Enow Orock GE1, Takang W2, Enow Orock A3*, Ewane TP3, Egbe OT4, Halle Ekane G4 and Mbu RE5
1National Cancer Control Program, Cameroon
2Regional Hospital Bamenda, Cameroon
3Regional Hospital Buea, Cameroon
4General Hospital Douala, Cameroon
5Central Hospital Yaounde, Cameroon
- *Corresponding Author:
- Professor George Enow Orock
Regional Hospital Buea
South-West Region, Cameroon
Tel: 237 67771 6045
Email: enowrock24@yahoo.com
Received Date: December 26, 2018; Accepted Date: January 23, 2019; Published Date: January 31,
2019
Citation: Enow Orock GE, Takang W, Enow Orock A, Ewane TP, Egbe OT, et al. (2018) Comorbidity of HIV and Cervical Cancer: A One Year Multicentric Pilot Study in Cameroon. J HIV Retrovirus. 5:2. doi: 10.21767/2471-9676.100052
Background: Although the national prevalence of HIV infection has reduced in the past few years in Cameroon, patients with HIV-related malignancies, especially cervical cancer are on the rise. There is enormous challenge in the management of these patients in our setting. Both diseases respectively and collectively, have a high morbidity and mortality. Few studies on the profile of patients with both HIV infection and cervical cancer have been carried out in our setting, whereas their Knowledge is essential in the short and long term management strategies for both diseases. This study was aimed at finding the factors associated with co morbidity of HIV and cervical cancer.
Objective: The main objective of this study was to find out the relationship between cervical cancer and HIV infection among patients in our community. Specifically we wanted to find out the transition time from HIV+ to HIV-cervical cancer amongst these patients.
Materials and Methods: This is a one year prospective, cross-sectional, multicentre pilot study from January to December 2015, in 5 hospitals across 3 regions of the country. Vital data on the patients and data concerning both HIV infection and cervical cancer respectively were assembled and analyzed.
Results: We found 66 patients with various malignant cervical lesions with a coinfection of HIV in this study. The patients ranged in age between 24 and 71 years and majority (63.6%) were aged 40 years and above, with 56% having attained at least a secondary education and majority were married (70%). The main finding was a squamous cell lesion which was invasive carcinoma (68.18%) or a dysplasia (16.66%). The commonest HIV serotype amongst patients was type 1 (66.7%), though in 18.2% of cases there was HIV type 1 and 2 co-infection. Majority of cases had CD4 counts below 400 cells/mm3. The average duration of the infection before apparition of cancer was 2.5 years. In all cases, cancer was diagnosed after HIV infection.
Conclusion: HIV and cervical cancer co morbidity prevalence is increasing in our community. Cervical cancer occurs within few years following HIV. The risk factors of these co-morbid conditions include infection by HIV serotype I, a low CD4 count, married women and a high educational level. This conclusion is in reserve of our sample size and in disregard of income factor amongst the patients.
Though a squamous cell lesion is more predominant, adenocarcinoma is also common in patients. Screening and treatment for cervical cancer and appropriate HIV management strategies should be instituted as soon as the infection is diagnosed. Cervical cancer surveillance should be intensified within the first few years following HIV infection.
Keywords
Cervical; Cancer; HIV; Cameroon
Introduction
The burden of disease in developing countries is being overwhelmed by known and emerging infections. It has also been shown by various studies that non-communicable diseases are becoming a public health problem in these communities [1]. Numerous viral infections have for long been associated with various types of cancers. Prominent amongst these is the relationship between the Human Papillomavirus (HPV) and cervical [1-3]. The history of HIV (Human Immuno-deficiency Virus) and its link with cancer started with the first descriptions of AIDS (Acquired Immuno-deficiency Syndrome) [4]. People infected with HIV have a higher risk of some types of cancer than uninfected people. Almost 4 decades after the apparition of the HIV/AIDS pandemic, new challenges to this disease are being faced by patients and the global health systems. Patients are living longer with HIV infection due to increase availability of HAART (Highly Active Anti-retroviral Therapy) with increased chances of developing a cancer [5].
Globally there are about 270,000 deaths from cervical cancer per annum with over 85% of these occurring in low resource countries, where it is the leading cause of cancer deaths in women [6,7]. Cameroon is rated as having and an age-standardized incidence rate of 87.3 cervical cancer cases per 100.000 persons [8].
There is still much controversy concerning the relationship between HIV and invasive cervical cancer. Globally, an increased risk of HPV infection and cervical pre-cancerous squamous intraepithelial lesions has been found in HIV-positive women [9,10]. In some European populations, like HPV, a positive association of HIV infection and invasive cancer of the cervix has also been documented [11,12]. However most studies in Africa on this association have been conflicting and inconclusive [13- 16]. While some of the studies infer that HIV infection could act as a cofactor for this disease in HPV infected women [17], others found no association between the two [18].
The interaction between HIV and host antigens and eventual occurrence of related cancers has not been fully understood. Due to immune compromise, cervical cancer in AIDS patients has peculiar characteristics different from that in immune competent patients [12]. If HIV infection increases both the likelihood of cervical cancer developing from dysplasia and the likelihood of a worsening of the stage of cervical cancer, a correlation could be expected between the HIV prevalence in Cameroon and the incidence of cervical cancer.
The national HIV infection rate in Cameroon has decreased from 12% in 1995 to 4.5% in 2014, yet there has been an upsurge of both AIDS-defining and other cancers in patients with the infection [19]. This is due to longer survival of HIV-infected patients which increases the risk of cancer amongst them. This occurs even though preventive actions against cervical cancer began two decades ago and culminated in 2014 with the launching of the National Programme of Vaccination against Human Papilloma Virus in Cameroon [20]. The advent of HIV/AIDS has caused a significant change in the epidemiology of cancer in Cameroon, reducing the average incidence age for the latter in the population by about 8 years [21].
In resource-stressed communities like ours, numerous difficulties are faced in the management of HIV/AIDS and cancer patients respectively, and the situation is worse in patients who have both diseases. The role of underlying genetics, co-infections, and lifestyle exposure to known/unknown antigens can never be underestimated, and therefore scientists should continue to investigate the interaction of HIV and its proteins with host machinery in the aetiology of oncogenesis from a molecular to epidemiologic level. This study of the profile of patients with co morbidity of HIV and cervical cancer in Cameroon is aimed at documenting basic epidemiologic and other findings that characterise patients with both diseases and serve as platform for further studies.
Materials and Methods
For this prospective study, data on patients with both HIV infection and cancer from 5 randomly selected pilot centres of an NCI (USA)-sponsored HIV malignancies project were assembled. The data collection began from January 1 to December 31, 2015. The patients were recruited at services in concerned with the management of cancer or HIV respectively. A patient who tested positive for the condition in one service was sent to the other service for the other specialized test. Patients who were found to be positive for both conditions were documented. It is from this cohort that we recruited patients who were positive for both HIV and a cervical cancer. Data on these patients was assembled and analyzed. Specifically we documented vital data on the patients with both co morbidities, data on HIV infection including mode of transmission, serotype, duration of infection and CD4 count. Concerning cancer we found out the morphology and extent of the disease. We then proceeded to cross-match these to find out if there was any association between them. Dates for incidence of the respective morbidities was inferred from the date of their respective diagnosis and HIV to cancer conversion time was calculated from date of diagnosis of HIV infection to date of diagnosis of associated cancer. It is from this cohort that we extracted data on patients who tested HIV positive and had a cervical cancer. The vital statistics of the patient, data on HIV on and data on the cancer were all assembled and analysed. The duration of both cancer occurrence and HIV infection were inferred from the respective dates of diagnoses of the diseases.
Results
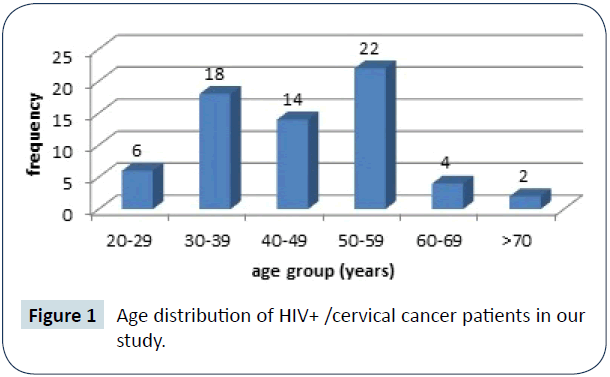
Cervical cancer in HIV+ patients predominates at 2 peak age groups (30-39 years-27.3%) and (50-59 years-33.3%). A high proportion of cases are below 40 years of age (36.4%).
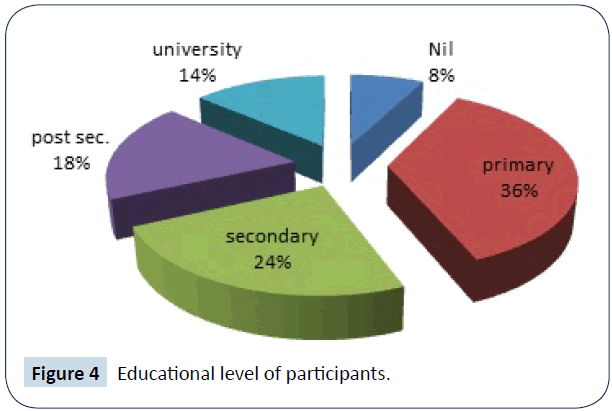
Majority (56%) of participants had a secondary education and beyond and 44% had not gone beyond primary school.
3 out of 10 regions of the country (30%) were covered by the study. Majority of patients (77.3%) were from the Center region. An annual average of 66 cases of HIV+/cervical Cancer cases was obtained.
Discussion
In Cameroon, breast and cervical cancers are the leading causes of cancer-related morbidity and mortality [20]. Cervical cancer is one of the AIDS-defining illnesses [22]. This is based on the observation that women infected with HIV had a significantly higher risk of developing Squamous Intraepithelial Lesions (SIL), the pre-malignant stage of cervical cancer, and a faster progression to more advanced stages of the diseases [23].
Other studies have also suggested [24], while others confirmed [25], yet some authors found an inconclusive correlation between malignant cervical lesions and HIV infection [26]. Nawal reported that Immune depression especially by HIV is known to be a risk factor for cervical cancer [7]. Innocent et al. hypothesized that HIV facilitates infection with specific types of HPV, some of which may promote (HPV-p types) or inhibit (HPV-i types) progression to cervical carcinogenesis in any single individual [22], while others [27] went as far as qualifying that HIV positive patients had 8.5 times risk to develop cervical cancer than their HIV negative counterparts.
We found 66 patients with co-morbid conditions of cervical cancer and infection with HIV in a one year prospective, crosssectional, multi-centre, pilot study in Cameroon (Table 1). This was more than previous reports [4] which found 36 cases in a ten year study in one hospital in Kenya. This disparity in incidence could be explained by the multiplicity of our study sources.
| Cancer Morphology |
Frequency |
Percentage |
| Squamous cell |
Invasive |
45 |
68.2 |
| Dysplasia |
11 |
16.7 |
| Adenocarcinoma |
4 |
6.06 |
| Adeno-squamous carcinoma |
4 |
6.06 |
| Angiosarcoma |
1 |
1.52 |
| Choriocarcinoma |
1 |
1.52 |
| Total |
66 |
100 |
Table 1 Cervical cancer morphology amongst HIV+ patients.
Our patients ranged in age between 24 and 71 years at an average of 45.4 years and majority (33.3%) were in the 50-59 years age range (Figure 1). This finding was lower than a previous report [21] where a peak age of 50-59 years and an average of 55 years was found amongst HIV-naïve cervical cancer patients in Cameroon. Our finding was however similar to some [4] who found a mean age at diagnosis of cervical cancer of 47 years in HIV naïve patients. Sando [20] and Rhamadani [28] reported in a ten years study on trends of breast and cervical cancer in Cameroon and the influence of HIV infection on cervical cancer respectively that cervical cancer occurred in patients above 30 years of age.
Figure 1: Age distribution of HIV+ /cervical cancer patients in our
study.
Similar to our study, earlier reports in Zimbabwe showed that HIV-seropositive women with invasive cervical cancer were 5 years younger than HIV-negative women with invasive cervical cancer [29]. In the same trend Lomalisa et al. [30] reported that HIV-seropositive women in South Africa presented with invasive cervical cancer 10 years earlier than HIV-negative women. Most of our patients (58%) were aged 20-49 years, like Myeni who concluded in a similar study that HIV-positive cervical cancer patients were predominantly less than 49 years of age compared to their HIV negative counterparts [31].
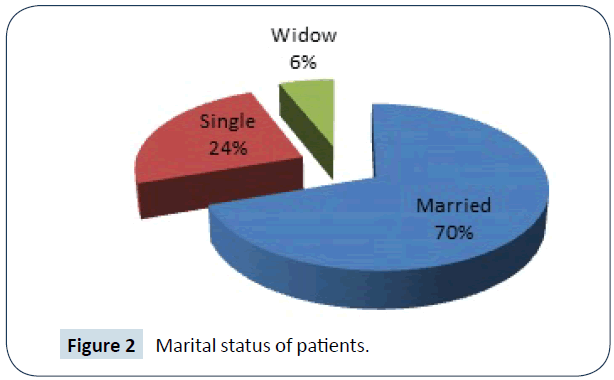
In this study we covered 3 out of 10 regions of the country (30%); a ratio likely to impact on the national incidence of this disease (Table 2). Up to 69.7% of our patients were married (Figure 2). In consideration of HIV versus marital status, this rate is higher than the report by Shisana in South Africa who found HIV prevalence among married people of 10.5% compared to 15.7% among unmarried people. They inferred in their work that the risk of HIV infection did not differ significantly between married and unmarried people; and concluded that the relationship between marital status and HIV is complex, depending on various demographic factors and sex behaviour practices [32]. In a different study however, the author reported that those who were married living with their spouse had significantly reduced odds of being HIV-positive compared to all other marital spouses groups [33] We did not study marital sub groups in this work.
| Hospital |
Region |
N (%) |
| Central Hospital Yaounde |
Centre |
39 (59.1) |
| University Hospital Yaounde |
Centre |
8 (12.1) |
| Regional Hospital Bamenda |
North- west |
1 (1.5) |
| General Hospital Yaounde |
Centre |
4 (6.1) |
| Regional Hospital Buea |
South west |
14 (21.2) |
| All hospitals |
3 |
66 (100) |
Table 2 Data sources for study on HIV+/ cervical cancer patients.
Figure 2: Marital status of patients.
Considering the relationship between cervical cancer and marital status, the relative rarity of the disease in the unmarried and its higher incidence in formerly married than in currently married women had been reported with inference to association of the disease with number of sexual partners [34]. The same trend was reported by Sanae who attributed the protective effect of marriage from cervical cancer to be mostly at the level of prevention of the disease [35]. Myeni had a contrary finding in his study when he concluded that cervical cancer patients that were never married were 3.7 times more likely to be HIV positive than married patients [31].
The HIV serotype was predominantly type 1 (66.7%). This is higher than previous reports where an HIV-1 prevalence of 21.0% in a comparative study of HIV positive and negative women and concluded that HIV-1 infection is associated with invasive cancer of the cervix [36]. In 18.2% of our cases, infection was both by HIV serotypes 1 and 2. This is similar to an earlier report of 19.2% concurrent HIV-1/ HIV-2 infection in a study in Cameroon [37].
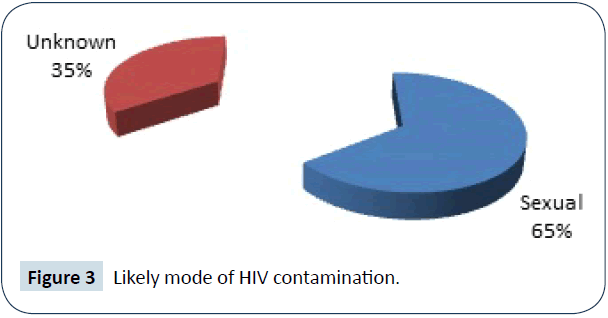
Concerning the route of contamination, it was mainly sexual for the cases where data was provided (Figure 3). This finding had been reported in previous studies [38].
Figure 3: Likely mode of HIV contamination.
In our study, majority (56%) of participants had a secondary education and beyond, while 44% had not gone beyond primary school (Figure 4). This is in contradiction to the common notion that cervical cancer is a disease of the lower class [39], assuming that education infers a high socio-economic status. Our finding is similar to the trend though lower in value to Hailemariam [27] who reported that the likelihood of cervical cancer among literate women was 6.1 times higher as compared to illiterate women at a value of 78.9% compared to the later.
Figure 4: Educational level of participants.
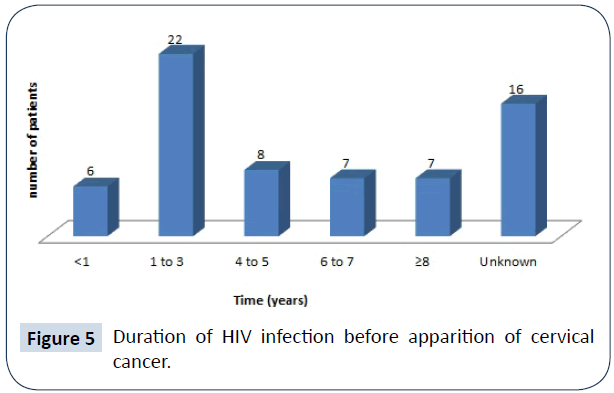
In all cases (100%), the HIV infection preceded the apparition of cervical cancer for periods ranging between 1-6 years. The average duration of the infection before diagnosis of cancer was 2.5 years (Figure 5). Like in our study, some reports indicated the time interval since HIV/AIDS diagnosis amongst cervical cancer patients ranged from 1 month to 10 years, with a mean of 2.5 ± 2.2 years [40]. At the time of diagnosis most patients had CD4 counts between 200 and 500 cells/mm3 (66%) amongst cases whose counts were known at a mean of 400 cells/mm3 (Table 3). This is similar to an earlier report by where majority of cases (73.9%) had a CD4+ cell count between 200 and 500 cells/mm3 [40].
| CD4 count |
Frequency |
Percentage |
| Jan-99 |
0 |
0 |
| 100-199 |
3 |
4.54 |
| 200-299 |
4 |
6.06 |
| 300-399 |
11 |
16.66 |
| 400-499 |
8 |
12.12 |
| =500 |
2 |
3.03 |
| Unknown |
38 |
57.58 |
| All counts |
66 |
100 |
Table 3 CD4 count in HIV+/cervical cancer patients at time of cancer
diagnosis.
Figure 5: Duration of HIV infection before apparition of cervical
cancer.
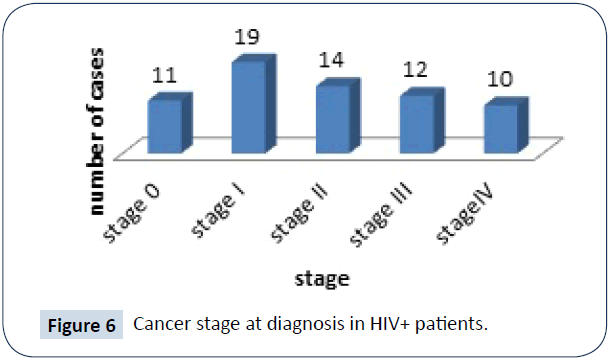
Infection with HIV has been shown to be a risk factor for cervical cancer [41] and was also reported that HIV-positive women develop more cervical precancerous lesions compared with HIV negative women. The main pathological diagnosis found in our study involved the epithelial squamous cell of the cervix (Table 1). In 16.7% of our cases, the cervical lesion was a dysplasia (I, II or III). Earlier comparative studies had indicated that the prevalence of cervical precancerous lesions was higher (71.8%) in HIV-positive women than in HIV-seronegative women [28]. In this same study the prevalence of invasive cervical cancer was 8% in HIV-seronegative women and 11% in HIV-positive women, lower than our rate of 68.18%. Most of our patients were diagnosed with cancer at stage ≤ II (66.7%) (Figure 6). This is contrary to previous reports on stage of diagnosis of cancer from HIV naive screening studies in this community [21]. It is also contrary to a study in Zambia among HIV infected women which stated that not only does cervical cancer occur more in the immune suppressed, but HIV positive women also have higher likelihood of having high grade cervical squamous intra epithelial lesions [42]. Probably HIV infection promotes early presentation of patients to a health facility for checkups and consequently enables early screening and diagnosis of cervical cancer in HIV+ patients with various cervical lesions. This view had been expressed in an earlier report [21]. Unlike our finding some reports [4] found a lower rate of 44.6% cases of HIV/cervical cancer cases at stage ≤ II and concluded that there was no significant change in either age at presentation or severity of cervical cancer in HIV+ cervical cancer patients compared to HIV- counterparts. Though some reports have shown that the role of immunosuppression in the progression to invasive cancer may be marginal [43], we found a squamous cell lesion was the commonest histologic finding (84.84%) and a squamous cell carcinoma was most predominant, while in few cases the lesion was a dysplasia. 12.12% of these HIV-immune depressed patients had an adenocarcinoma of the cervix. This is lower than the finding that reported adenocarcinoma of the cervix to make up more than 20% of all cervical cancer cases diagnosed each year in the United States [44] and similar to others who found the rate to be above 12.5% [45].
Figure 6: Cancer stage at diagnosis in HIV+ patients.
Limitations of this Study
The present work has some limitations that should be considered in interpreting the results. First, the study participants were recruited from hospitals; thus, the findings might not be truly representative of HIV-infected women with cervical cancer who do not have access to hospitals. Second, this study was completed at 5 pilot sites and results cannot be generalized to all HIVpositive cervical cancer patients all over Cameroon. Third, the small sample size limited further analysis of factors that influence co morbidity of the 2 diseases. Fourth, the short duration could impact on our findings. Lastly, the information provided by the participants could be affected by social acceptability bias and/ or recall bias, despite our attempts to minimise this by ensuring anonymity.
Acknowledgements
The authors are grateful for the sponsorship by the New York University School of Medicine (NYUSoM) Daugherty Centre and the National Institute of Health (NIH) in the USA with Grant number D43CA153726.
Ethical clearance for the study was obtained from the Ministry of Public Health Ethical Review Board and the local Ethical Review Boards of the various institutions involved in the study.
Conflict of Interest
The authors declared no conflict of interest.
Contribution of Authors
All authors contributed in the conception, collection of data, write up, analysis, and proof reading of this article.
References
- Joint United Nations Programme on HIV and AIDS (2014) The Gap Report.
- Joint United Nations Programme on HIV and AIDS (2014) World AIDS Day Report Fact Sheet.
- Lima DV (2015) AIDS incidence and AIDS-related mortality in British Columbia, Canada, between 1981 and 2013: A retrospective study. The Lancet HIV 2: 92-7.
- Gichangi P, De Vuyst H, Estambale B, Rogo K, Bwayo JJ, et al. (2002) HIV and cervical cancer in Kenya. Int J Gynaecol Obstet 76: 55-63.
- Shiels MS, Pfeiffer RM, Gail MH, Hall I, Li J, et al. (2011) Cancer burden in the HIV-Infected population in the United States. J Natl Cancer Inst 103: 753-62.
- Parkin DM, Pisani P, Ferlay J (1999) Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer 80: 827-41.
- Nawal MN (2009) Cervical cancer: A preventable death. Rev Obstet Gynecol 2: 240-4.
- GLOBOCAN (2012) 2004-2006/2010-2011. Yaounde cancer registry technical report, Yaounde: National Cancer Control Committee, Cameroon.
- Abdus-Salam A, Ogunnorin O, Abdus-Salam R (2008) HIV seroprevalence in patients with carcinoma of the cervix in Ibadan, Nigeria. Ghana Med J 42: 141-3.
- Franceschi S, Dal Maso L, Pezzotti P, Polesel J, Braga C, et al. (2003) Incidence of AIDS-defining cancers after AIDS diagnosis among people with AIDS in Italy, 1986-1998. J Acquir Immune Defic Syndr 34: 84-90.
- Franceschi S, Dal ML, Arniani S, Re AL, Barchielli A, et al. (1998)Linkage of AIDS and cancer registries in Italy. Int J Cancer 75: 831-4.
- Dal ML, Serraino D, Franceschi S (2001) Epidemiology of AIDS-related tumours in developed and developing countries. Eur J Cancer 37: 1188-1201.
- Hawes SE, Critchlow CW, Faye Niang MA, Diouf MB, Diop A, et al. (2003)Increased risk of high-grade cervical squamous intraepithelial lesions and invasive cervical cancer among African women with human immunodeficiency virus type 1 and 2 infections. J Infect Dis 188: 555-63.
- Rabkin CS, Biggar RJ, Baptiste MS, Abe T, Kohler BA, et al. (1993) Cancer incidence trends in women at high risk of human immunodeficiency virus (HIV) infection. Int J Cancer 55: 208-12.
- Sun XW, Kuhn L, Ellerbrock TV, Chiasson MA, Bush TJ, et al. (1997) Human papillomavirus infection in women infected with the human immunodeficiency virus. N Engl J Med 337: 1343-9.
- Dal ML, Serraino D, Franceschi S (2001) Epidemiology of AIDS-related tumours in developed and developing countries. Eur J Cancer 37: 1188-1201.
- Adjorlolo-Johnson G, Unger ER, Boni-Ouattara E, Touré-Coulibaly K, Maurice C, et al. (2010)Assessing the relationship between HIV infection and cervical cancer in Cote d'Ivoire: a case-control study. BMC Infect Dis 10: 242.
- Odida M, Sandin S, Mirembe F, Kleter B, Quint W, et al. (2011) HPV types, HIV and invasive cervical carcinoma risk in Kampala, Uganda: a case-control study Infect Agent Cancer 6: 8.
- Enow-Orock G, Ngowe NM (2013) Mortality and morbidity in HIV/AIDS patients in Yaounde, Cameroon. Online J Med and Medical Sc Res 2: 44-8.
- Sando Z, Fouelifack YF, Fouogue TJ, Essame-Oyono JL (2015) Trends in breast and cervical cancer incidence n Cameroon (Central Africa) from 2004 to 2011. J Afr Cancer 7: 118-21.
- Orock GE, Ndom P, Doh AS (2012) Current cancer incidence and trends in Yaounde, Cameroon. OGH Rep 1: 58-63.
- Maranga IO, Hampson L, Oliver AW, He X, Gichangi P, et al. (2013) HIV Infection alters the spectrum of HPV subtypes found in cervical smears and carcinomas from Kenyan women. Open Virol J 7: 19-27.
- Gemignani M, Maiman M, Frutcher RG, Arrastia CD, Gibbon D, et al. (1995) CD4 Lymphocytes in women with invasive and preinvasive cervical neoplasia. Gynecol Oncol 59: 364-369.
- Maggwa BK, Hunter DJ, Mbugua S, Tukei P, Mati JK (1993) The relationship between HIV infection and clinical intraepithelial neoplasm among women attending two family planning clinics in Nairobi, Kenya. AIDS 7: 733-8.
- Ruche GL, Ramon R, Mensah-Ado I, Bergeron C, Diomande M, et al. (1998) Squamous intraepithelial lesions of the cervix, invasive cervical carcinoma and immunosuppression induced by human immunodeficiency virus in Africa. Cancer 82: 2401-8.
- Serraino D, Carrieri P, Pradier C, Bidoli E, Dorrucci M, et al. (1999) Risk of invasive cervical cancer among women with, or at risk for, HIV infection. Int J Cancer 82: 334-7.
- Hailemariam T, Yohannes B, Aschenaki H, Mamaye E, Orkaido G, et al. (2017) Prevalence of cervical cancer and associated risk factors among women attending cervical cancer screening and diagnosis center at Yirgalem General Hospital, Southern Ethiopia. J Cancer Sci Ther 9: 730-5.
- Ramadhani SC, Stephen S, Salum JL, Ntoli M, Rui MM (2017) Influence of HIV/AIDS on cervical cancer: A retrospective study from Tanzania. Journal of Global Oncology 3: 72-8.
- Chokunonga E, Levy LM, Bassett MT, Mauchaza BG, Thomas DB, et al. (2000) Cancer incidence in the African population of Harare, Zimbabwe: second results from the cancer registry 1993-1995. Int J Cancer 85: 54-9.
- Lomalisa P, Smith T, Guidozzi F (2000) Human Immunodeficiency virus infection and invasive cervical cancer in South Africa. Gynecol Oncol 77: 460-3.
- Myeni, Sebentile N (2015) Factors associated with co-morbidity of HIV and cervical cancer in Swaziland. Dissertation (MPH)-University of Pretoria.
- Shisana O, Zungu-Dirwayi N, Toefy Y, Simbayi LC, Malik S, et al. (2004) Marital status and risk of HIV infection in South Africa. S Afr Med J 94: 537-43.
- Shisana O, Risher K, Celentano DD, Zungu N, Rehle T, et al. (2016) Does marital status matter in an HIV hyperendemic country? Findings from the 2012 South African National HIV Prevalence, Incidence and Behaviour Survey. AIDS Care 28: 234-41.
- Leck I, Sibary K, Wakefield J (1978) Incidence of cervical cancer by marital status. J Epidemiol Community Health 32: 108-10.
- Sanae EI, Paulo P (2013) The effect of marital status on stage and survival in women with cervical cancer. Conference Paper. Conference: American Society of Preventive Oncology (ASPO), At Memphis, TN.
- Crispin K, Julius M, Henry RW, Twalib N, Joan NK, et al. (2008) Association between invasive cancer of the cervix and HIV-1 infection in Tanzania: the need for dual screening. BMC Public Health 8: 262.
- Nsagha DS, Njunda AL, Kamga HLF, Assob JCN, Bongkem EA (2012) HIV-1/HIV-2 co-infection among voluntary counselling and testing subjects at a regional hospital in Cameroon. Afr Health Sci 12: 276-81.
- George MS, Eric H (2012) HIV Transmission. Cold Spring Harb Perspect Med 2: a006965.
- Seema P, Brennan P, Boffettameta P (2003) Analysis of social inequality and risk of cervical cancer. Int J Cancer 105: 687-91.
- Belglaiaa E, Souho T, Badaoui L, Segondy M, Prétet JL, et al. (2018) Awareness of cervical cancer among women attending an HIV treatment centre: a cross-sectional study from Morocco. BMJ Open 8: e020343.
- Silverberg MJ, Neuhaus J, Bower M, Gey D, Hatzakis A, et al. (2007) Risk of cancers during interrupted antiretroviral therapy in the SMART study. AIDS 21: 1957-63.
- Singh GK (2012) Rural-urban trends and patterns in cervical cancer mortality, incidence, stage, and survival in the United States, 1950-2008. J Community Health 37: 217-23.
- Aklimunnessa K (2006) Effectiveness of cervical cancer screening over cervical cancer mortality among Japanese women. Jpn J Clin Oncol 36: 511-8.
- Smith HO, Tiffany MF, Qualls CR, Key CR (2000) The rising incidence of adenocarcinoma relative to squamous cell carcinoma of the uterine cervix in the United States-a 24-year population-based study. Gynecol Oncol 78: 97-105.
- https://radiopaedia.org/articles/