanded, concrements are not visualized. Vascular pedicles of the kidneys - without changes. The ureters are not dilated. In the abdominal cavity, directly under the anterior abdominal wall, 1.0- 4.0 cm above the navel - 4 rounded formations of 1.1-1.6 cm in diameter; their size, number and structure have not changed substantially in comparison with the previous examination on July 27, 2011. Soft-tissue formation with rather clear, smooth circuits of 2.7×2.1 cm in size is detected in the abdomen, under the right lobe of the liver. Above-described formations moderately uniformly accumulate contrast agent. Lymph nodes in the abdomen and retroperitoneum are not increased. In the parametrial tissue on the left - single lymph nodes thickened up to 0.9 cm in diameter. No destructive changes in the bone structures at the level of examination.
Conclusion: nodular formations in the abdominal cavity without clear organ accessory, the nature of which is not fully understood currently. Additional slice of spleen. Diffuse changes in the liver.
Formations require differentiation between lymphoid, neoplastic or another process and ectopic splenic parenchyma.
Considering normal activity of blood P-isoamylase upon increased index of blood α-amylase, we concluded that the increase in the latter was due to S-isoamylase. This made us to consult a dentist.
Consultation of dentist: no data on the presence of inflammatory and neoplastic diseases in the maxillofacial area and oral cavity. Lymph nodes are enlarged, painless, of normal consistency. Treatment is not required.
Taking into account anamnesis, data of laboratory and instrumental examination, formations detected in the abdominal cavity are not associated with toxocariasis or echinococcosis. EBV-infection, stage of persistence. It’s recommended to repeat CT in 3-6 months. Hemogram monitoring.
Present rounded formations under the anterior abdominal wall have not grown for one year (according to CT). However, determining their nature is possible only after a biopsy of formations (if possible - puncture one). It’s necessary to conduct a testing for viral infections, urine inoculation of flora. Absolute norm in the peripheral blood (occasionally eosinophilia). DNA EBV in blood (++), antibodies of IgG class to nuclear antigen EBV and CMV are detected in the patient. Treatment by virucide 500 mg 2 times a day for 14 days, then 500 mg for 7 days is prescribed. Re-examination of DNA EBV after 2 months of therapy.
No data confirming the fact of malignant character of formations in abdominal cavity. More likely, they are not tumors at all.
Puncture biopsy of formation in the abdominal cavity: splenic tissue in the biopsy material.
Cam/Ccr ratio: 0.6% (norm 1‒4%).
Precipitation of blood amylase activity by PEG 6000 is performed. Precipitation of 87% of amylase activity is detected (norm - up to 73%)
Considering the steady increase in indices of blood α-amylase upon normal activity of urine α-amylase and blood lipase, reduction of Cam/Ccr ratio, increased results of precipitation of amylase activity by PEG 6000, we’ve already diagnosed MAE in the step II of the algorithm by J. E. Berk (1995) [1].
Clinical Diagnosis: MAE. EBV-infection, stage of persistence. Splenosis.
Recommendations: observation (1 ultrasound diagnostics in a half a year).
The fact that MA usually represents amylaseimmunoglobulin complex formed by the reaction of ‘antigen-antibody’ is proved by detection of this complex upon various autoimmune diseases and diseases accompanied with malabsorption: celiac disease [4], systemic lupus erythematosus [5], rheumatoid arthritis [6], as well as AIDS [7], and other infections [8]. There are cases of MAE in pregnant women [9], healthy children and children with frequent episodes of acute respiratory diseases [10]. MAE can occur upon various diseases which are based on the inflammatory process, e.g. acute appendicitis [11].
MA complexes can be formed in the presence of abnormal proteins in blood connected with amylase, e.g. upon multiple myeloma, myeloid leukemia [12]. MAE can be combined with the presence of other macroenzymes in blood [13-15].
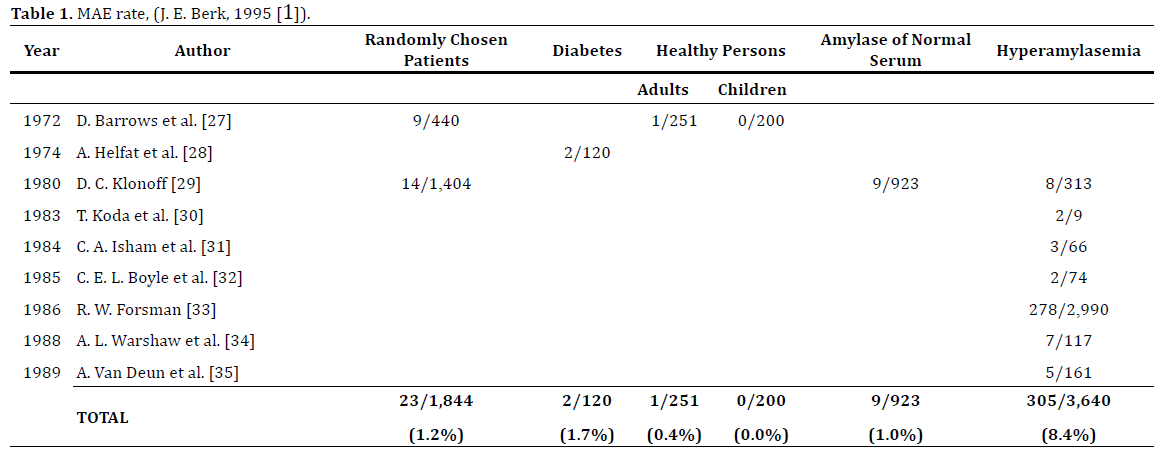
Rate of MAE is not studied thoroughly, as special identifying researches were not conducted. Published fragmentary information is presented in Table 1.
We did not find any description of the clinical observations of MAE combined with splenosis in the literature. In this regard, the following clinical case, in our opinion, seems to be rather interesting.
Descriptions of the ectopic spleen and splenosis are extremely rare ones in the modern literature. Role of these states is not sufficiently studied from the clinical and morphofunctional points of view.
Splenosis is more often localized in the parietal and visceral peritoneum, as a fragment of splenic tissue in the bed of a remote organ, as well as in the retroperitoneal space and in the extra-abdominal one - in the pleural cavity, pericardium, and postoperative scar and even in the meninges [16, 17, 18, 19, 20]. The rate of posttraumatic splenosis makes up to 67% after open splenectomy [21] and to 80% after laparoscopic one [22]. Purposeful autotransplantation of splenic tissue is one of the splenosis variants used to prevent postsplenectomy syndrome, the effectiveness of which is so far under discussion [23].
Unlike accessory spleen, splenosis is being developed due to destruction of the splenic pulp with its dissemination. In some cases this can lead to septic complications such as necrosis, abscess formation, and bleeding upon traumatic injury. Both upon the accessory spleen and upon splenosis there’s a need to differentiate them from tumors of the abdominal cavity with high-tech methods of research, but publications of clinical observations of these states in the literature are single. Ultrasonography does not have quite high sensitivity - up to 68% [24]. Scintigraphy with labeled red blood cells has better sensitivity. This method also gives a possibility to estimate the functional activity of residual foci of splenic tissue after splenectomy [25].
Considering the inaccessibility of radionuclide diagnostic method, ultrasound and laparoscopy remain the main methods of detection of splenosis, which can be supplemented by CT and magnetic resonance tomography for the differential diagnostics of tumors of the abdominal cavity. Studying the morphofunctional state of accessory spleen confirms that it has all the basic structural elements of the main spleen and produces all its functions.
It is hard to estimate the pathogenetic correlation between MAE and splenosis, as both states are not studied well. Splenectomy is known to cause the immunodeficiency; therefore patients should receive the pneumococcal conjugate vaccine (Prevnar), Hib vaccine, and the meningococcal vaccine. An increase in blood leukocytes can occur following a splenectomy. The postsplenectomy platelet count may rise to abnormally high levels (thrombocytosis), leading to an increased risk of potentially fatal clot formation [26]. Our patient does not have leukocytosis, and platelets level in the blood is only slightly increased. It is probably connected exactly with splenosis. Ectopic splenic tissue is likely to partially take over the function of the rejected spleen. Splenectomy may have contributed to the developing persistence of EBVinfection in the patient.
Although MAE may be caused by the binding of α-amylase with immunoglobulins or atypical proteins, Ig G, A, M levels in the patients’ blood serum are within the normal range. It can be assumed that the MA formation is caused by low-intensity inflammatory process (persistence of EBVinfection). However, all this is suggestions. Combination of MAE and splenosis in patient may be coincidental. Clinical observation without active treatment actions seems to be the most rational approach in this case.
Clinical significance of our study is that doctors should consider the MAE possibility in patients with asymptomatic increased α-amylase levels in the blood, as well as the probability of splenosis in patients who underwent splenectomy, with ambiguous voluminous formations mainly in the abdominal cavity, i.e. in patients after splenectomy attention should be paid not only to the state of immunity, peripheral blood indices, but also to the ultrasound and CT results with their correct interpretation.
In conclusion, it should be pointed out that the awareness of doctors on MAE and variants of splenic ectopy gives a chance in cases, being accidental discovery, to prevent unnecessary examinations and surgical interventions.
The authors state no conflict of interest.