Keywords
Public health; Health quality index; Child health; Women health; Health infrastructure
Introduction
Health is a state of physical, mental and social well-being in which disease and infirmity are absent [1]. Public health is "the science and art of preventing disease”, prolonging life and improving quality of lifethrough organized efforts and informed choices of society, organizations, public and private, communities and individuals" [2]. Good health and well-being have also been incorporated as the third goal within the SDGs (Sustainable Development Goals) 2015-30. Knowing the state of public health can help make informed policy decisions. Child health has been described as perhaps the most sensitive barometer of the fitness of the social environment for human life' (Lewis Mumford). The state of Women's Health indicates the degree of social development and gender parity. Health Infrastructure includes the presence of safe drinking water, health cover; primary health centres etc. and facilitates the realization of the fundamental right to good health [3].
Literature Review
Construction of an index helps to understand a given issue by means of a single representative figure. This methodology of using indices, especially for social dimensions started with the Human Development Report of the United Nations Development Programme [4]. This flagship report of the UNDP published on an annual basis uses Health Index as one of the dimensions of human development and uses the indicator of average life expectancy at birth for the same [5]. The national think tank of India NITI Aayog also constructed a State Health Index in its Healthy States, Progressive India report [6]. It came up with the SDGIndia (Sustainable Development Goals India) Index to measure the progress of Indian states with respect to the Sustainable Development Goals 2015-30 adopted by the United Nations Organization [7]. Philippas D [8] created a Children’s Health Index as a tool within Encyclopedia of Quality of Life and Well-Being Research (Philippas, 2014). Supravat Bagli [9] worked on a MPI (Multi Dimensional Poverty Index) using health as a dimension and observed that on average 58 percent households in North- East India collect drinking water from unsafe source, percentage of households having access to unsafe source of drinking water is highest in Nagaland followed by Sikkim and Manipur [9]. Bhattacharya and Mal [10] that the healthcare system of Northeastern states is much weaker than that of the country as a whole in terms of healthcare infrastructure. The authors observed that among all the North-East states, the lowest prevalence of full immunization was observed in Arunachal Pradesh and Nagaland; Vitamin-A in Manipur, Arunachal Pradesh and Nagaland. The prevalence of stunting and wasting was observed to be very high in Meghalaya and underweighted children were observed in Tripura, Nagaland, Arunachal Pradesh, Assam and Meghalaya. Rudra [11] worked on north eastern states and found that Nagaland has the poorest maternal and child healthcare indicators in Northeast India.
Objective
The objective of this paper is to assess the state of public health in the districts of the north-eastern states of India, namely Assam, Arunachal Pradesh,Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura.
Study area
The study area comprises of the eight north-eastern states of India, viz. Assam, Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura. These states lie in the far eastern part of India, separated by the chicken neck corridor (Figure 1). The latitudinal range of these states is from 29°22’4’’ N to N-2°57’2’’ N and the longitudinal range is from 87°58’38’’E to 97°21’20’’E. These states have an expanse of 2,62,179 km2, i.e. nearly 8 per cent of the total area of India and a combined population of 45,588,381 which is nearly 4 per cent of the country’s population. The most populated state is Assam while Sikkim is the least populated state. The physiography is marked by the eastern Himalayas (Sikkim and Arunachal Himalayas), the Purvanchal hills and the Meghalaya plateau. Majority of the area lies in the watershed of the Brahmaputra River, the largest river in this region. Apart from the flood plains, the landscape is marked by dense tropical broadleaved evergreen forests nourished by annual precipitation averaging above 250 cm, taiga and alpine forests in higher reaches. Hence, this is a unique biome. There are total 86 districts spread across the eight states which are inhabited 160 scheduled tribes, as per the sixth schedule of the Indian constitution. It is estimated that more than 500 ethnic groups are speaking nearly 400 languages and dialects in this region. It has been India’s gateway to South-East Asia. he region shares an international border of 5,182 kilometres (3,220 mi) (about 99 per cent of its total geographical boundary) with several neighbouring countries -1,395 kilometres (867 mi) with Tibet Autonomous Region, China in the north, 1,640 kilometres (1,020 mi) with Myanmar in the east, 1,596 kilometres (992 mi) with Bangladesh in the south-west, 97 kilometres (60 mi) with Nepal in the west, and 455 kilometres (283 mi) with Bhutan in the north-west. Historically, there have been tribal confederacies and kingdoms here and post-Independence, frequent insurgency has been a part of the process of integration into India in some regions. Due to the relative geographical isolation and various other issues, this region has lagged behind in development, and consequentially, there is a huge prospect of developing the human capital [12].
Database
The data for this study has been taken from the District Factsheet Report of the National Family Health Survey (Round 4) conducted in 2015-16, the district reports from National Health Mission and the Rural Health Statistics Report 2014-15 of the Statistics Division, Ministry of Health and Family Welfare, Government of India (Table 1).
Table 1: Indicators of study and their sources
| Sl.No. |
Source of Data |
|
Data Obtained |
| I |
National Family Health Survey (Round 4) |
1 |
Percent of Households with improved drinking water source |
| 2 |
Percent of families with health insurance |
| 3 |
Percent of families using family planning methods |
| 4 |
Percent of women receiving post-natal care |
| 5 |
Percent of institutional births |
| 6 |
Percent of children immunized of age upto 24 months |
| 7 |
Percent of stunted children |
| 8 |
Percent ofunderweight children |
| 9 |
Percent of wasted children |
| 10 |
Percent of women with BMI not in 18-25.5 range |
| 11 |
Percent of anaemic women |
| II |
National Health Mission |
12 |
Infant Mortality Rate |
| 13 |
Under-5 mortality rate |
| 14 |
Maternal Mortality Rate |
| III |
Rural Health Statistics& Census of India |
15 |
No. of Primary health centres (PHC) per lakh persons |
Methodology
The CHQI (Composite Health Quality Index) consists of three pillars of public health. The three pillars are (1) children’s health, (2) women’s health and (3) health infrastructure. Further, there are 15 indicators across the pillars.
After obtaining the district level data, the above indicators (Table 1) were normalized by modifying the method used for normalization in constructing the SDG-India Index by the NITI Aayog. For this, the indicators were classified into two types: (a) Positive indicators for which higher value represents better performance (indicators 3,10,11,12,13,14,15) and (b) Negative indicators for which higher value represents poor performance (indicators 1,2,4,5,6,7,8,9 ), (Table 2):
Table 2: Weighted Indicators
| Pillar No. |
Pillar |
Sl.No |
Indicator |
Weight |
Aggregate weight |
| I |
Children’s Health |
1 |
Infant Mortality Rate |
1/18 |
1/3 |
| 2 |
Under-5 mortality rate |
1/18 |
| 3 |
Percent of children immunized of age upto 24 months |
1/18 |
| 4 |
Percent of stunted children upto 6 years of age |
1/18 |
| 5 |
Percent of underweight children upto 6 years of age |
1/18 |
| 6 |
Percent of wasted children upto 6 years of age |
1/18 |
| II |
Women’s
Health |
7 |
Percent of women with BMI not in 18.5-25 kg/m2 range |
1/9 |
1/3 |
| 8 |
Percent of anaemic women |
1/9 |
| 9 |
Maternal Mortality Rate |
1/9 |
| III |
Health Infrastructure |
10 |
Percent of Households with improved drinking water source |
1/18 |
1/3 |
| 11 |
Percent of families with health insurance |
1/18 |
| 12 |
Percent of families using family planning methods |
1/18 |
| 13 |
Percent of women receiving post-natal care |
1/18 |
| 14 |
Percent of institutional deliveries |
1/18 |
| 15 |
No. of Primary health centres (PHC) per lakh persons |
1/18 |
(a) For positive indicator s:
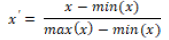
Normalized indicator value (say x’) = (Indicator value – Minimum Value) / (Maximum Value – Minimum Value)
(b) For negative indicators:
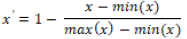
Normalized indicator value (x’) = 1- [(Indicator value– Minimum Value) / (Maximum Value – Minimum Value)].
Hence, all the normalized indicator values were multiplied by the weight assigned to them and summed up to arrive at the CHQI (Composite Health Quality Index).Each pillar has been assigned equal weight and further, each indicator within a pillar has also been weighted equally (Table 2).
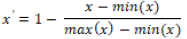
The three pillars have also been analysed separately for micro-analysis of the components of index, namely, Chid Health Quality Index, Women Health Quality Index and Health Infrastructure Quality Index The index score varies from 0 to 1, with 0 representing worst performance and 1 representing the best performance.Thus, a higher index value represents a better state of public health in that district. This data has been plotted spatially on map using the GIS software ArcGIS.
Justification for the indicators
From over 75 indicators measured in the NFHS, only 11 have been chosen for this study as per it provides the holistic view of the status of the public health system. Children are the most sensitive category within the population in terms of health. The health of children has been called ‘the most sensitive barometer of public health within a society.’ The state of children’s health represents the efforts taken by the government and community. After birth, children are not only susceptible to death but also poor health if their nutritional requirements are not fulfilled. Infant Mortality Rate represents the state of natal and infant care that children get, under-five mortality rate represents the quality of childhood care on a half-decadal time scale. Immunization plays a vital role in the healthy development of children. It prevents them from several life-threatening morbidities and death. Most of the vaccinations are given to children within the first two years of their birth. Stunting, underweight and wasting signify the nutritional status of children. Their presence leads to what is known as ‘hidden hunger’.
Historically and culturally, women in general and their health, in particular, have primarily been in a state of dismay, especially in the context of India. The health of women is intricately linked with the health of children. Healthy mothers tend to bear healthy children and nurture healthy families. However, owing to the multiplicity of factors well known such as gender discrimination and disparity, mobility inhibition, lack of accessibility to resources and self-dependence, patriarchal control, the state of women continues to be neglected. In the north-east, one finds traditions of matrilineal and matriarchal societies within tribes such as the Khasi tribes of Meghalaya. However, it is also true that nearly half of women in India suffer from multi-nutritional deficiencies, and almost 50% of them have anaemia. The indicators chosen by the writers to represent women’s health are Percent of women with BMI not in 18.5 kg/m2-25 kg/m2 range, Percent of anaemic women, Maternal Mortality Rate. The first represents the overall health, the second indicates nutritional status using a single parameter of haemoglobin levels, and third represents how secure and well-provided the women are during one of the most critical phases of their lives, i.e. pregnancy.
Health infrastructure is an essential component of public health. A welfare state, like India, should strive for building up of quality health infrastructure and ensuring its accessibility to all people equally. It will lead to prevention, mitigation and timely intervention for improvement in the health of people. The indicators chosen are : a) Percent of Households with improved drinking water source because water is a basic need and good water quality prevents many waterborne diseases, b) Percent of families with health insurance because it reduces the burden of out-of-pocket expenditure on health by families and is increasingly becoming popular for this reason, c) Percent of families using family planning methods because small families invariably can ration more resources per capita, fewer pregnancies mean less of a burden on the women and is in line with the two-child policy advocated by the National Population Policy 2000, d) Percent of institutional deliveries because they facilitate adequate medical assistance and help deal with health complications before, during and after a delivery e) Percent of women receiving post-natal care represent the availability of medical staff and care to look after women immediately in the post-pregnancy phase and f) No. of Primary health centres (PHC) per lakh population because they are the nodes of healthcare service at the grassroots levels, much needed by the rural population.
Definition of the indicators used
Percent of Households with improved drinking water source: Piped water into dwelling/yard/plot, public tap/standpipe, tube well or borehole, protected dug well, protected spring, rainwater, community RO plant.
Percent of families using family planning methods: Family planning method refers here to fecund women who are using contraception but who wish to postpone the next birth (spacing) or stop childbearing altogether (limiting).
Percent of women receiving post-natal care: Mothers who received postnatal care from doctor/nurse/LHV/ANM/midwife/ other health personnel within 2 days of delivery.
Percent of institutional births: Giving birth to a child in a healthcare institution under the overall supervision of trained and competent health personnel where there are more amenities to handle the situation to care and save the life of the child and mother is Institutional delivery.
Percent of children immunized of age up to 24 months: Children age 12-23 months fully immunized (BCG, measles, and 3 doses each of polio and DPT).
Percent of stunted children: low height-for-age, below -2 standard deviations, based on the WHO standard.
Percent of underweight children: low weight-for-age, below -3 standard deviations, based on the WHO standard.
Percent of wasted children: low weight-for-height, below -2 standard deviations, based on the WHO standard.
Percent of women with BMI not in 18.5 kg/m2-25 kg/m2 range: Excludes pregnant women and women with a birth in the preceding 2 months, 18.5 kg/m2-25 kg/m2 is the normal range of Body Mass Index or BMI.
Percent of anaemic women: Haemoglobin levels of <11.5gram per decilitre, adjusted for smoking, and for altitude in enumeration areas that are above 1,000 metres.
Infant Mortality Rate: Infant mortality rate (IMR) is the number of deaths per 1,000 live births of children under one year of age. Under-5 mortality rate: The child mortality rate, also 'underfive mortality rate', refers to the probability of dying between birth and exactly five years of age expressed per 1,000 live births. It encompasses neonatal mortality and infant mortality (the probability of death in the first year of life).
Maternal Mortality Rate: The maternal mortality ratio is calculated by dividing recorded (or estimated) number of maternal deaths by total recorded (or estimated) number of live births in the same period and multiplying by 100,000.
No. of Primary health centres (PHC) per lakh persons: Primary Health Centre (PHCs), sometimes referred to as public health centres, are state-owned rural health care facilities in India. They are essentially single-physician clinics usually with facilities for minor surgeries, too. They are part of the government-funded public health system.
Findings and Discussion
Based on the CHQI scores, the districts were classified into 6 categories (based largely on the SDG India Index categorization) (Tables 3 and 4).
Table 3: Categories of Index Score
| Sl.No. |
Index Score |
Category |
| 1 |
0.70-1.00 |
Achiever |
| 2 |
0.61-0.70 |
Front Runner |
| 3 |
0.51-0.60 |
Performer |
| 4 |
0.41-0.50 |
Aspirant |
| 5 |
0.31-0.40 |
Underperformer |
| 6 |
0.01-0.30 |
Bad Performer |
Table 4: State-wise Index Scores.
| Sl.No |
State |
ChildHQI |
WHQI |
HIQI |
CHQI |
| 1 |
Arunachal Pradesh |
0.7 |
0.56 |
0.4 |
0.61 |
| 2 |
Assam |
0.64 |
0.65 |
0.39 |
0.5 |
| 3 |
Manipur |
0.6 |
0.58 |
0.35 |
0.61 |
| 4 |
Meghalaya |
0.62 |
0.66 |
0.42 |
0.44 |
| 5 |
Mizoram |
0.63 |
0.73 |
0.47 |
0.6 |
| 6 |
Nagaland |
0.6 |
0.51 |
0.42 |
0.6 |
| 7 |
Sikkim |
0.68 |
0.67 |
0.44 |
0.65 |
| 8 |
Tripura |
0.66 |
0.67 |
0.45 |
0.55 |
*Child HQI= Child Health Quality Index; WHQI= Women Health Quality Index; HIQI= Health Infrastructure Quality Index; CHQI= Composite Health Quality Index.
Following observations can highlight on the basis of above Table:
• As a whole, the mean CHQI score of all the northeastern states is 0.56.
• The best performing state was Sikkim followed by Manipur, both infrontrunner category.
• The most underperforming state was Meghalaya.
• The district with the highest score was Aizawl, scoring 0.70 while the one with least score was Ribhoi, Mizoram, with a score of 0.37.
• In ChildHQI, Arunachal Pradesh was the best performer, followed by Sikkim. The mean score of all states was 0.64.
• The most laggard states were Manipur and Nagaland
• The best performing district was North Tripura in the Achiever category while the lowest ChildHQI score was in Udalgiri, Assam.
• In WHQI, the mean score of all states was 0.62. Mizoram was the best state for women’s health, in the achiever category, while Arunachal Pradesh got the least score.
• Best performing district was Lawngtlai, Mizoram in achiever category scoring 0.94 whereas Mokokchu in Nagaland fared the worst.
• In terms of HIQI, mean score was 0.41.
• Mizoram delivered the best infrastructure while Assam had the weakest infrastructure for public health.
• Changlang district in Arunachal Pradesh scored the highest whereas Kamrup Rural district had the poorest infrastructure.
Indicator-wise Analysis is shown in Tables (Tables 5 and 6).
Table 5: State level analysis of indicators
| Sl.No. |
Indicator |
Top performing state |
Least performing state |
| 1 |
Infant Mortality Rate |
Manipur |
Meghalaya |
| 2 |
Under-5 mortality rate |
Arunachal Pradesh |
Meghalaya |
| 3 |
Percent of children immunized of age up-to 24 months |
Sikkim |
Nagaland |
| 4 |
Percent of stunted children |
Tripura |
Meghalaya |
| 5 |
Percent of-underweight children |
Manipur |
Assam |
| 6 |
Percent of wasted children |
Manipur |
Tripura |
| 7 |
Percent of women with BMI not in 18-25.5 range |
Meghalaya |
Assam |
| 8 |
Percent of anaemic women |
Manipur |
Meghalaya |
| 9 |
Maternal Mortality Rate |
Manipur |
Meghalaya |
| 10 |
Percent of Households with improved drinking water source |
Sikkim |
Manipur |
| 11 |
Percent of families with health insurance |
Tripura |
Nagaland |
| 12 |
Percent of families using family planning methods |
Meghalaya |
Manipur |
| 13 |
Percent of women receiving post-natal care |
Sikkim |
Arunachal Pradesh |
| 14 |
Percent of institutional deliveries |
Sikkim |
Arunachal Pradesh |
| 15 |
No. of Primary health centres (PHC) per lakh population |
Arunachal Pradesh |
Tripura |
Table 6: District-wise analysis of indicators
| S.No. |
Indicator |
Top performing district |
Least performing district |
| 1 |
Infant Mortality Rate |
Imphal West, Manipur |
East Siang, Arunachal Pradesh |
| 2 |
Under-5 mortality rate |
Thoubal, ,Manipur |
Saiha, Mizoram |
| 3 |
Percent of children immunized of age upto 24 months |
South District, Sikkim |
Longleng, Nagaland |
| 4 |
Percent of stunted children |
South Garo, Meghalaya |
West Khasi Hills, Meghalaya |
| 5 |
Percent ofunderweight children |
Mokokchung, Nagaland |
Goalpara, Assam |
| 6 |
Percent of wasted children |
Mokokchung, Nagaland |
South Garo, Meghalaya |
| 7 |
Percent of women with BMI not in 18-25.5 range |
Tirap, Arunachal Pradesh |
Tinsukia, Assam |
| 8 |
Percent of anaemic women |
Champhai, Mizoram |
West Garo District, Meghalaya |
| 9 |
Maternal Mortality Rate |
Kamrup Metropolitan, Assam |
Saiha, Mizoram |
| 10 |
Percent of Households with improved drinking water source |
South District, Sikkim |
Tuensang |
| 11 |
Percent of families with health insurance |
East Siang, Arunachal Pradesh |
Senapati, Manipur |
| 12 |
Percent of families using family planning methods |
Dhalai, Tripura |
Est kameng. Arunachal Pradesh |
| 13 |
Percent of women receiving post-natal care |
South Garo, Meghalaya |
Mon, Nagaland |
| 14 |
Percent of institutional deliveries |
South District, Sikkim |
Mon, Nagaland |
| 15 |
No. of Primary health centres (PHC) per lakh population |
Upper Siang, Arunachal Pradesh |
Tirap, Arunachal Pradesh |
Other observations
• Districts in and around capital cities tend to have better state of public health.
• There generally tends to be strong correlation between linked factors as : institutional deliveries, receiving of post natal care and maternal mortality rate, institutional deliveries and infant mortality rate, immunization and under-5 mortality rate etc.
• Sikkim has delivered highly in terms of public health in general whereas Assam and Meghalaya, except the Shillong region have fared badly and need to improve their health care especially in terms of IMR, stunting, immunization and Maternal Mortality Rate (Figure 2).
Figure 2: District level distribution of Index value.
• Except Arunachal Pradesh, all other states have very low density of PHCs, with some districts even having just a single PHC. Considering that the north eastern states have more rural population than urban, the role of PHCs in ensuring good public health is of paramount importance.
Conclusion
The state of public health in the north eastern states is not very satisfactory. Nearly half of the states have Maternal Mortality Rate way higher than the national goal. The number of PHCs remains abysmally low. The incidence of stunting and wasting remain high, which indicates multiple nutritional deficiencies. The state of women’s health in Meghalaya needs to be improved. Health infrastructure across all the states needs a lot of investment. Overall, the prospects of improvement in the health and healthcare of the north eastern states are very high. The role of governments, at the central, state, regional and grassroot levels and their funding will be very crucial in attaining a high standard of public health and human capital.
References
- W.H.O (2006) Constitution of The World Health Organization.
- Winslow CEA (1920) The Untilled Field of Public Health. Science.
- Ghebreyesus TA (2017) Health is a fundamental human right.
- Draper WH (1990) Human Development Report 1990. New york: Oxford University Press.
- Conceiçao P (2019) Beyond income, beyond averages, beyond today: Inequalities in human development in the 21st century. New York: AGS.
- Aayog N (2015-16) Healthy States, Progressive India, New Delhi, India.
- NITI (2019-20) SDG India Index . New Delhi: NITI Aayog.
- Philippas D (2014) Children’s Health Index. In: Michalos AC. Encyclopedia of Quality of Life and Well-Being Research. Springer.
- Bagli S (2015) A Study of Multidimensional Poverty in North-East India. Poverty, Inequality and Health in India with Special Emphasis to North-East India.
- Sibsankar Mal, Prabhat Bhattacharya, Bikash Ghosh (2013) Consequence of health infrastructure of North East India in comparison with India. A Journal of Radix International Education and Research Consortium 7(2): 1-14.
- Rudra S (2018) Nagaland has poorest maternal and child healthcare indicators in Northeast India.
- Gogoi JK, Goswami H, Borah KC (2009) Problems of Border Areas In North East India: Implications For The Thirteenth Finance Commission. Department of Economics, Dibrugarh University, Dibrugarh.