- (2008) Volume 9, Issue 4
Mehrdad Nikfarjam1, Niraj J Gusani1, Eric T Kimchi1, Rickhesvar P Mahraj2, Kevin F Staveley-O’Carroll1
Departments of 1Surgery and 2Radiology, Penn State Milton S. Hershey Medical Center, Penn State College of Medicine. Hershey, PA, USA
Received February 5th, 2008 - Accepted May 6th, 2008
Context Nephrectomy and pancreaticoduodenctomy are operations often performed for the treatment of malignancy. However, the combination of both procedures is rarely reported. Objectives The indications and outcomes of combined right nephrectomy and pancreaticoduodenectomy were assessed. Study design Patients were identified from a prospective operative database between 2002 and 2008. Setting A tertiary care center. Patients One-hundred and 80 patients undergoing pancreaticoduodenectomy. There were 5 (2.8%) patients treated by combined right nephrectomy and pancreaticoduodenal resection. Main outcome measure Description of these 5 patients. Results Three patients had retroperitoneal sarcomas adherent to the right kidney and duodenum, one patient had a locally advanced transitional-cell carcinoma and the remaining patient presented with an ampullary malignancy and concurrent right renal tumor All patients underwent en bloc resection with clear margins. Median operating time was 13 hours (range: 9-21 hours). There was no perioperative mortality in this series.Complications were noted in 3 (60%) patients related to pancreaticoduodenal resection and all were managed conservatively without significant clinical impact. Median postoperative hospital stay was 8 days (range: 7- 11 days). At a median follow-up of 14 months (range: 3-36 months) all patients were alive without evidence of disease recurrence. Conclusion En bloc right nephrectomy combined with pancreaticoduodenal resection can be performed in selected patients with malignant tumors with acceptable morbidity to achieve clear resection margins.
Kidney; Nephrectomy; Pancreas; Pancreatic Neoplasms; Pancreaticoduodenectomy; Sarcoma
Nephrectomy is indicated for the treatment of localized renal cell carcinoma and uroepithelial malignancies. Pancreaticoduodenectomy is the treatment of choice for periampullary cancers. The indication for the combination of both procedures is not welldefined. As far as is known, there have been no previous series reporting on patients treated by combined right nephrectomy and pancreaticoduodenal resection. Most of the information on this combined procedure is confined to isolated case reports [1, 2].
We report on a series of patients undergoing en bloc right nephrectomy and pancreaticoduodenectomy. The indications for surgery, the surgical approach, and outcomes of the patients undergoing this combined procedure are described.
Patients
One-hundred and 80 patients undergoing pancreatic resection at Milton S. Hershey Medical Center between January 2002 and December 2007 were identified from a prospectively maintained operative database. Combined right nephrectomy and pancreaticoduodenal resection was performed in 5 patients (2.8%).
Operative details, indications for combined resection, the length of procedure, blood loss, complications and outcomes were analyzed.
All patients underwent complete work-up for evidence of metastatic disease by computed tomography (CT) of the chest, abdomen and pelvis. Tumors were considered potentially locally resectable if there was no evidence of major vessel encasement. All patients in this series were well functioning and considered fit for major surgery. Abdominal pain was the most common presenting symptom.
En bloc resection of the right kidney, pancreas, and duodenum was performed to minimize the risk of tumor disruption, with the aim of obtaining a negative surgical margin when tumors involved both the periampullary and right perinephric regions. Following a midline laparotomy, mobilization of the right kidney from lateral to medial was performed as the initial step. The renal vessels were identified posteriorly, followed by ligation and division. The adrenal gland was separated from the kidney and retained, if possible, when resection margins were not being compromised. Otherwise the right adrenal gland was mobilized along with the kidney and vessels. In cases where there was tumor extension inferiorly to involve the right colon, the root of the small bowel mesentery was completely mobilized and a right hemicolectomy performed. Otherwise following division of the right renal vessels, further dissection was carried anterior to the vena cava, until the left renal vein was completely exposed, to achieve full kocherization of the duodenum.
Pancreaticoduodenectomy was performed in all cases in a conventional manner [3]. This involved ligation of the gastroduodenal artery, division of the distal bile duct followed by exposure of the portal vein. The proximal jejunum was divided and its mesenteric vessels transected close to the intestinal wall. The neck of pancreas was divided anterior to the portal-superior mesenteric vein confluence, clear of macroscopic tumor, followed by division of uncinate process adjacent to the superior mesenteric artery, allowing the specimen to be removed.
Reconstruction following pancreaticoduodenal resection proceeded in a standard manner as previously described [3]. An end-to-side pancreaticojejunal duct-to-mucosa anastomosis was constructed. This was followed by a single layer biliary anastomosis and a two layered duodenojejunal or gastrojejunal anastomosis. Abdominal drains were placed adjacent to the biliary and pancreatic anastomoses. Complications were defined according to previously defined criteria [3, 4].
All patients were managed in a surgical intensive care unit (SICU) for 24 hours post operatively unless more prolonged monitoring was subsequently indicated. Nasogastric tubes were inserted at the time of operation and removed at day 1 postoperatively. A liquid diet was commenced day 2 post operatively and progressed to a soft diet. Drain fluid amylase measurements were performed after day 5 post operatively. Octreotide was not administered prophylactically in this series. Erythromycin was commenced at day 2 post operatively at 200 mg intravenously 8 hourly for prevention of delayed gastric emptying. No patients in this series had operative feeding jejunostomy tubes inserted as they were not considered malnourished preoperatively. Patients not tolerating a diet by day 7 post operatively, but otherwise clinically well, were considered to have delayed gastric emptying. They were commenced on total parenteral nutrition and discharged home or to a rehabilitation facility with outpatient follow-up.
Consent was obtained for each patient for possible combined resection including nephrectomy and pancreaticoduodenectomy. Review of charts was performed with institutional review committee approval. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki.
Frequencies, median, and range were used as descriptive statistics.
Details of the 5 patients who underwent combined right nephrectomy and pancreaticoduodenal resection during the study period are shown in Table 1. There were 3 male and 2 female patients. The median age at the time of surgery was 67 years (range: 56-84 years). Primary retroperitoneal sarcoma was the most common tumor treated, occurring in three patients. One patient had a locally advanced transitional cell carcinoma, with surrounding inflammatory changes and the remaining had an ampullary adenocarcinoma coexisting with a renal oncocytoma. On imaging, retroperitoneal sarcomas were adherent to kidney and duodenum/pancreas, without direct tumor infiltration of these organs (Figure 1). Nephrectomy and pancreaticoduodenal resection was considered necessary to ensure clear resection margins. Similarly, in a case of transitional cell carcinoma, adherence to the duodenal wall rather than direct infiltration necessitated en bloc resection to achieve tumor clearance.
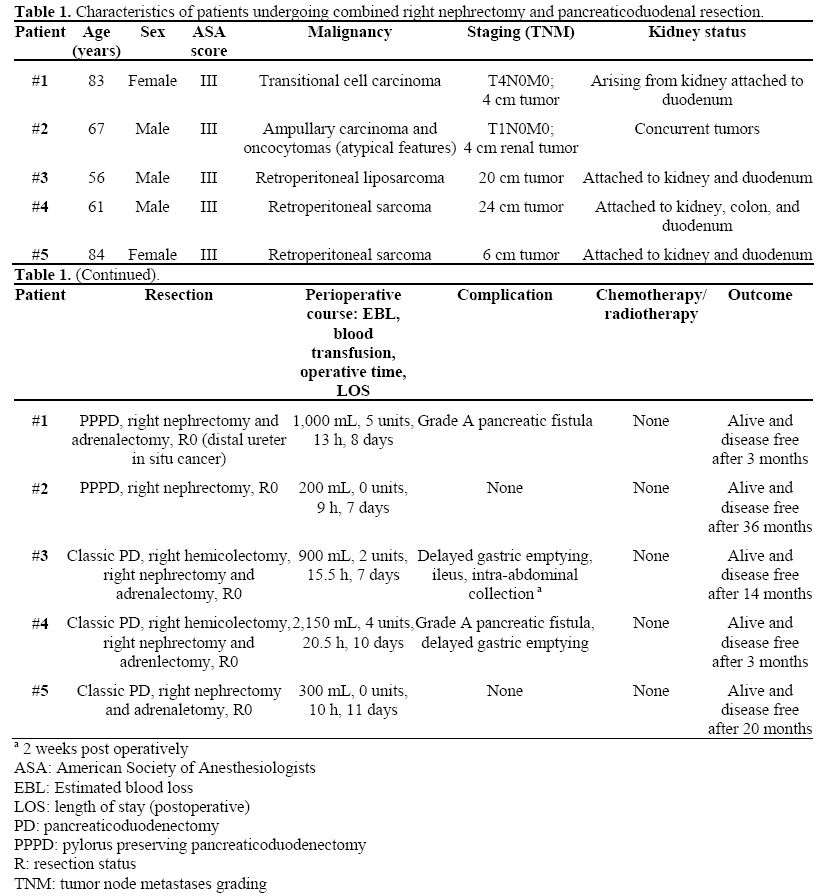
Figure 1. Computed tomography (CT) images of two cases showing adherence of retroperitoneal sarcomas to the right kidney and duodenum/pancreas requiring combined resection. a. Sagittal section showing tumor (*) attached to the inferior pole of the kidney and duodenum (Patient #4). b. Axial image depicting the large size of the tumor, with surrounding inflammatory change due to an episode of pancreatitis (Patient #4). c. Coronal section showing tumor located adjacent to hilum of the right kidney abutting the portal vein and duodenum. An incidental abdominal aortic aneurysm is demonstrated (Patient #5). d. Axial view more clearly showing attachment of sarcoma to duodenum anteriorly (Patient #5).
The median operating time was 13 hours (range: 9-20.5 hours). Median estimated blood loss was 900 mL (200-2,150 mL). Blood transfusions were required in 3 patients. Median postoperative intensive care stay was 2 days (1-6 days). One or more complications were noted in 3 cases (60.0%). Two patients had low volume pancreatic fistulae that were managed conservatively and did not prolonged hospital stay. Median length of post-operative hospital stay was 8 days (7-11 days). All radial resection margins were clear of malignancy. One patient with transitional cell carcinoma, had carcinoma in situ at the ureteral cut margin. Median followup in this series was 14 months (3-36 months), with all patients alive and disease free at the time of the last review.
Nephrectomy and pancreaticoduodenal resection are often performed for the treatment of malignancy. The outcomes of patients undergoing nephrectomy are well document for both open and laparoscopic procedures [5]. Similarly, outcomes of large series of patients treated by pancreaticoduodenal resection are increasingly reported [6, 7]. However, reports of combined nephrectomy and pancreaticoduodenal resection are limited to isolated case reports [2]. The indications for combined procedures, surgical approach and outcomes are essentially unknown.
The complication rate for nephrectomy is well described in large series and varies somewhat between laparoscopic and open approaches [5, 8]. Generally nephrectomy is associated with low major complication rates. In a series of 98 patients undergoing open nephrectomy, the overall complication rate was 31%, with a median operating time of 3 hours [5]. There was no perioperative mortality. Wound related complications were most common, followed by ileus. The estimated blood loss was 216 mL with less than 10% of patients requiring a blood transfusion. The median length of hospital stay in this series was 6 days. The median blood loss in other recent open nephrectomy series range from 216 to 371 mL and the median hospital stay range from 4 to 16 days [9, 10, 11]. In our series there were no specific complications related to nephrectomy and all patients had preserved renal function based on comparisons of preoperative and postoperative serum creatinine measurements.
The morbidity and mortality of pancreaticoduodenal resection has been the subject of numerous publications [6, 7, 12]. The mortality rate with this procedure ranges from 1 to 5% in large series [6, 7, 13]. Morbidity remains high, ranging from 30 to 50% [4, 6, 7, 12]. Delayed gastric emptying remains the most common complication occurring in 15 to 45% of cases depending on the definition used [14]. Pancreatic fistula is the next most common complication of pancreaticoduodenal resection ranging from 2% to more than 20% [4, 6]. The median length of hospital stay is quoted as 9 days in large volume pancreatic centers [6, 15]. In our series, the observed morbidity was related to pancreaticoduodenal resection and reflects finding reported elsewhere in literature [4, 6, 7, 12].
The morbidity observed in our cases is not unexpected given the complexity of tumors treated. Three patients had retroperitoneal sarcomas attached to right kidney and duodenum. One of these patients also had attachment of tumor to the right colon. The median operating time and estimated blood loss was 13 hours and 900 mL, respectively. Blood transfusions were required in 3 of 5 cases (60%). Pancreatic fistulas occurred in two patients (40%). This is acceptable particularly given that all pancreatic anastomoses in this series involved high risk cases, based on pancreas texture. Four patients had a soft texture pancreas, with one developing a fistula. The remaining patient with a retroperitoneal sarcoma had patchy necrosis of the pancreas due to a previous episode of severe acute pancreatitis. In both cases of pancreatic fistula, this did not have significant clinical impact on patient outcomes, resolving with conservative treatment. Delayed gastric emptying was noted in two patients, treated by a short period of total parenteral nutrition. The median length of hospital stay in this series was 8 days and reflects the low clinical impact of complications observed. This also reflects our early discharge policy, particularly in patients that are otherwise well, but with delayed gastric emptying. There are no other reports of series of patients treated by en bloc right nephrectomy and pancreaticoduodenectomy to compare with our series. Although there are no other such reports, the morbidity associated with this procedure is similar, if not better than other reports, where multivisceral operations are performed, that include pancreatic resection [1, 16, 17].
The indications and outcomes of patients undergoing combined right nephrectomy and pancreaticoduodenectomy have not previously been defined. The only other detailed report of combined right nephrectomy and pancreaticoduodenectomy is a case of a patient with colon cancer invading into the pancreas and kidney [2]. Even in large reviews of patients undergoing pancreaticoduodenectomy or nephrectomy, the combination of both procedures is rarely reported. Renal malignancies very rarely attach to the duodenum and pancreas, and in most circumstances can be separated from these organs. In our series, one patient with transitional cell cancer had a locally advanced tumor attached to duodenum and pancreas with surrounding inflammatory change, not allowing for a lesser resection. In another patient with a concurrent renal tumor and ampullary adenocarcinoma, for oncologic reasons it was felt that en bloc resection should be undertaken. Combined resection of pancreas and right kidney appears most applicable to retroperitoneal sarcoma attached to both kidney and periampullary region. If there is a small focus of tumor attachment to the duodenum, partial duodenal resection with appropriate repair should be contemplated. More often, distinguishing tumor boundaries can be very difficult and any breach of these boundaries could equate to early tumor recurrence. A combined en bloc resection in these cases may ensure clear resection margins and no recurrence has been observed to this date. In our series 3% of pancreaticoduodenal resections were combined with right nephrectomy. This is a higher percentage than expected, but partly reflects our interest and aggressive approach to the management of advanced retroperitoneal malignancies.
Right nephrectomy combined with a pancreaticoduodenal resection appears to be a safe operative procedure for resection of tumors invading the right kidney and duodenum/pancreas, those located in close proximity to both regions and in the cases of concurrent tumors. En bloc resection can be performed to minimize the risk of positive margins without increased morbidity. The morbidity of this procedure appears to be related to pancreaticoduodenal resection alone.
The authors have no potential conflicts of interest