Keywords
Hair and skin infection; Dermatophytes; Non dermatophytic; Moulds
Introduction
Fungi are responsible for three distinct kinds of infections: superficial mycoses, subcutaneous and deep ones [1]. Fungal infections constitute a major health problem all over the world. Dermatomycoses constitute a group of superficial fungal infections of the keratinised tissues, viz; the epidermis, hair and nails. Superficial mycoses are the fungal infections exclusively invading the integumentary tissue, parasitizing the horny layer of the skin and other structures rich in keratin, like hair and nails, leading to a dermal inflammatory response with intense itching. Signs and symptoms induced by various dermatophytic and non-dermatophytic infections are clinically indistinguishable from each other. Identification and characterization of fungus by in vitro culture is warranted for proper diagnosis, treatment and understanding of epidemiological characteristics of a region [2]. The aim of our study was to identify the clinical presentation and mycological etiology of skin and hair infections in patients attending the dermatology clinics in a tertiary level hospital in New Delhi.
Materials and Methods
Study design
The study was conducted over a period of 9 months (April 2013-December 2013) on 100 consecutive patients referred from dermatology outpatients to Mycology laboratory of a tertiary care hospital, New Delhi, with clinical suspicion of superficial fungal infection of hair and skin. The study was approved by the Institutional Review Board.
Clinical identification and sampling technique
A superficial fungal infection of hair and skin was suspected when a lesion had central clearing, with advancing, red, scaly, elevated border, with or without vesicles on the border of the affected area. Tinea corporis was suspected when there was a circular plaque with demarcated border and T. cruris was suspected when there was an erythematous plaque in the groin area, often bilateral with pruritis. Tinea pedis was suspected when there were white macerated areas in the webs, and chronic, dry, scaly hyperkeratosis of the sole and heel. Tinea manuum was suspected when there was erythema, mild scaling with dorsum involved appearing in the palm as chronic, dry, scaly hyperkeratosis [3]. The clinically samples like plucked hair, skin scrapings, skin biopsy, and skin scales were collected from the suspected sites. Nail samples were not included in our study.
Microbiological processing of the samples
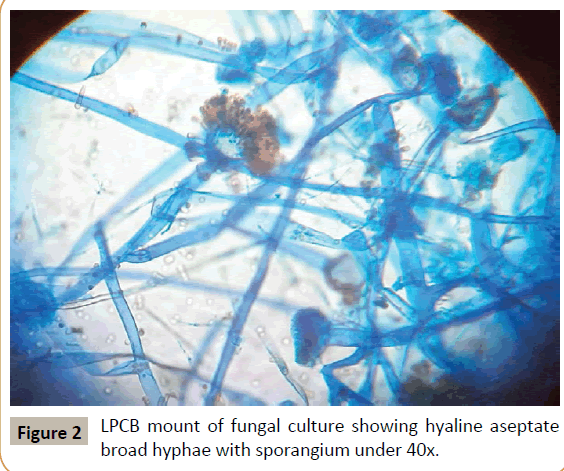
The collected samples were sent to the laboratory in sterile petri dishes. The sample was divided into two parts. From the first part 10-20% potassium hydroxide (KOH) mount was made and direct microscopy was done. The KOH wet mounts were screened under low power (x10) and then at high power (x40) for visualization of the fungal hyphae, spores and yeasts cells (Figure 1). The second part of the sample was inoculated onto two sets of Sabourauds dextrose agar (SDA), one with 0.05 mg/ml chloramphenicol and another with 0.5 mg/ml of cycloheximide along with 0.05 mg/ml chloramphenicol and incubated at 25 and 37°C. The cultures were examined twice a week, they were declared negative if no growth was obtained till 4 weeks. The culture isolates were identified by studying the colony morphology, microscopic examination of the lactophenol cotton blue (LPCB) mounts (Figure 2) and slide culture (wherever necessary).
Criteria for identification of the pathogenic fungus
Candida species were considered as the primary pathogen on isolation as a single pure growth along with a direct microscopy result showing yeast cells with or without pseudomycelia. Candida spp. were considered as secondary pathogens if they were isolated with dermatophytes or non-dermatophytic pathogenic molds [4,5]. Non-dermatophyte molds were considered significant if there was a positive KOH finding and they were isolated repeatedly (more than twice) in pure culture. Whereas all other NDM cases were considered to be contaminants. Those samples that yielded 3 or more growths and were negative in KOH mount were considered contaminants/mixed growth.
Limitations
Our study was conducted on the patients attending outpatient clinic, and it was difficult for us to collect data about the working history of the patients whether they were involved in household or outdoor activity. Also very few patients turned up to the laboratory with their own collected samples and hence was difficult to see and take an image of the actual clinical picture of the skin and hair.
Results
Out of the 100 patients, the infection was seen to be more common in males (66%) as compared to females (34%) with a male: female ratio of 1.9:1. The infection was predominant in <10 years of age (30%) and least common in >60 years (3%) of age (Table 1).
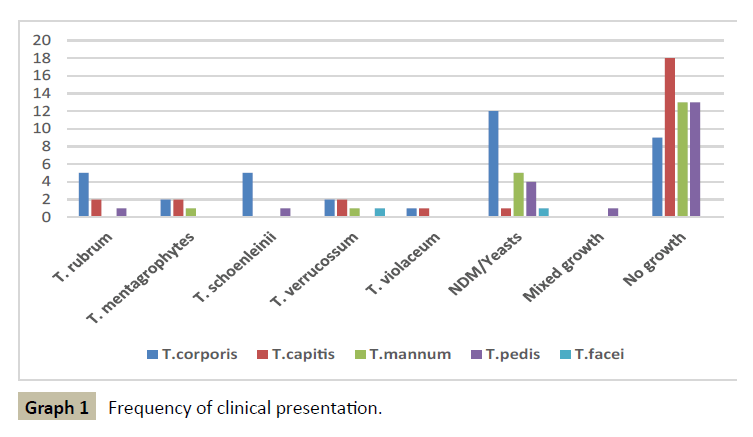
The clinical profile of the patients showed that, Tinea corporis(32%) was the commonest presentation, followed by T. capitis (26%), T. mannum (20%), T. pedis (20%) and T. faciei (2%) was the least common presentation (Table2 and Graph 1).

Figure 1 :KOH mount of the skin scrapping showing hyaline septate fungal hyphae at 40x.
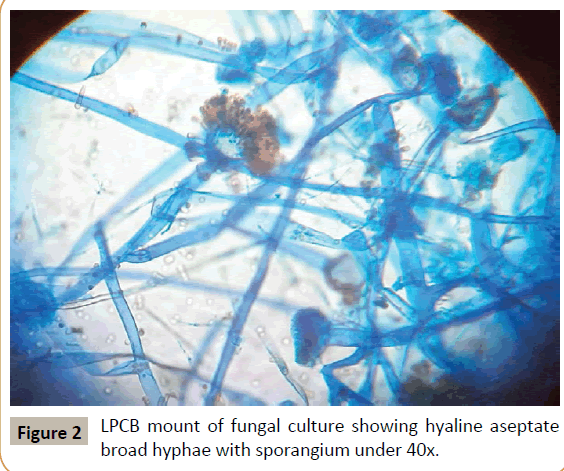
Figure 2:LPCB mount of fungal culture showing hyaline aseptate broad hyphae with sporangium under 40x.
The age-sex distribution of the patients with different clinical presentation is shown in the Table 3. Most of the patients belonged to 0-10 years of age (30%). Followed by 31-40 (22%) years of age. T. corporis was the most common clinical presentation in males (25%) followed by T. capitis in females (15%). T. faceie was the least common presentation in both males and females (1%).
Of the 100 suspected cases of superficial fungal infection, 37% were positive by direct microscopy by KOH mount, 46% were positive by culture and 27% were positive by both microscopy and culture. Out of the 46 culture positive cases, 42% had single isolates as growth and only 4% had growth of 2 organisms and contaminants (>3 types of growth) were grown in only one of the tubes (Table 4).
| Age |
Male |
Female |
Total n (%) |
| 0-10 |
12 |
18 |
30 (30%) |
| 11-20 |
9 |
6 |
15 (15%) |
| 21-30 |
15 |
2 |
17 (17%) |
| 31-40 |
18 |
2 |
20 (20%) |
| 41-50 |
6 |
4 |
10 (10%) |
| 51-60 |
3 |
2 |
5 (5%) |
| >60 |
3 |
0 |
3 (3%) |
| Total |
66 (66%) |
34 (34%) |
100 |
Table 1: Age and sex distribution of the patients.
Out of all the culture positive cases, 27 (24.5%) grew dermatophytes and 17 (16.5%) had a growth of non-dermatophyte moulds (NDMs) with only 6 (5.8%) growing yeasts. In skin samples the most common isolates were Trichophyton rubrum and Trichophyton schoenleinii (8.1% each) followed by Candida albicans (CA), Non albicans Candida (NAC) and Aspergillus flavus (4% each). While in hair samples, most common dermatophytes were T. rubrum and T. verrucossum (7.1% each). Alternaria alternata (3.5%) was the only NDM isolated from hair samples. Amongst the dermatophytes, T. rubrum was the commonest isolate (7.8%). The other dermatophytes isolated were T. verrucossum (5.8%), T. schoenleinii (5.8%), T. mentagrophyte (3.9%) and T. violaceum (1.9%). While, amongst the NDMs, Aspergillus flavus (2.9%) was commonly isolated. The other NDMs that were isolated were, A. terreus, A. fumigatus, A. niger, Penicillium spp., Syncephalastrum spp., Paecillomyces spp., Mucor spp. Rhizopus spp. and Epicoccum spp. Amongst the yeasts, both C albicans and Non albicans Candida (NAC) were isolated in equal numbers (2.9%) (Table 5).
Discussion
In our 100 cases of superficial fungal infection, the infection was seen to be more common in males (66%) as compared to females (34%). The male predominance might be due to increased outdoor activity leading to increased perspiration and hence the increased predisposition in these cases. The infection was more common in children <10 years of age. This might be due to their being involved in a lot of outdoor games leading to perspiration and might also be due to lack of hygienic awareness amongst the children. While, in two studies conducted by Lakshmanan et al. [3] in 2015, in Tamil Nadu and Prabhu et al. [6] in 2013 in Coastal Karnataka, the superficial fungal infection was more common in 30-45 years of age which is the second most common age group in our study.
| Clinical pattern |
No. of sample (%) |
T. rubrum |
T. mentagrophyte |
T. schoenleinii |
T. verrucossum |
T. violaceum |
NDM/Yeasts |
Mixed |
No growth |
| T. corporis |
32 (32%) |
5 |
2 |
5 |
2 |
1 |
12 |
0 |
9 |
| T. capitis |
26 (26%) |
2 |
2 |
0 |
2 |
1 |
1 |
0 |
18 |
| T. mannum |
20 (20%) |
0 |
1 |
0 |
1 |
0 |
5 |
0 |
13 |
| T. pedis |
20 (20%) |
1 |
0 |
1 |
0 |
0 |
4 |
1 |
13 |
| T. facei |
2 (2%) |
0 |
0 |
0 |
1 |
0 |
1 |
0 |
0 |
| TOTAL |
100 |
8 |
5 |
6 |
6 |
2 |
23 |
1 |
53 |
Table 2 Etiological profile of the clinical presentations.
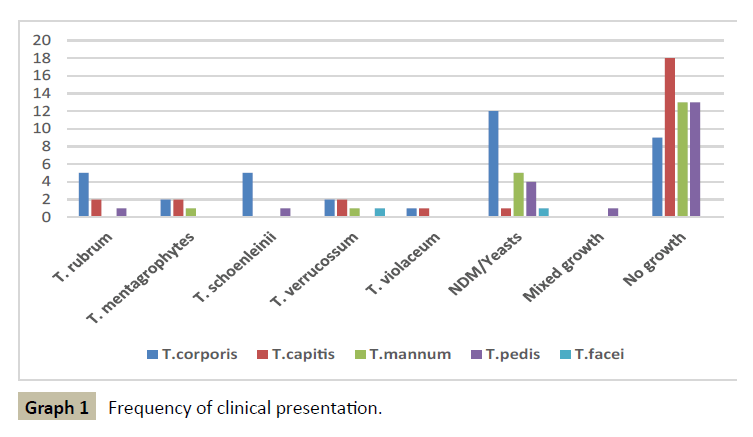
Graph 1 :Frequency of clinical presentation.
| Clinical Presentation |
Sex distribution |
Age Distribution in years |
| 0-10 |
11-20 |
21-30 |
31-40 |
41-50 |
51-60 |
>60 |
Total |
| T. corporis |
Male |
0 |
2 |
5 |
11 |
3 |
2 |
2 |
25 |
| Female |
0 |
2 |
3 |
1 |
1 |
1 |
0 |
8 |
| T. capitis |
Male |
9 |
0 |
0 |
0 |
1 |
0 |
0 |
10 |
| Female |
14 |
1 |
0 |
0 |
0 |
0 |
0 |
15 |
| T. mannum |
Male |
1 |
2 |
3 |
6 |
1 |
1 |
0 |
14 |
| Female |
4 |
0 |
0 |
0 |
1 |
1 |
0 |
6 |
| T. pedis |
Male |
2 |
4 |
6 |
4 |
1 |
0 |
0 |
17 |
| Female |
0 |
2 |
0 |
0 |
1 |
0 |
0 |
3 |
| T. facei |
Male |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
1 |
| Female |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
1 |
| TOTAL |
100 |
30 |
13 |
17 |
22 |
10 |
5 |
3 |
100 |
Table 3:Age and sex distribution of different clinical presentation.
| No. of samples |
KOH+ |
KOH- |
Both KOH+, Culture+ |
Culture+ (n=46) |
Culture- |
Mixed growth |
| Single growth |
Double growth |
| 100 |
37 |
63 |
27 |
42 |
4 |
53 |
1 |
| Percentage |
37% |
63% |
27% |
42% |
4% |
53% |
1% |
Table 4 Microscopy and culture profile.
| |
Organisms |
Skin (n=72) |
Hair (n=28) |
Total |
NDM(16.5%) & Yeasts
(5.8%) |
A. niger |
2 (2.7%) |
- |
(1.9%) |
| A. terreus |
1 (1.3%) |
- |
1 (0.9%) |
| A. flavus |
3 (4%) |
- |
- (2.9%)
|
| A. fumigatus |
2 (2.7%) |
- |
2 (1.9%) |
| Penicillium spp. |
1 (1.3%) |
- |
1 (0.9%) |
| Paecillomyces spp. |
1 (1.3%) |
- |
1 (0.9%) |
| Mucor spp. |
2 (2.7%) |
- |
2 (1.9%) |
| Syncephalstrum spp. |
2 (2.7%) |
- |
2 (1.9%) |
| Rhizopus spp. |
1 (1.3%) |
- |
1 (0.9%) |
| Epicoccum spp. |
1 (1.3%) |
- |
1 (0.9%) |
| A. alternata |
- |
1 (3.5%) |
1 (0.9%) |
| C. albicans |
3 (4%) |
- |
3 (2.9%) |
| NAC |
3 (4%) |
- |
3 (2.9%) |
Dermatophytes
24.5% |
T. mentagrophyte |
2 (2.7%) |
3 (10%) |
4 (3.9%) |
| T. rubrum |
6 (8.1%) |
2 (7.1%) |
8 (7.8%) |
| T. schoenleinii |
6 (8.1%) |
- |
6 (5.8%) |
| T. verrucosum |
4 (5.4%) |
2 (7.1%) |
6 (5.8%) |
| T. violaceum |
1 (1.3%) |
1 (3.5%) |
2 (1.9%) |
| Negative |
- |
33 (44.5%) |
20 (71.4%) |
53 (51.9%) |
| >3 Growths |
- |
1 (1.3%) |
- |
1 (0.9%) |
| Total |
- |
75 |
28 |
103 |
Table 5 Distribution of different isolates from the clinical samples.
In the current study, Tinea corporis (32%) was the commonest clinical presentation, followed by T. capitis (26%), T. mannum (20%), T. pedis (20%) and T. faciei (2%). Studies conducted by Lakshmanan et al. [3] in Tamil Nadu, Mishra et al. [1] in Odisha et al. [7] in North Carolina, USA have also found T. corporis to be the commonest clinical presentation. However, these studies observed T. pedis to be the least common clinical presentation, compared to our study where T. faciei was the least common presentation. The age and sex distribution of the clinical presentation in our study showed that the most common clinical presentation was T. corporis (25%) in males followed by T. capitis in females (15%). The least common presentation was T. facei in both males and females (1%). In a study conducted by Al Shimaa et al. [8] in Egypt in 2015, T capitis was the most common presentation mostly seen amongst the males (65.5%). The least common in their study was T. cruris commonly seen in females (52.2%).
37% cases were positive by direct microscopy by KOH mount, 46% were positive by culture and 27% were positive by both microscopy and culture. However, Lakshmanan et al. [3] found 160 (50.5%) of their cases to be confirmed by KOH microscopic examination which was more than what was seen in our study, and 82 (27%) were both KOH and culture positive, similar to our study. While in another study [6] in 2013 from Coastal Karnataka, India, 100% cases of superficial fungal infection were positive by KOH microscopy and 72.9% were positive by culture, whereas, the study done in 2002 in Amritsar, India, reported that 59.2% isolates were positive on direct microscopy and 50.4% were positive on culture [9].
Amongst our culture positive cases, there was maximum occurrence of dermatophytes 27 (24.5%), followed by NDMs 17 (16.5%) and only 6 (5.8%) yeasts. In a study in Tamil Nadu, India in 2015, dermatophytosis was seen to be in 75.6% (62/82) and non-dermatophytosis in 24.4% (20/82) [3]. The infection rate by the NDMs has been seen to show an increasing trend as found in studies conducted in Odisha in 1998 and in 2000 in North Carolina, USA, which was also evidenced in our study [1,7].
Amongst the dermatophytes, Trichophyton rubrum was the commonest isolate (7.8%) followed by T. verrucossum (5.8%), T. schoenleinii (5.8%), T. mentagrophyte (3.9%) and T. violaceum (1.9%). In another two studies in India in 2015 and 2010, T. rubrum was the commonest dermatophyte isolated, similar to our study [3,10]. However in a study conducted by Agharmirian et al. in Iran [11], Epidermophyton floccosum was the commonest dermatophyte isolated, while M. canis was most commonly isolated in the studies conducted by Fortuño et al. [12] in Spain and Mangiaterra et al. [13] in Argentina. However Weitzman et al. [14] commonly isolated T. tonsurans in the United States and Nowicki et al. [15] in Poland and Abu-Elteen et al. [16] in Jordan observed T. mentagrophytes as their common dermatophyte.
In our study, 22.3% non-dermatophytes were isolated. Amongst them, the most common isolates were NAC, C.albicans and A. flavus (2.9% each). The other NDMs that were isolated were, A. terreus, A. fumigatus, A. niger, Penicillium spp., Syncephalastrum spp., Paecillomyces spp., Mucor spp., Rhizopus spp. and Epicoccum spp. Also in a study conducted by Lakshmanan et al. [3], the percentage of non-dermatophytic fungus isolated was 24.4%, similar to our study. The commonest non-dermatophytes isolated in their study were Candida spp. (60%) followed by Aspergillus spp. (20%) Alternaria spp. (10%), Curvularia spp. (5%) and Fusarium spp. (5%) While, Grover et al. [17] in North eastern part of India, have isolated 34% of non-dermatophytes in their study, a higher percentage than detected in our study. In their study on onychomycosis, Veer et al. [18] in Aurangabad, Maharashtra have isolated Scopulariopsis spp. (16.66%), Alternaria spp. (16.66%), Fusarium spp. and Curvularia spp. (8.3%) each. Sarma et al. [19] in New Delhi had isolated Curvularia lunata, Penicillium spp., Alternaria alternata and Geotrichum candidum (1 each, 10%). While a study group in Shimla in 2007 had found Aspergillus spp. (6.1%) to be the most common NDM isolates. Other NDMs isolated in their study were Acremonium spp., Fusarium spp., Scopulariopsis spp., Curvularia spp. and P. marneffei [20].
We have isolated NDMs like Syncephalastru spp., Epicoccum spp. and Paecillomyces spp. causing superficial infection of hair and skin in our patients. On review of literature it was seen that Syncephalastrum spp. has been known to cause dermatomycoses and onychomycoses and rarely pulmonary and CNS infections. Paecillomyces spp. is normally considered a contaminant but occasionally causes cutaneous, pulmonary infections and sinusitis. While Epicoccum spp. has usually been seen to be associated with skin allergies.
To the best of our knowledge this is the first Indian study to report these species in the causation of these infections. However, the limitation of our study was that it was conducted on the patients attending outpatient clinic and hence it was difficult to do follow up studies to look for the post therapeutic effect.
Conclusion
We found an increasing predilection of males in superficial fungal infection of hair and skin, with T. corporis (32%) being the commonest presentation. Dermatophytes (24.5%) were the most common pathogens followed closely by the NDMs (16.5%) confirming an increasing trend of infection by the same. The importance of microscopy and culture is highlighted and it is stressed upon to understand and manage the locally prevalent fungi involved in the causation of disease and their control, helping in decreasing the drug resistance and morbid outcomes.
References
- Mishra M, Mishra S, Singh PC, Mishra BC (1998) Clinico-mycological profile of superficial mycoses. Indian J Dermatol Venereol Leprol 64: 283-285.
- Yehia MA, El-Ammawi TS, Al-Mazidi KM, Abu El-Ela MA, Al-Ajmi HS (2010) The spectrum of fungal infections with a special reference to dermatophytoses in the capital area of Kuwait during 2000-2005: A retrospective analysis. Mycopathologia 169: 241-246.
- Lakshmanan A, Ganesh KP, Raam MS, Hemamalini M, Madhavan R (2015) Epidemiological and clinical pattern of dermatomycoses in rural India. Indian J Med Microbiol 33: S134-S136.
- Daniel CR, Gupta AK, Daniel MP, Sullivan S (1998) Candida infection of the nail: Role of Candida as a primary or secondary pathogen. Int J Dermatol 37: 904-907.
- Gupta AK, Ryder JE, Summerbell RC (2002) The diagnosis of non-dermatophyte mold onychomycosis. Int J Dermatol 41: 647-651.
- Prabhu SR, Shetty VH, Shetty NJ, Girish PN, Rao BPK, et al. (2013) Clinico-mycological study of superficial fungal infections in Coastal Karnataka, India. J Evol Med Den Sci 2: 863886-863846.
- Goldstein AO, Smith KM, Ives TJ, Goldstein B (2000) Mycotic infection. Effective management of condition involving skin, hair and nails. Geriatrics 55: 40-42.
- Al Shimaa M, Elmegeed A, Ouf SA, Moussa TAA, Eltahlawi SMR (2015) Dermatophytes and other associated fungi in patients attending to some hospitals in Egypt. Braz J Microbiol 46: 799-805.
- Aggarwal A, Arora U, Khanna S (2002) Clinical and mycological study of superficial mycoses in Amritsar. Indian J Dermatol 47: 218-220.
- Patel P, Mulla S, Patel D, Shrimali G (2010) A study of superficial mycosis in south Gujarat region. Natl J Commun Med 1: 85-88.
- Agharmirian MR, Ghiasian SA (2008) Dermatophytoses in outpatients attending the dermatology center of Avicenna hospital in Qazvin, Iran. Mycoses 51: 155-160.
- Fortuño B, Torres L, Simal E, Seoane A, Uriel JA, et al. (1997) Dermatophytes isolated in our clinics. 5-year-study in Zaragoza. Enferm Infecc Microbiol Clin 15: 536-539.
- Mangiaterra ML, Giusiano GE, Alonso JM, Pons de SL, Waisman R (1998) Dermatophytosis in the greater Resistencia area, Chaco Province, Argentina. Rev Argent Microbiol 30: 79-83.
- Weitzman I, Chin NX, Kunjukunju N, Della-Latta P (1998) A survey of dermatophytes isolated from human patients in the United States from 1993 to 1995. J Am Acad Dermatol 39: 255-261.
- Nowicki R (1996) Dermatophytoses in the Gdansk area, Poland: A 12-year survey. Mycoses 39: 399-402.
- Abu-Elteen KH, Abdul MM (1999) Prevalence of dermatophytoses in the Zarqa district of Jordan. Mycopathologia 145: 137-142.
- Grover S, Roy P (2003) Clinico-mycological profile of superficial mycosis in a hospital in North-East India. MJAFI 59: 114-116.
- Veer P, Patwardhan NS, Damle AS (2007) Study of onychomycosis: Prevailing fungi and pattern of infection. Indian J Med Microbiol 25: 53-56.
- Sarma S, Capoor MR, Deb M, Ramesh V, Aggarwal P (2008) Epidemiologic and clinicomycologic profile of onychomycosis from North India. Int J of Dermatol 47: 584-587.
- Gupta M, Sharma NL, Kanga AK, Mahajan VK, et al. (2007) Onychomycosis: Clinico-mycologic study of 130 patients from Himachal Pradesh, India. Indian J Dermatol Venereol Leprol 2007: 389-392.