Research Paper - (2017) Volume 3, Issue 2
Tanya Alim1*, Suneeta Kumari1, Leslie Adams2, Didier Anton Saint-Cyr1, Steve Tulin1, Elizabeth Carpenter-Song3, Maria Hipolito1, Loretta Peterson1 and William B Lawson4
1Department of Psychiatry and Behavioral Sciences, College of Medicine, Howard University, USA
2Health Behavior Doctoral Student, University of North Carolina, United States
3Assistant Professor of Community and Family Medicine, Dartmouth Psychiatric Research Center (PRC), Geisel School of Medicine, United States
4Associate Dean for Health Disparities, Dell Medical School, The University of Texas, Texas
*Corresponding Author:
Tanya Alim
Department of Psychiatry and Behavioral Sciences
College of Medicine, Howard University, Washington, D.C., USA
Tel: 202-865-3796
E-mail: talim@howard.edu
Received date: June 15, 2017; Accepted date: July 11, 2017; Published date: July 18, 2017
Citation: Alim T, Kumari S, Adams L, Saint-Cyr A, Tulin S, et al. Craving and Depression in Opiate Dependent Mentally Ill African Americans Receiving Buprenorphine/Naloxone and Group CBT (Cognitive Behavioral Therapy). Clin Psychiatry 2017, 3(2):11. doi: 10.21767/2471-9854.100042
Copyright: © 2017 Alim T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Given limited research on patient perspectives, we sought to assess craving and depression in dually diagnosed African Americans receiving Buprenorphine/Naloxone and group therapy. Nineteen subjects were recruited and 13 completed the 12 month longitudinal study. Buprenorphine/Naloxone treatment and group therapy were provided weekly. Quarterly evaluations of craving, depression and patient perspectives of treatment were obtained. Craving, depression and reported opiate use significantly declined from baseline. Depression increased slightly at 12 months. Buprenorphine/Naloxone and group therapy resulted in a significant decrease in craving, depression severity, and reported opioid use with improvement in quality of life.
Keywords
Craving; Opioid use; Depression; Buprenorphine/Naloxone; Group therapy; African Americans
Introduction
Mental illness and substance use disorders are major global public health concerns [1,2]. The co-occurrence of severe mental illness (SMI) and substance use is common with approximately 50% of people with mental illness developing a substance use disorder [3]. Specifically, individuals with an opioid use disorder have a lifetime prevalence of any mood disorder of 54.2% or higher [4,5].
Rates of substance use disorders are higher in African Americans who have SMI as compared with Euro-Americans or Latinos [6]. When SMI and substance use co-occur, they can lead to increased risk for psychiatric and substance use relapses, higher psychological distress, lower treatment retention and poor medication adherence [7,8]. Improved interventions for these clients are urgently needed, as the cost of treating cooccurring disorders is higher than mental illness alone [9], and current approaches have limited success and high rates of treatment failure [10,11].
A key component in the maintenance of substance use and relapse is the person’s craving for the drug. Craving has been defined as the subjective experience of the desire to use alcohol or drugs [12,13]. Craving has been found to be associated with depression. Zilberman, Tavares and el-Guebaly [14] found that craving scores were positively correlated with depression and negatively correlated with number of days abstinent from substance use.
In a study of patients detoxifying from alcohol in an inpatient setting, de Timary [15] found a positive correlation between depression and craving. Witkiewitz and Bowen [16] noted a strong relationship between negative affect and craving, with depressive symptomatology showing strong links to craving and substance abuse relapse. The relation between depression and substance use also results in the disproportionately higher rates of substance use relapse in individuals with affective disorders [17-19]. In other studies of depressed individuals, a strong relation was found between depressive symptoms and both craving and relapse [20-22]. Together, these studies suggest a link between craving, depression and relapse.
Opioid agonist pharmacotherapy, in combination with psychotherapy, can be clinically effective for the treatment of opioid use disorder [23]. Opioid addiction can be effectively treated with Buprenorphine/Naloxone (BUP/NAL) which was approved by the Food and Drug Administration [24]. BUP/NAL has been found to be effective in reducing craving when combined with psychotherapy [25]. Several studies also show that BUP/NAL reduces depressive symptoms as well [26,27].
Qualitative studies evaluating BUP/NAL in patients are limited. In a study examining patient perspectives on BUP/NAL treatment in opioid users in the context of HIV care, patients reported improvement in substance use problem as well as their HIV care adherence [28]. Teruya [29] evaluated retention in patients being treated with opioid agonist therapies.
Our study sought to examine impact of BUP/NAL plus group psychotherapy in dually diagnosed African Americans on mood and craving from a quantitative and qualitative perspective.
Methods
Procedures
Written informed consent was obtained from all subjects. This study was funded by NIDRR Grant H133A080063 “Building Knowledge and Capacity in the Rehabilitation and Recovery of African-Americans suffering from severe mental illness.” The study was approved by the university Institutional Review Board for the Protection of Human Subjects. Subjects were provided a $25 gift card incentive for each visit.
Study design
The study employed a longitudinal, mixed-methods approach with baseline and weekly drug toxicology tests and weekly treatment interventions. Weekly group CBT was facilitated by a clinical social worker and a psychiatrist.
Study sample
The initial study sample consisted of 19 African-Americans who were diagnosed using DSM-IV criteria for current opioid dependence and SMI, with diagnoses including Bipolar Disorder, Major Depressive Disorder (several patients also had an anxiety disorder). In this study SMI was defined as a chronic and disabling psychiatric disorder. Subjects were recruited via waiting list for BUP/NAL treatment at a hospital mental health clinic in Washington, D.C., as well as by flyer and word of mouth. After successful enrollment, subjects received psychiatric care for their mental illness at Mental Health Clinic or by community providers in Washington, D.C.
All subjects reported showing recent opioid use for at least a month before starting BUP/NAL, confirmed by positive opioid toxicology. Thirteen subjects reported using intravenous heroin and 11 reported intranasal use (5 reported both). Subjects were excluded if unable to give informed consent, using pain narcotic medications or benzodiazepines, pregnant or lactating, or not using a reliable method of birth control.
Thirteen subjects completed the study. Of the 19 subjects who began the study, 2 did not return after baseline visit. Four were dismissed from the study and referred for more intensive treatment. For the following reasons: one of the 4 subjects was on pain narcotic medication and another was prescribed both pain narcotic medication and benzodiazepines by an outside provider. The other subject attended group while extremely intoxicated and the 4th person did not attend group CBT after 3 weeks.
Assessment of psychiatric disorders: Patients were interviewed with a modified Mini International Neuropsychiatric Interview (MINI), a brief diagnostic interview for psychiatric disorders [30].
Assessment of drug dependence: Addiction Severity Index Lite (ASI) was done at baseline and 12 months assessing past 30 day and lifetime alcohol and drug use, medical, psychiatric, family/social, employment, and legal problems. The ASI Lite is correlated with the full ASI [31].
Assessment of depression: The Patient Health Questionnaire (PHQ 9), a nine item scale was used to screen for depression and monitor treatment response [32] was done quarterly. The range of scores is from 0 to 27. The severity of scores are the following: minimal depression (1 to 4); mild depression (5 to 9); moderate depression (10 to 14); moderately severe depression (15 to 19) and severe depression (20 to 27).
Assessment of craving: Intensity and frequency of craving were captured using the Brief Substance Craving Scale (BSCS) quarterly. The BSCS is a short version of the 16 item self-report instrument assessing craving for substances of abuse over a 24 hour period [33]. The range of scores reported is from 0 to 12.
Assessment of treatment outcome (total days of opiate use): The Timeline Follow-back Method (TLFB) obtains information on drug consumption and duration using a calendar method on which the client estimates alcohol/drugs used on each occasion during a specific time period. TLFB was designed for alcohol consumption but has been validated for drug use [34]. TLFB was done quarterly and drug usage was assessed in the previous 90- day time period.
Treatment adherence: Treatment adherence was defined by meeting two criteria: 1) taking BUP/NAL as prescribed and 2) positive toxicology screen for BUP/NAL for 80% of visits (Tkacz et al., 2011). Adherence to BUP/NAL was emphasized by encouraging patients to take medication throughout the study. Urine or cheek swabs were obtained weekly to assess illicit drug use and BUP/NAL adherence.
Assessment of subjective experience of co-occurring disorders and treatment: Qualitative interviews were conducted quarterly. Interviews explored subjects’ experiences of mental illness and addiction, their experience of treatment, as well as its perceived impact on recovery covariates such as housing, community integration, and social support.
Data Analysis
Statistical analysis was performed using STATA IC version 13. Analysis of variance (ANOVA) was used to compare study subjects’ mean depression and craving over the 12 months. We used generalized estimating equations (GEE) to test interaction between craving and depression across the 12 months and to account for missing data. The analyses controlled for age and gender.
Results
Patient characteristics
Table 1 presents the socio-demographic and clinical features of the sample at baseline. The initial sample included 10 females and 9 males. On average, study participants completed 11.6 years of education. 74% had a generalized anxiety disorder, 58% had bipolar disorder and 42% had major depressive disorder (several subjects had multiple diagnoses). The average duration of heroin use was 23 years, with average recent use of 13 days out of the last 30 days. There was a significant reduction in the composite ASI drug score between baseline and 12 months (0.29 to 0.12, p<0.001). The average of dose of BUP/NAL was 24 mg/6 mg per day.
| Characteristics | Total group (N=19) |
|---|---|
| Age, mean years [stdv] | 51.79 [1.88] |
| Gender, % Female (n) | 52.63 (10) |
| Religion, % (n) | |
| Protestant | 21.05 (4) |
| Catholic | 21.05 (4) |
| Islamic | 10.53 (2) |
| Other | 36.84(7) |
| None | 10.53 (2) |
| Education level, % years (n) | |
| Low to Moderate (0-10 yrs) | 21.05 (4) |
| High (11-15 yrs) | 78.95 (15) |
| Marital Status, % (n) | |
| Married | 21.43 (3) |
| Never married, widowed, divorced, separated | 78.57 (11) |
| Living Arrangements, % (n) | |
| Sexual partner + children | 5.26 (1) |
| Sexual partner alone | 10.53(2) |
| Children alone | 10.53 (2) |
| Parents | 5.26 (1) |
| Other family | 31.58 (6) |
| Friends | 15.79 (3) |
| Alone | 21.05 (4) |
| Co-morbid disorders, % yes | |
| Bipolar Disorder | 57.89 (11) |
| Anxiety Disorder | 73.68 (14) |
| Major Depressive Disorder | 42.11 (8) |
| Severe Mental Illness, % yes | 70.00 (14) |
| Living with someone with alcohol problems, % yes | 22.22 (4) |
| Living with someone using non-prescribed drugs, % yes | 22.22 (4) |
| Route of Heroin use, % (n) | |
| Oral | 3.57 (1) |
| Nasal | 39.29 (11) |
| Smoking | 7.14 (2) |
| Non-IV Injection | 3.57 (1) |
| IV | 46.43 (13) |
| Substance use in past thirty days, mean [stdv] | |
| Heroin | 12.77 [13.35] |
| Alcohol | 7.47 [5.51] |
| Methadone | 1.23 [5.51] |
| Opiates | 1.46 [5.96] |
| Barbituates* | 0.23 [1.28] |
| Cocaine | 1.58 [4.44] |
| Cannabis | 1.1 [5.47] |
| Substance use over lifetime, mean in years [stdv] | |
| Heroin | 23.00 [14.41] |
| Alcohol | 18.73 [13.87] |
| Methadone | 1.13 [3.40] |
| Opiates | 0.43 [2.19] |
| Barbituates* | 1.03 [4.09] |
| Cocaine | 8.87 [12.46] |
| Cannabis | 7.52 [14.78] |
Table 1: Characteristics of study participants (N=19) in BUP/NAL trial.
Depression severity
PHQ-9 scores declined from 18.1 at baseline (moderately severe to severe) to 8.3 (mild to moderate) at the 9 months’ follow-up (p<0.05). Absolute depression scores showed a nonsignificant increase at 12 months to 10.8 (moderate). The decline of depression severity over time among study subjects was significant (p=0.002).
Craving
At baseline subjects had an average craving score of 8.6 out of 10. Craving scores declined from 8.6 to 5.1 from baseline to month 12. Changes in craving between the 9 to 12 months’ period were not significant. The overall decline in craving from baseline to 12 months was significant (p<0.001).
Reported Total Days of Opiate Use
Figure 1 depicts total days of opiate use over time using the TLFB. Based on the TLFB (assessing the last 90 days of use) selfreported total days of opiate use declined during the study, from 73.2 days at baseline to 1 day at 9 months. The greatest reduction occurred between baseline and 3 months (73.2 to 4.5 days, p<0.001). There was an increase in use between 9 and 12 months (1 to 6.8 days, p<0.001).
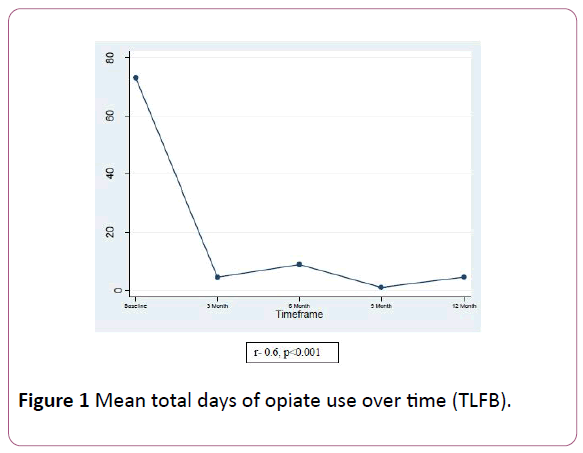
Figure 1: Mean total days of opiate use over time (TLFB).
Treatment adherence
Initially, the total sample size for this study was 20 patients, however, lab data for 7 participants were not included in final analysis due to early termination or missing data. We calculated percentages of positive toxicology to drugs at baseline and at quarterly visits.
Based on our definition of adherence stated earlier, 53% (7) of the patients were compliant with BUP/NAL treatment over time and 92% were positive for BUP/NAL at quarterly visits.
The results from the toxicology data show those participants who were non-compliant with BUP/NAL treatment also used other illicit drugs (cocaine, marijuana, PCP) in addition to opioids. Table 2 shows a summary of the results.
| Toxicology Result | % (N) |
|---|---|
| Mean Quarterly BUP/NAL Positive | 92.30% (12) |
| Adherent with BUP/NAL Treatment | 53.84% (7) |
| Opioid Positive (Codeine, Morphine) | 46.15% (6) |
| Cocaine Positive | 38.46% (5) |
| Marijuana Positive | 23.07% (3) |
| PCP Positive | 7.69 % (1) |
Table 2: Toxicology result.
Subjective experiences of participants
Subjects reported a decline in craving frequency and intensity over the course of the study. Prior to this change many subjects reported frequent substance use as part of their daily routines. Subjects described heroin craving at baseline as pervasive in their daily lives before entering the study.
At the 3 and 6 month follow-up subjects described a decline in many of the thoughts associated with opiate use and the shifting of their priorities towards recovery. One participant stated, “It (Suboxone) stopped my cravings, my desire to use. It helps a lot with the withdrawal symptoms of the opiates. And you really don’t think about using that much”. Subjects noted some side effects of BUP/NAL that were a barrier to its use, including dry mouth, headache and lack of energy.
By 9 and 12 months, qualitative responses mirrored the quantitative reductions in craving with a reduced overall need for opiates and a more positive approach towards recovery, with more upbeat tone and attitude. Subjects also reported increased clarity of thinking over time and less intrusive thoughts regarding substance use.
Two subjects spoke about their progress related to craving in the final months of the study. One stated, “It’s (Suboxone) keeping the desire to use, it’s keeping me away from it, I don’t think about it, I’m not tempted anymore, I’m taking my Suboxone and I’m happy. Don’t want it (heroin), taking away the dope sickness in the morning time. I have happy feelings, it has affected tremendously, I don’t have the desire very, very, very, very less craving, so it’s no, I don’t want it, I don’t crave for it that world is gone”
Another stated, “Everything is alright with me now, I’m taking my medication as prescribed. I don’t do it (heroin) anymore and I feel good about that. Suboxone helps me with my drug use and my thoughts are clear. My energy is not where I want but it’s much better.”
In addition to noting a reduction in craving, many subjects noted increased hope of recovery from substance use. Subjects who completed 12 months also attributed their reduction in opiate use to family support and religious influences. As subjects began to have reduced craving, employment was mentioned more frequently as a method of improving overall recovery. Many felt that having a stable job would remove them from the tempting environments that initiated substance use and further reduce cravings.
Generalized Equation Modeling and Correlation Analysis
Higher craving scores and depression severity were positively associated, suggesting that improving mental health may be linked to decreased opiate craving or the treatment intervention was effective for both (r=0.63, p<0.001, Figure 2). Crude GEE analysis displayed a significant association between craving score and depression (β=0.22, p<0.001). After adjustment, results of the GEE analysis supported the association between lower craving scores and observed decreases in depression severity (β=0.23, p<0.001). Both age and gender had a nonsignificant impact on craving score.
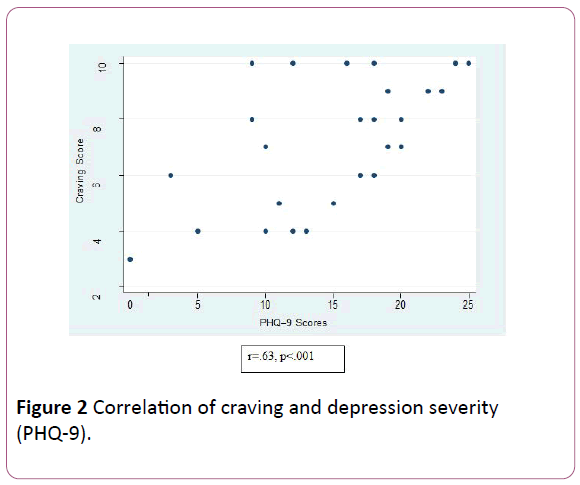
Figure 2: Correlation of craving and depression severity (PHQ-9).
Discussion
Craving scores and depression ratings declined significantly from baseline to 12 months overall. Moreover, they were correlated and both were associated with a decrease in substance use. A slight increase in craving, depression and use of opioids was observed from 9 months to 12 months. Selfreported drug use reported between months 9 and 12 on TLFB is consistent with our preliminary drug toxicology results. While we are uncertain of the cause of this increase, it may be consistent with the phenomenon of “slipping” in recovery from drug use [35-37]. The finding that an increase in craving was associated with an increase in depression is consistent with Zilberman [14,21], de Timary [15] and Witkiewitz and Bowen [16]. ASI scores showed improvement in drug use. These results suggest that both medication assisted therapy and psychotherapy can be an effective treatment for dually diagnosed African American patients.
Limitations
The study had several limitations. The sample for this study is drawn from the Metropolitan Washington, D.C. area and is African American, thus results may not be generalizable to other outpatient settings where patients receive BUP/NAL maintenance treatment, to non-African Americans, or to populations in suburban and rural areas. Additionally, due to the small sample size, comparative analyses were underpowered. Given these limitations, it is important not to understate the significance of these findings.
To our knowledge, this is the first study that preliminarily examined quantitative and qualitative factors associated with the treatment of dually diagnosed African Americans on BUP/NAL and group psychotherapy. Based on the findings from this study, future well-designed, larger sampled, prospective studies may help to better understand mental health and substance use recovery of individuals with mental illness and opioid use disorders in African Americans and other minority groups to determine if these differences are race specific and if these results are persistent. The results may also generalize to non-minority populations, whose use of opioids has become an increasing challenge.
Acknowledgements
“Building Knowledge and Capacity in The Rehabilitation and Recovery of African-Americans Suffering from Severe Mental Illness: The Dartmouth-Howard Collaboration” (NIDRR RRTC H133A080063; PI: Whitley), Rebeka Nazneen, Samuel Odedokun, Ali Raza and Mental Health Clinic staff.
Disclosures
Drs. Saint-Cyr, Tulin, Carpenter-Song report, Ms. Adams and Ms. Peterson have no financial relationships with commercial interests. Dr. Alim had a financial relationship with Otsuka Pharmaceutical, Inc. Dr. Lawson had a financial relationship with Merck, Inc. and Ostuka Pharmaceuticals, Inc. The authors have no additional income to report.