Original Article - (2019) Volume 20, Issue 1
1Yale New Haven Health Bridgeport Hospital, CT, USA
2Bassett Healthcare, NY, USA
3Sir Gangaram Hospital, Delhi, India
Received November 25th, 2018 - Accepted January 10th, 2019
Objective The purpose of the study is to select & assess the effectiveness of computed tomography Guided percutaneous drainage in patients with pancreatitis according to the clinical and imaging parameters.
Materials and Methods The study was performed from January 2012 to January 2017. The study included 126 consecutive patients (103 men and 23 women; median age 39 years) with necrotizing pancreatitis who underwent percutaneous catheter drainage via computed tomography guidance and were evaluated according to the clinical criteria, radiological scores, drainage and catheter characteristics, and complications. A retrospective review of our cross-sectional interventional radiology database over 60 months (5 years) identified all patients who underwent primary computed tomography -guided percutaneous drainage for acute necrotizing pancreatitis.
Results Successful percutaneous drainage outcome was achieved in 108 of 126 patients (85.7%). No surgery was required in 95 patients (75%). Of these 108 patients, 13 patients had the liquefiable part of the collection drained by percutaneous drainage, but the phlegmon caused persistent sepsis, and had to undergo elective surgical necrosectomy. Rest of the 18 patients did not have a successful outcome on percutaneous drainage; of these, 16 patients had treatment failure on percutaneous drainage then surgery was performed, and 2 patients passed away with treatment failure on percutaneous drainage and surgery. The procedurerelated complications were observed in six patients of which one had hemorrhage due to the catheter eroding the vessel and five had a pancreatico-cutaneous fistula. Of the total 126 patients, 110 patients were managed as outpatients with regular clinic visits.
Conclusion Percutaneous catheter drainage is a safe and effective technique for treating infected acute necrotizing pancreatitis. Appropriate selection of patients should be performed to maximize the benefit of percutaneous procedures. Treating necrotizing pancreatitis requires dedicated multidisciplinary team efforts from the physicians, surgeons, radiologist and the drain management team.
Infectious pancreatic necrosis virus; Pancreatitis, Acute Necrotizing
CT computed tomography; ERCP endoscopic retrograde cholangiopancreatography; FNAB fine needle aspiration for bacteriology; PCD percutaneous drainage
Acute necrotizing pancreatitis accounts for 10-15% of all cases of acute pancreatitis. It is frequently accompanied by a systemic inflammatory response syndrome and multisystem organ failure and occasionally by infected necrosis [1, 2]. Depending on the presence or absence of necrosis, acute collections in the first four weeks are called acute necrotic collections or acute peripancreatic fluid collections. Once an enhancing capsule develops, persistent acute peripancreatic fluid collections are referred to as pseudocysts; and acute necrotic collections, as walledoff necrosis. All can be sterile or infected. The revised classifications are used to standardize the terminology among the radiologists, gastroenterologists, surgeons, and pathologists to facilitate treatment planning and enable precise communication among different departments and institutions [3].
The study was performed from January 2012 to January 2017. There were 126 consecutive patients (103 men and 23 women; median age 39 years) with necrotizing pancreatitis who underwent percutaneous catheter drainage via CT guidance and were evaluated according to the clinical criteria, radiological scores, drainage and catheter characteristics, and complications. A retrospective review of our cross-sectional interventional radiology database over 60 months (5 years) identified all patients who underwent primary CT-guided percutaneous drainage (PCD) for acute necrotizing pancreatitis. Assessment of the patient's clinical condition at initial percutaneous CTguided PCD was based on criteria set forth by the revised classification of Acute Pancreatitis – 2012, revision of Atlanta classification, 1992. The revised classification identifies early and late phases of the disease and classifies into mild, moderate and severe acute pancreatitis. The mild acute pancreatitis has no organ failure, no local or systemic complications. The moderate acute pancreatitis has transient organ failure or local complications or exacerbation of co-morbid diseases. The severe acute pancreatitis has persistent organ failure for more than 48 hours [3]. The initial CT findings were calculated according to the Modified CT Severity index. The Modified CT Severity Index is a scoring system that incorporates the extent of pancreatic necrosis (none, <30% or >30%) along with peripancreatic inflammation (presence or absence of fluid collections).
Procedures
Referral for radiological intervention was based on suspicion of infection raised by fever, leucocytosis, renal or cardiac compromise or general clinical deterioration refractory to conservative medical care. The decision for PCD was always multidepartment based on referral from the clinical team for persistent sepsis, and departmental guidelines according to the American College of Radiology appropriateness criteria with radiological imaging suggesting a liquefied drainable collection, rapidly enlarging collections, collections larger than 5 cm, collections causing obstruction and infected collections [4]. Infection in the collection was assessed on the imaging picture (collection with gas or the collection density has higher Hounsfield Units than water) and in indeterminate cases with prior needle aspiration. The Seldinger technique was systematically used to place a catheter in each of the necrotic collections via the most direct transperitoneal route, avoiding intervening bowels and solid organs. One or more multiperforated double-sump 14- to 16- French catheters were placed to aspirate the cavity fluid and to start with continuous irrigation with 1 L/drain/day of normal saline. Later the new larger catheter was inserted after sequential dilation. The goal was to increase the diameter of the catheter to a maximum of 28–32 French large-bore catheters whose distal holes were expanded manually (Sherwood, Argyle) and additional holes made where ever required. As for the initial drainage, continuous and abundant daily irrigation was initiated, ranging from 0.5 to 1.5 L/drain/day of normal saline, depending on the size of the collection. The decision to remove the catheters and stop the drainage was based on clinical improvement (i.e., control of the sepsis and hemodynamic stability), resolution of the necrotic cavity on CT scan and when the amount of drain fluid was less than 20 mL/day. The mean time between presentation with pancreatitis and the first interventional procedure was 25 days (range, 12-65 days).
Patient Outcome
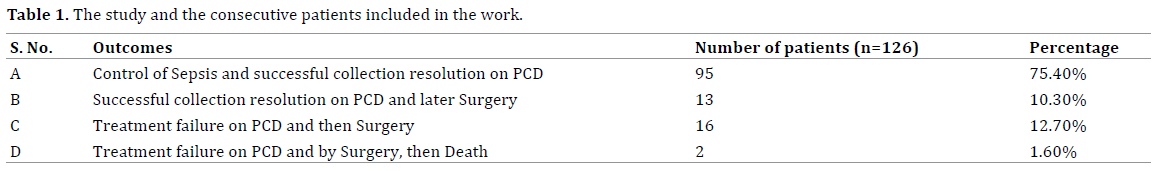
Patient outcome was categorized into four groups:- control of sepsis and successful collection resolution on PCD (A); successful collection resolution on PCD but later Surgery (B); treatment failure on PCD then Surgery (C); treatment failure on PCD & Surgery then Death (D). Control of sepsis and successful resolution on PCD, was defined as normalization of vital signs, resolution of leukocytosis and complete resolution of the collection with less than 10 ml daily drain output. The successful resolution on PCD and later surgery, was defined as complete resolution of the collection but, persistent sepsis likely secondary to infected phlegmon leading to surgery. Treatment failure on PCD and then surgery, was defined as incomplete resolution of collection or multiple inaccessible loculated collections not amenable to PCD drainage and persistent sepsis warranting surgery. The treatment failure on PCD and the surgery and death, was defined as incomplete resolution of the collection on PCD and severe sepsis not controlled by surgery ultimately leading to death. The total length of hospital stay, length of hospital stay after the initial percutaneous catheter drainage procedure and the number of days elapsed before surgical debridement was calculated. Cause of death and interval between interventional procedure or surgery and patient death were recorded. Complications related to the PCD interventional procedures were recorded as hemorrhage, Pancreatico – cutaneous Fistula, Pancreatico – enteric Fistula, Pancreatic Abscess.
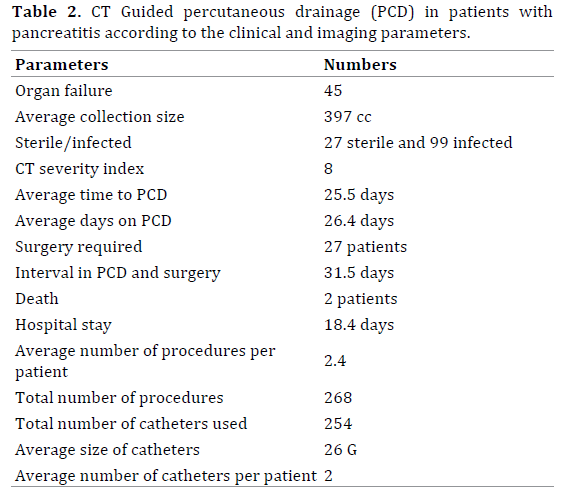
The successful drainage outcome is grouped into, control of sepsis by PCD or complete resolution of liquefied collection by PCD or stabilization of patient for elective surgery, if needed. Successful PCD outcome i.e. collection resolution was achieved in 108 (A+B) of 126 patients (85.7%). No surgery was required in 95 patients (A) (75%). Of these 108 patients, 13 patients (B) had the liquefiable part of the collection drained by PCD, but the phlegmon caused persistent sepsis, and had to undergo elective surgical necrosectomy, however, PCD helped in stabilizing these patients and reducing the septic load in the body for better surgical outcome. Rest of the 18 patients did not have a successful outcome on PCD; of these, 16 patients (C) had treatment failure on PCD then surgery was performed, and 2 patients (D) passed away with treatment failure on PCD and surgery. Moderate pancreatitis was observed in 102 patients and were managed with PCD and surgery was not avoided. Severe pancreatitis was observed in 24 patients, of those, 8 patients were stabilized with PCD and elective surgery was performed to remove non-liquefied infected phlegmon; 16 patients had treatment failure on PCD and had to undergo surgical necrosectomy; and 2 unfortunately had treatment failure on PCD and with surgery and died. The procedure-related complications were observed in six patients of which one had hemorrhage due to the catheter eroding the vessel and five had a pancreatico-cutaneous fistula. None of these complications were lethal. Pancreatico-enteric fistula developed in 3 patients and was not procedure related. They underwent surgical management. Of the total 126 patients, 110 patients were managed as outpatients with regular clinic visits. The major causes of acute pancreatitis were cholelithiasis; alcohol, ERCP, hypertriglyceridemia, autoimmune, trauma and idiopathic. The detailed results are listed in Tables 1, 2.
The mainstay of treatment of patients with acute necrotizing pancreatitis traditionally has been surgical debridement, however, morbidity with surgery has been between 43%-89% and mortality between 9%-39% [5]. This high rate has been largely attributed to the presence of comorbid medical conditions, including multisystem organ failure, derived from a systemic response to pancreatitis. Despite the availability of several clinical (Ranson criteria, Acute Physiology and Chronic Health Evaluation II score) and radiologic (Balthazar scoring system, modified CT severity index) grading systems, accurate prediction of outcome and best treatment of patients with acute necrotizing pancreatitis remains difficult. The risk of infection increases with the duration of the disease, reaching a peak during the third week with an incidence rate of 71% [6, 7]. Clinical, biologic, and radiologic signs are not specific enough to reveal infection of the necrosis. Many recent studies suggested that routine laboratory parameters like blood urea nitrogen, hematocrit, procalcitonin, C-reactive protein, and creatinine have a significant association in predicting the occurrence of infected pancreatic necrosis secondary to necrotizing pancreatitis [8, 9]. Aspiration and culture can provide bacteriologic confirmation of infection with both high sensitivity and specificity [10]. It is generally accepted that, in IPN, the infected non-vital solid tissue has to be removed to control the sepsis. Surgical necrosectomy has been the preferred treatment of years, with very variable mortality rates ranging from 3% to 42% [11]. Common complications of necrotizing pancreatitis are a pancreatic abscess, pancreatico-cutaneous fistula, pancreatico-enteric fistula, and hemorrhage. The pancreatic abscesses, can be treated with debridement and lavage. The pancreatico-cutaneous fistula results when the pancreatic secretions leak through the drain site or wound. The role of percutaneous catheter drainage in such cases is to help closure of fistula with drainage of fluid collection. Octreotide helps in reducing exocrine pancreatic secretions in cases of pseudocyst recurrence, pancreatic fistula from percutaneous drainage, or elective treatment to restrict pancreatic drainage [12, 13]. Pancreatico-enteric fistula, is leakage of pancreatic secretions into the bowl, either duodenum or colon. These can be managed with transpapillary stenting of disrupted pancreatic duct or surgery. Life-threatening hemorrhage into the gastrointestinal tract, retroperitoneum, or peritoneal cavity complicates acute pancreatitis in only 1–3% of patients. CT angiography and digital subtraction mesenteric angiography can detect the bleeding site in approximately 80% of cases and arterial embolization can achieve definite hemostasis in 35–50% and helps stabilize critically ill patients to permit elective surgery [14].
PCD of IPN is a well-recognized minimally invasive alternative treatment to primary surgical necrosectomy. Freeny et al. first described a homogeneous group of 34 patients exclusively treated by PCD for IPN using precise definitions of necrosis and infection. They recorded a clinical success rate of 47% and were able to identify multiorgan failure and central necrosis on CT as two predicting factors of poor response to catheter drainage [15]. The clinical success and mortality rely mainly and strongly on the commitment and the close cooperation among radiologists, surgeons, gastroenterologists, and intensivists who are willing to take care of such patients.
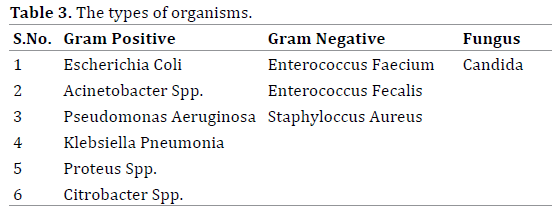
Image guided PCD has been found to be an effective alternative to surgical debridement in the treatment of selected patients with infected pancreatic necrosis. Wasler et al. has evaluated the clinical utility of CT-guided PCD in patients with sterile pancreatic necrosis and concluded no benefit in draining sterile collections versus simple aspiration, however, there is increased risk of bacterial colonization [16]. It is conceivable, however, that a patient with sterile necrosis whose condition continues to deteriorate despite aggressive supportive therapy may also benefit from percutaneous catheter drainage [17] (Figures 1, 2). In infected pancreatic collections, the most common gram-negative organism isolated was Escherichia Coli and the most common gram-positive organism was Enterococcus Faecium. Few patients had polymicrobial infection [18]. The types of organisms isolated are included in Table 3.
In our study, the sterile necrosis was found in 21% of patients and this did not correlate with patient outcome. This observation supports the hypothesis, substantiated by other investigators, that multisystem organ failure is a more reliable indicator of poor patient outcome and severity of severe pancreatitis than is the presence of infected necrosis [19]. Our study also had similar outcome with worse prognosis and multiple procedures in patients with severe pancreatitis secondary to multiorgan failure. These multiple procedures may be secondary to multiple loculated collections or persistent infected collections or slow liquefaction of the pancreatic necrosis and phlegmon not amenable to catheter drainage. Vigilant follow-up, including daily irrigation of pancreatic cavities with the assessment of the patient's vital signs, WBC count, and catheter drainage output is needed. Each catheter should be irrigated with sterile saline solution at least once daily. Abdominal CT should be performed periodically on the basis of clinical status and amount of drainage to check for residual and undrained fluid collections. The CT findings help determine adequate drainage, development of additional non-communicating collections or complications.
Several interventional therapy regimens, including endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy, fine needle aspiration for bacteriology (FNAB), percutaneous or endoscopic drainage of peripancreatic fluid collections, pseudocysts, and late abscesses, as well as selective angiography and catheterdirected embolization of acute pancreatitis associated bleeding complications have been well established as diagnostic and therapeutic standards in the management of acute pancreatitis. The risk of infection increases with the extent of intrapancreatic and extrapancreatic necrosis [17]. The mortality for sterile necrosis is low and can usually be successfully treated by a conservative approach, although surgery might be required for late complications or persistent severe pancreatitis [20]. The mortality rate for patients with infected pancreatic necrosis is higher than 20%, and up to 80% of fatal outcomes in acute pancreatitis are due to septic complications [21]. Freeny et al. developed a technique of percutaneous drainage which not only drained infected necrosis passively but included necrosectomy by adding aggressive irrigation through large bore percutaneous catheters (28 F) [15]. Some centers described combined percutaneous retroperitoneal necrosectomy, fragmentation of necrotic pancreatic and peripancreatic tissue with a snare catheter and Dormia baskets, continuous lavage of the cavity, and repeated bronchoscopic visualization of the cavity to successfully treat and avoid surgery in a patient [22]. In our patient population large bore 20–32 F catheters were placed under CT guidance, with a retroperitoneal approach from the left side or the most accessible route. The necrotic and solid material was fragmented and removed actively with aspiration and irrigation of the cavity was performed using up to 2-3 liters of normal saline solution per day and additionally, manual aspiration of solid material was performed on a daily basis till the time patients were in the hospital (Figure 3). This helped in reducing the infected material from the abdominal cavity and in reducing the leucocytosis. Many times the catheters needed to be replaced during irrigation procedures as large chunks of infected fat necrosis would get occlude the catheters. The replacement of the catheters was easy as these chronic catheters had epithelized tracts which don't collapse easily. Similar methods have been described in the literature.
Figure 3. Axial CT images showing pancreatic tail collection with large bore (28 Fr) catheter within it (Solid white arrow). Part of the Pigtail catheter (14 Fr) visualized in the anterior aspect of the collection (Hollow white arrow) used for irrigation purposes. Also visualized is the part of the nasojejunal tube in the duodenum (Solid black arrow).
In patients with treatment failure with PCD, another method of treatment is with double catheter lavage along with percutaneous flexible endoscopic debridement which may prevent surgical debridement [23]. Some researchers suggested that endoscopic transmural drainage of walled off necrosis with multiple stents to be safe and effective in avoiding direct endoscopic necrosectomy [24, 25].
To our knowledge, our study is the largest reported to date, to assess the clinical utility of CT-guided percutaneous catheter drainage in patients with drainable symptomatic pancreatic necrosis. Our study had few limitations, including the retrospective nature, the variability of experience among the interventional radiologists and surgeons involved in the treatment of these patients. There is a concern regarding the hospital stay of these patients related to repeated procedures and subsequently an increase in the length of hospital stay with the minimally invasive procedures, however, we could manage most patients on an outpatient basis. Once the drain output reduces and sepsis is controlled, the patients were discharged with the drainage catheter connected to stoma bag for easy care at home. The patients were educated about the drain care and monitoring the drain output on a daily basis and advised to report to the emergency room if the drain output falls abruptly (suggesting drain blockage) or the collection becomes hemorrhagic or they develop signs of sepsis. The patients were followed with regular visits to the gastroenterology or interventional radiology clinic. In the clinic the dedicated drain care team would take care of dressing changes, suturing the dislodged drain sutures and monitor the output (steadily decreasing or increasing). We were able to manage 110 out of 126 patients on an outpatient basis with regular visits to the clinic. No complication related to outpatient management was reported.
Percutaneous catheter drainage is a safe and effective technique for treating infected acute necrotizing pancreatitis. Appropriate selection of patients should be performed to maximize the benefit of percutaneous procedures. Treating necrotizing pancreatitis requires dedicated multidisciplinary team efforts from the physicians, surgeons, radiologist and the drain management team. Many patients can be managed on an outpatient basis reducing the hospital stay and the healthcare cost. The patient, the referring physician, and the radiologist must be ready to handle the number of catheters, the catheter changes, multiple imaging scans, and the duration of drainage.
The authors have no conflicts of interests to declare.