Keywords
Placenta percreta; Conservative treatment; Additional therapy; Morbidity
Introduction
The placenta percreta is an abnormal penetration of chorionic villi in the myometrium and uterine serosa or adjacent organs. The incidence of placenta accreta has increased in recent years from 1 per 3000 deliveries in the 1980s to 1 per 300 in 2014 [1]. Although the overall incidence of placenta percreta is low (5%), the appearance of this rare disorder seems to be increasing due to the performance of more cesarean deliveries. Because of their more extensive invasion through the uterus and into surrounding tissues, percretas are associated with a higher incidence of morbidity and mortality (7%) [1].
Antenatal diagnosis is mainly based on ultrasound data and MRI techniques currently well-defined and allowed the organization of multidisciplinary therapeutic management [2].
Cases of placenta accreta managed without hysterectomy have recently been reported [3,4]. In order to preserve fertility it was proposed to leave the adherent placenta in situ at the time of caesarean section. The purpose of our study was to report the experience of our department in the conservative management of placenta percreta and to evaluate our results.
Materials and Methods
A prospective study was performed in the Department B of gynaecology and obstetric of university hospital of Charles Nicolle from January 2011 until December 2014. We identified women with a confirmed placenta percreta. Placenta accreta was diagnosed via ultrasound and magnetic resonance imaging (MRI) in the prenatal period. For these patients, a conservative approach was attempted with a close collaboration between obstetricians, anesthesists and neonatologists. Exclusion criteria were heavy haemorrhage.
Conservative treatment consisted in opening the uterus at a site distant from the placenta, and delivering the baby without disturbing the placenta. In this procedure, placenta was left in place until spontaneous resorption. Supplementary treatment sometimes followed conservative approach. Postpartum, 2- week antibiotics was given. Placental involution was monitored by a weekly ultrasound exam. If heavy haemorrhage began after conservative treatment, a secondary hysterectomy was performed.
Maternal and obstetric characteristics, postoperative complications, time to resumption of menstrual periods, desire for pregnancy, and outcomes were collected prospectively from the patients' medical records.
Results
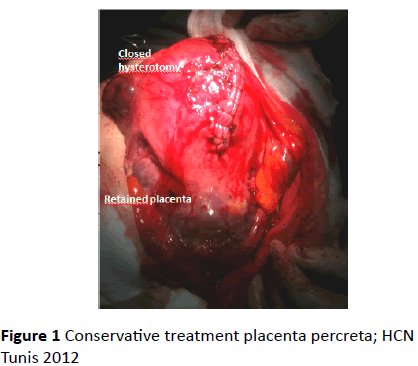
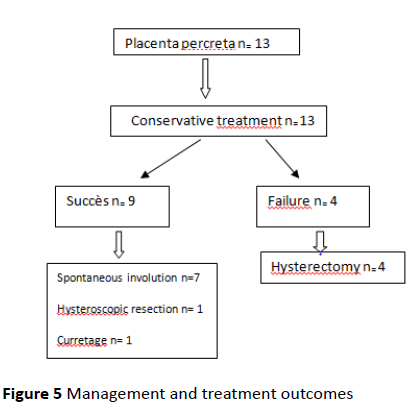
Thirty one cases (0.2%) of placenta accreta were observed in 15,633 deliveries during the study period. Of the 31 cases, 13 patients (42%) were treated by conservative management. the entire placenta was left in situ in all cases. The final diagnosis was confirmed by a clinical diagnosis of placenta percreta (Figure 1).
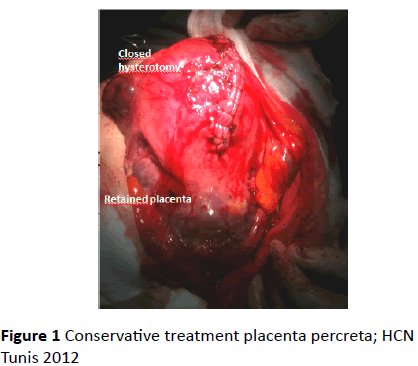
Figure 1: Conservative treatment placenta percreta; HCN Tunis 2012
The mean age was 34 years and ranged from 26 to 43 years. The average gestity was 4, the parity one was 3.2. Median gestational age at delivery was 36 weeks (it ranged from 35 to 37 weeks.
Most of the patients (93%) had an associated placenta previa. Antenatal screening placenta accreta was performed in all patients. Prenatal diagnosis was been attempted with the use of ultrasonography and MRI. Patient’s clinical characteristics are reported in Table 1.
| Characteristics |
|
| Age |
34 (26-43) |
| Previous pregnancy |
4 (2-9) |
| Parity (1-3) |
3.2 (1-6) |
| 1. Cesarean delivery |
1/13 |
| 2. Cesarean deliveries |
11/13 (84) |
| 3. Cesarean deliveries |
2/13 |
| Uterine surgery |
1/13 |
| Placenta previa |
12/13 (93) |
| Metrorrhagia |
2/13 (15) |
| Ultrasonographic suspicion of placenta accrete |
13 (100) |
| MRI suspicion of placenta accreta |
12/13 (93) |
| Gestational age at birth |
36 (35-37) |
Table 1: Patient’s clinical characteristics
During the study period, the incidence of conservative management was regularly attempted each year. Of 13 patients who underwent conservative treatment, 10 patients had an elective cesarean delivery and 3 patients had an emergency caesarean delivery. The indication of conservative treatment was operational difficulties related to invasion of serous uterine, bladder and broad ligament.
Recovery of the pfannenstiel incision was adopted in 3 cases. All caesarean sections were performed under general anesthesia. For the adjuvant treatment, prophylactic ligation of the hypogastric was performed in 7 cases and PGE2 was administrated in 3 cases. No intraoperative embolization has been carried. Additional medical treatment by Methotrexate was performed in 2 cases.
There was no bladder injury or any other pelvic organ. No patients had blood transfusion on intraoperative. No patients were transferred to intensive care unit. Treatment details are listed in Table 2.
| |
Number of cases (n=13) |
| LBHA |
7 |
| PGE2 |
3 |
| Embolization |
0 |
| MTX |
2 |
| No additional treatment |
1 |
| BLHA: bilateral ligation of hypogastric arteries |
| MTX: methotrexate |
| PGE2:prostaglandin E2 |
Table 2: Additional treatment in conservative management of placenta percreta
Table 2 Additional treatment in conservative management of placenta percreta
For this group treated conservatively, 5 patients developed fever (38%) related to endometritis in 4 cases (30%) requiring antibiotics prescriptions. One case of pulmonary embolism was reported and no cases of haemorrhage was deplored in the immediate postpartum.
The procedure was successful and did not lead to hysterectomy in 9 cases (70%).
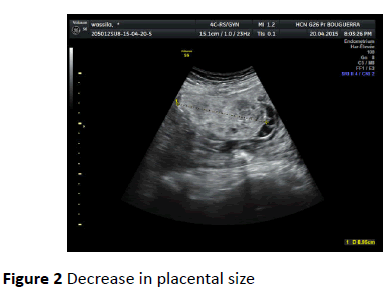
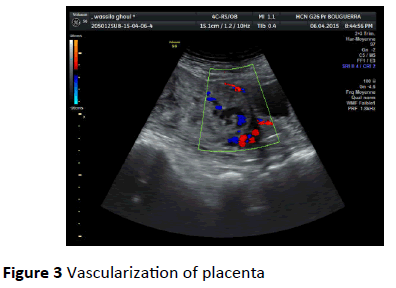
The mean length of hospitalization was 30 days. Follow-up ranged from 2 to 6 months. In this conservative group, 7 patients underwent regular weekly ultrasound examinations showing complete placental involution after 4 months. Predictive criteria of a placental resorption were a significant decrease in placental size, disappearance of the vascularization of the placenta and high resistances to the uterine Doppler (Figures 2 and 3).
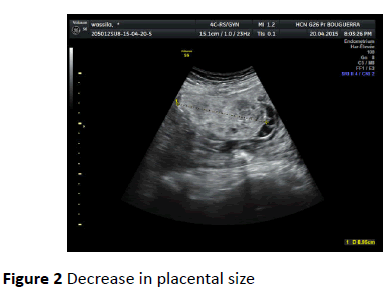
Figure 2: Decrease in placental size
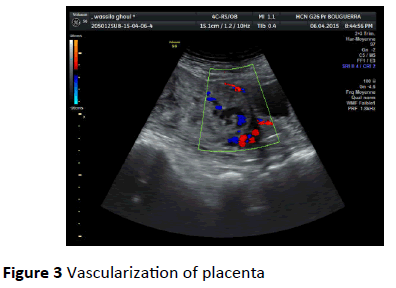
Figure 3: Vascularization of placenta
Resection under hysteroscopy was performed in an asymptomatic patient because of an ultrasound finding of placental retention n.
One patient had a vacuum aspiration for endometritis with placental residue with evacuation of necrotic tissue 60 days after delivery. In this subgroup, normal menses cycles have been reported in all cases. No women had desired a subsequent pregnancy. Five women have tubal ligations during cesarean section.
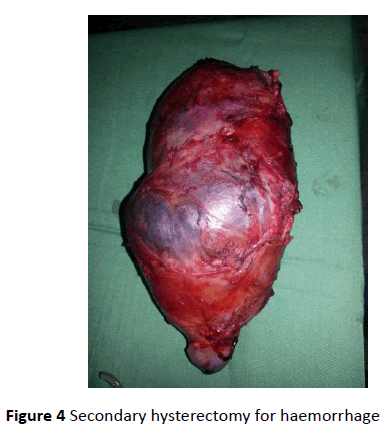
Conservative management failed for 4 patients, it is late failures occurring after an average of 53 days and had all required subsequent hysterectomies because of postpartum haemorrhage. There was a total hysterectomy (Figure 4).
Figure 4: Secondary hysterectomy for haemorrhage
It had no digestive or bladder injury. A vesicovaginal fistula was diagnosed and resolved spontaneously. Intra-operatively, the mean blood transfusion was 4 units of red blood cells. No patient had stayed in intensive care.
Management and treatment outcomes are reported on the Figure 5.
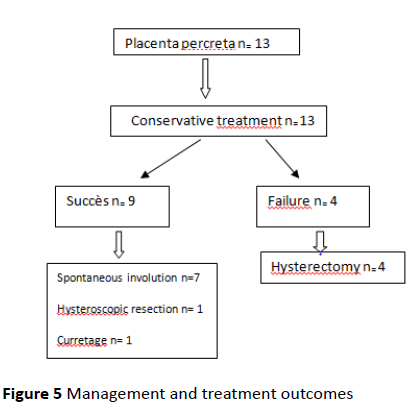
Figure 5: Management and treatment outcomes
Concerning neonatal complications, we didn’t report any fetal complications. The fetal weight at birth ranged from 3200 g to 4000 g.
Comment
Hysterectomy has long been the gold standard recommended treatment of placenta accreta [5]. In case of placenta percreta, hysterectomy is a high-risk procedure. Recently, some authors have proposed conservative treatment as an alternative to preserve fertility and to minimize damage [3-6].
The majority of these studies reported only case reports and small series. In our study, we identified 13 cases of conservative management among 35 cases of placenta accreta observed during the study period. The incidence of placenta accreta has grown in the last few decades [1]. The rate reported in our study was 1/500 deliveries. Our department is level III maternity center and could potentially increase the number of placenta accreta.
Management consists of opening the uterus at a site distant from the placenta, and delivering the baby without disturbing the placenta. Going straight through the placenta to achieve delivery is dangerous attitude, associated with more bleeding, and should be avoided. In case of placenta percreta, leaving placenta and closing appears associated with less blood loss than hysterectomy [7].
Conservative management should be planned before delivery. There is now ample evidence that prenatal diagnosis of placenta accreta, combined with elective delivery and care provided by a multidisciplinary team markedly reduces maternal morbidity and intraoperative blood loss [2,8]. The timing of elective delivery ranged from 35 to 37 weeks. For that, maternal corticosteroid administration is necessary before 34 weeks in order to make favourable neonatal outcomes.
For the adjuvant therapy, although published reports are not extensive, it appears that conservative treatment might best be combined with another treatment to avoid secondary haemorrhage. In our series, bilateral hypogastric ligation was performed in half of the cases. However, systematic recourse of this procedure is not recommended.
Post-operative embolization of uterine arteries may help to prevent excessive blood loss during follow up and to promote placental resorption [9-11]. Successfully some cases of placenta percreta managed conservatively using uterine artery embolisation were reported. Clinical success rate of this procedure is at around 86% [12].
According to a retrospective chart review which through the study of 95 consecutive patients with prenatal suspicion of placenta accreta, prophylactic uterine artery catheterization and embolization in the management of placenta accreta appeared to be feasible and safe [13]. However, this approach may be associated with complications such as uterine necrosis. In our department, we have not performed embolization postoperatively.
The utility of balloon-tipped catheters remains unclear [14]. A recent study concluded that conservative management using combined prophylactic internal iliac artery balloon occlusion and immediate postoperative uterine artery embolization may be an effective strategy to control intraoperative blood loss and to preserve the uterus in patients with invasive placenta [15].
For the Methotrexate, widely used in the treatment of ectopic pregnancy, its use as an auxiliary treatment to reduce placental mass is not well proven to date [16]. It has been reported only in isolated cases [17]. In our study, only two patients were treated with a 100 mg intramuscular injection of methotrexate immediately postpartum.
Similarly, the intraoperative sulprostoneuse is not recommended systematically [9].
In order to demonstrate the place of the various additional therapeutic, only a prospective randomized study could clearly resolve several questions. Such a study appears difficult, because its both complex and ethically unacceptable aspects.
During the period of placental involution, haemorrhage, infection and disseminated intravascular coagulation can occur. Bretelle et al. obtained with this management in 26 women, 19% of hysterectomy rate [18]. Sentilhes et al. reported on a cohort of 167 women with accreta in whom conservative management was planned before delivery. Eighteen underwent a delayed hysterectomy. Severe morbidity occurred in 10 women, and there was one death due to complications of methotrexate therapy [19].
In our study, conservative treatment failed in four cases (28.5%) and led to hysterectomy. These hysterectomies were related to secondary haemorrhage.
Endometritis is as well as frequently reported complication of conservative treatment [20,21]. In this way, prophylactic antibiotics may be helpful in the immediate postpartum period to reduce this risk [13]. We reported 2 cases treated by antibiotics.
Subsequent follow up of these patients performed weekly until complete involution of the placenta. It includes a physical examination, pelvic ultrasound and laboratory tests in search of infection (vaginal swab, C reactive protein) [13]. A psychological care may also be offered in this very anxietyproducing situation. Prolonged retained placenta may cause a delayed postpartum haemorrhage. Hysteroscopic resection is a conservative therapeutic option for placenta accreta in stable patients [22]. In our study, one patient having persistent products of conception was undergoing hysteroscopic resection with complete resolution of his symptoms.
Few publications have assessed the subsequent follow up of patients treated conservatively for placenta accreta [23,24]. Normal menses cycles and few pregnancies have been observed even after vascular ligation or embolization. The impact of conservative approach on fertility and subsequent pregnancy will require a long-term follow-up. In our study, despite the preservation of the uterus in the present study, most of the women expressed no desire for another pregnancy, probably because of the psychological trauma related to the delivery.
The risk of recurrence of placenta accreta appears to be possible. Furthermore, in case of subsequent pregnancy, placentation should be carefully monitored, particularly if the placenta is located at the same site as the previous placenta [25].
Conclusion
Our preliminary results are encouraging and show that conservative treatment may be an interesting alternative procedure in some selected patients with placenta percreta. Patients and teams must be warned about the risk of secondary complications. This risk must reserve this management to centres with experience. The impact on subsequent fertility, need to be validated in a prospective large series with long-term follow-up of patients.
References
- Morlando M, Sarno L, Napolitano R, Capone A, TessitoreG, et al. (2013) Placenta accreta: incidence and risk factors in an area with a particularly high rate of cesareansection. ActaObstetGynecolScand92:457-460.
- Ouerdiane N, Daaloul W, Masmoudi A, Othmani K, Ben Hamouda S, et al. (2015) Prenataldiagnosis of placenta accrete. Imagerie de la femme 25:204-210.
- Di Luigi G, Patacchiola F, Di Stefano L, D'Alfonso A, Carta A (2013) Placenta accreta: conservative approach. ClinExpObstetGynecol 40(4): 596-598.
- Nishijima K, Shukunami K, Arikura S, Kotsuji F (2005) An operative technique for conservative management of placenta accreta.Obstet Gynecol 105(5): 1201-1203.
- Timmermans S, van Hof AC, Duvekot JJ (2007) Conservative management of abnormally invasive placentation. ObstetGynecolSurv 62:529-539.
- Clement D, Kayem G, Cabrol D (2004) Conservative treatment ofplacenta percreta: a safe alternative. Eur J ObstetGynecolReprodBiol 114:108-109.
- Kayem G, Davy C, Goffinet F, Thomas C, Clement D, et al. (2004) Conservative versus extirpative management in casesof placenta accreta. Obstet Gynecol 104:531-536.
- Warshak CR, Ramos GA, Eskander R, Benirschke K, Saenz CC, et al. (2010) Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. ObstetGynecol 115:65-9.
- Kayem G, Keita H (2014) Management of placenta previa and accrete. Eur J ObstetGynecolReprodBiol43: 1142-1160.
- Diop AN, Chabrot P, Bertrand A, Constantin JM, Cassagnes L, et al. (2010) Placenta accreta: management with uterine artery embolization in 17 cases. J VascInterv 21(5): 644-8.
- Sentilhes L, Goffinet F, Kayem G (2013) Management of placentaaccreta. Acta ObstetGynecolScand 92:1125-34.
- Eller A, Porter T, Soisson P, Silver R (2009) Optimal managementstrategies for placenta accreta. BJOG 116:648-54.
- Bretelle F, Courbiere B, Mazouni C (2007) Management of placenta accreta: morbidity and outcome. Eur JObstetGynecolReprodBiol133(1): 34-39.
- Thon S, McLintic A, Wagner Y (2011) Prophylactic endovascular placement of internal iliac occlusion balloon catheters in parturients with placenta accreta: a retrospective case series. Int J Obstet Anesth 20(1): 64-70.
- D'Souza DL, Kingdom JC, Amsalem H, Beecroft JR, Windrim RC, et al. (2015) Conservative Management of Invasive Placenta Using Combined Prophylactic Internal Iliac Artery Balloon Occlusion and Immediate Postoperative Uterine Artery Embolization. Can AssocRadiol J 66(2): 179-84.
- Palacios-Jaraquemada JM (2008) Diagnosis and management of placenta accreta. Best Practice & Research Clinical Obstetrics and Gynaecology 22: 1133-48.
- Mussali GM, Shah J, Berck DJ, Elimian A, Tejani N, et al. (2000) Placenta accreta and methotrexate therapy: three case reports. J Perinatol 20: 331-4.
- Bretelle F, Courbiere B, Mazouni C, Agostini A, Cravello L, et al. (2007) Management of placenta accreta: morbidity andoutcome. Eur J Obstet Gynecol ReprodBiol 133: 34-9.
- Sentilhes L, Ambroselli C, Kayem G, Provansal M, Fernandez H, et al. (2010) Maternal outcome afterconservative treatment of placenta accreta. Obstet Gynecol 115: 526-34.
- Fitzpatrick K, Sellers S, Spark P, Kurinczuk J, BrocklehurstP, et al. (2014) The management and outcomes of placentaaccreta, increta, and percreta in the UK: a population-baseddescriptive study. BJOG 121: 62-70.
- Morel O, Desfeux P, Fargeaudou Y, Malartic C (2009) Uterine conservation despite severe sepsis in a case of placenta accreta first treated conservatively: 3-month delayed successful removal of the placenta. FertilSteril 91(5).
- Legendre G, Zoulovits FJ, Kinn J (2014) Conservative Management of Placenta Accreta: Hysteroscopic Resection of Retained Tissues. J Minim Invasive Gynecol 21: 910-13.
- Sentilhes L, Kayem G, Ambroselli C, Provansal M, Fernan-dez H, et al. (2010) Fertility and pregnancy outcomesfollowing conservative treatment for placenta accreta. Hum Reprod 25:803-10.
- Provansal M, Courbiere B, Agostini A, D'Ercole C (2010) Fertility and obstetric outcome after conservative management of placenta accrete. Inter J GynecolObstet 109: 147-50.
- Kayem G,Clément B, Goffinet F (2007) Recurrence following conservative management of placenta accreta. Int J GynecolObstet 99(2): 142-143.