Key words
cultural barriers, diabetes, effective diabetes care delivery, ethnic minority groups, health workers
Introduction
Diabetes is a long-term, serious and challenging metabolic condition and a major health issue worldwide. Although diabetes affects every society, some populations are particularly susceptible but also lack understanding of the condition (Baradaran and Knill Jones, 2004; International Diabetes Federation, 2009; Alam et al, 2012). Evidence suggests that, where members of susceptible populations are in the minority, they may not receive equitable diabetes care. This is attributed to a mixture of cultural factors and some service providers’ lack of cultural competence (Hawthorne et al, 1993; Narayan and Rea, 1997; Cone et al, 2003; Brown et al, 2002; Zeh, 2010; Zeh et al, 2012; Mainous et al, 2007). The National Service Framework for Diabetes stipulates the minimum standards of diabetes care to be offered to all patients, irrespective of ethnicity, language, culture, religion, gender, disability, age and location (Department of Health, 2001). Healthcare practices should be designed to ensure that health workers take into account the individual patient’s background and deliver tailored services (Cone et al, 2003; NHS Health Scotland, 2004). However, few studies have explored the effects of cultural and linguistic barriers which may compromise the quality of care delivered to members of ethnic minority groups with diabetes (Davies, 2006; Hill, 2006; Fleming and Gillibrand, 2009). Very little is known about how these barriers may operate in particular societies, and some service providers do not appear to appreciate the nature of these barriers or how they may prevent members of ethnic minority groups from receiving patient-centred diabetes care (Department of Health, 2001; Roberts, 2007; Wilson et al, 2012). A better understanding of these cultural issues may guide healthcare commissioners and clinical commissioning groups (CCGs) to reconfigure diabetes services in primary care, which may improve both care service engagement and outcomes in minority populations (NHS Health Scotland, 2004).
Culture is a shared and dynamic phenomenon displayed by the behaviours and attitudes of a social group, which remains difficult to interpret, but requires a good understanding by health workers (Naeem, 2003). In this review, culture is defined broadly as a shared system of values, beliefs, identities, traditions, behaviours, and verbal and non-verbal patterns of communication that bind a group of people together and differentiate them from other groups (Salimbene, 1999). It encompasses beliefs, language, social norms and values, including practices which can create a sense of social support and belonging for individuals who share the same core beliefs. These can both facilitate and impede health coping styles, access to and utilisation of healthcare services, and implementation of professional advice. This study focused on the cultural barriers to accessing and use of diabetes services. In this review, the term ethnic minority group refers to a population group with an ethnic origin different from that of the majority population of the host country (Bulmer, 1996; Modood and Berthoud, 1997).
Scoping searches identified 10 reviews that reported cultural barriers among members of ethnic minority groups with diabetes. Two were systematically conducted reviews (Brown et al, 2002; Fleming and Gillibrand, 2009) and eight were literature reviews with some methodological flaws, for example, reviews with no inclusion criteria (Hawthorne et al, 1993; Davies, 2006; Hill, 2006; Gohdes, 1988; Brown, 1997; Oldroyd et al, 2005; Greenhalgh, 1997, 2008) and single-authored reviews (Davies, 2006; Gohdes, 1988; Brown, 1997; Greenhalgh, 1997, 2008; Hill, 2006). Although these reviews provided some insight into cultural barriers, the following two questions seemed to have received less attention. The present systematic review aimed to address these.
1 What specific cultural barriers impede members of ethnic minority groups from receiving effective diabetes care services, and how do they do so?
2 What can be done to minimise these cultural barriers?
Methods
Design, search strategy, data sources and eligibility
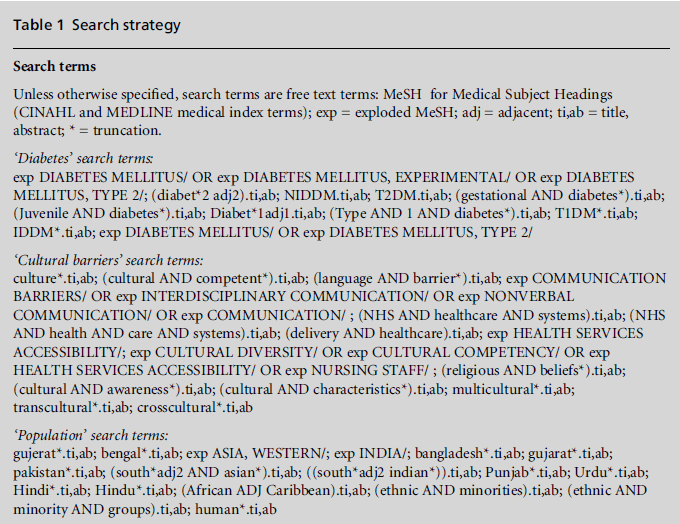
This is a systematic review, which included qualitative, quantitative andmixed methods study designs. CINAHL and MEDLINE databases were searched from inception to September 2011 using the search terms listed in Table 1. In addition, searches were conducted using Cochrane and DARE databases, two NHS Evidence specialist libraries based at Warwick University for diabetes (www.library.nhs.uk/diabetes) and for ethnicity and health (www.library.nhs.uk/ethnicity), and Warwick Medical School Research Publications from 2004 to 2011 (https://www2.warwick.ac.uk/fac/med/ staffintranet/staffresources/researchpublications/n = 1) and diabetes and behavioural change research (n = 1) were contacted for advice and to identify additional studies. The journal Diabetes Primary Care was hand searched as these articles were relevant to our topic but not accessible via PubMed or other major databases.
The inclusion criteria were as follows:
• Participants: children or adults with any type of diabetes, provided that they were an ethnic minority population in the country of study.
• Design: observational studies using qualitative or quantitative methods. Randomised controlled trials and quasi-experimental studies are deliberately excluded from consideration in this paper, as they are included in another published review using the same search strategy (Zeh et al, 2012).
• Setting: participants were recruited from any setting.
• Reporting: studies were included if they reported on cultural differences and data extracted from themes that explored any cultural barriers.
• Only primary published studies with no language restriction were included.
The screening and mapping exercise for the papers identified as a result of the search strategy (see Table 1) identified two issues, namely cultural barriers preventing members of ethnicminority groups fromaccessing effective diabetes care services, which is the focus of this review, and culturally competent healthcare interventions in ethnic minority groups with diabetes, which has been published elsewhere (Zeh et al, 2012). We found that ‘any structured intervention, tailored to ethnic minority groups by integrating elements of culture, language, religion, and health literacy skills, produced a positive impact on a range of patient important outcomes’ (Zeh et al, 2012, p. 1237). This strengthens the case for further exploring and understanding specific cultural barriers to diabetes healthcare provision.
Selection criteria
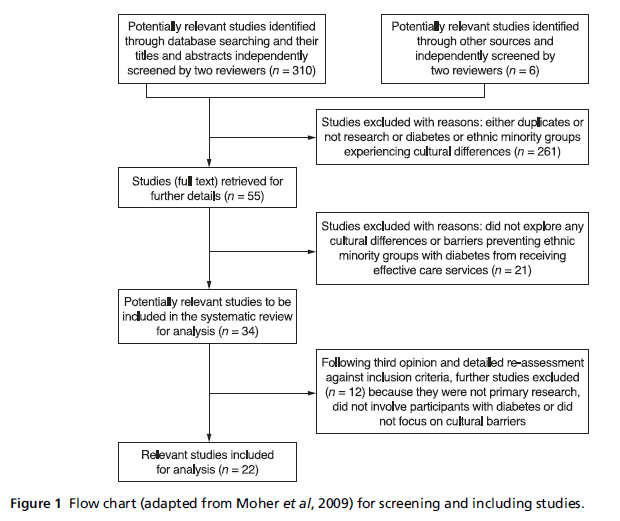
All citations were downloaded into Endnote Web and duplicates removed. All types of cultural and linguistic themes from any study involving any ethnic minority group with any type of diabetes in any setting globally were included. The titles/abstractswere independently scrutinised for eligibility by two reviewers (PZ for 100% of all papers, and JS or HS for 50% of the papers) using the inclusion criteria, and disagreements were resolved through discussion and a third opinion (JS or HS or AMC). Cohen’s kappa was used to test the screening process inter-coder reliability and to calculate agreement levels. Cohen (1960) sets a threshold of 0.85 as representing a very high level of agreement, whereas Landis and Koch (1977) stipulate limits of greater than 0.61 as a substantial agreement and greater than 0.81 as a perfect agreement. The Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) flow diagram details the results of the screening and selection processes (see Figure 1) (Moher et al, 2009).
Data extraction and quality assessment of studies
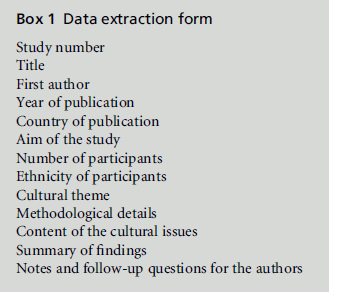
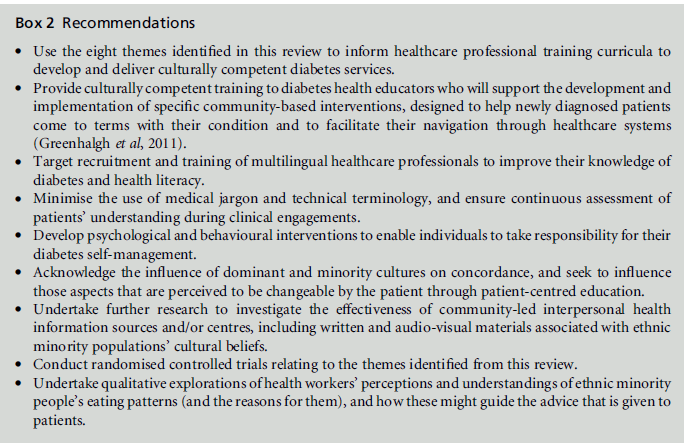
One reviewer (PZ) read and re-read each of the full included publications to understand how cultural barriers hindered the studied populations from accessing effective diabetes care services within the research settings. He extracted data using a revised data extraction form (Zeh et al, 2012; see Box 1). This form was piloted by three reviewers on three random included papers by cross-checking independent notes for consistency. The methodological quality of the qualitative studies was assessed using Popay et al (1998) and Jadad et al (1996) for quantitative and Creswell and Plano Clark (2007) for the mixed method research studies (see online Tables S1S3). Individual quality assessment checklists, in contrast to a universal tool (Pluye et al, 2009), were deemed more appropriate to facilitate specific study design assessments due to the heterogeneity of the included studies.
Data analysis
A narrative synthesis of the evidence was used because of the heterogeneity of the included studies. Following coding, thematic analysis was performed for each study and then tabulated across studies. Themes were discussed among all the researchers until agreement was reached. The results were triangulated without sep- arating the study designs (qualitative, quantitative or mixed-methods) to reduce duplication of themes and to improve validity and generalisability.
Figure 1: Flow chart (adapted from Moher et al, 2009) for screening and including studies.
Results
Available evidence
The searches identified 316 studies (310 studies from databases and 6 studies from other sources) (see Figure 1) and of 55 potentially relevant studies (all in English), a total of 22 were included (see Table 2). The inter-coder reliability of the screening processwas high (kappa score = 0.92).
Characteristics of the included studies
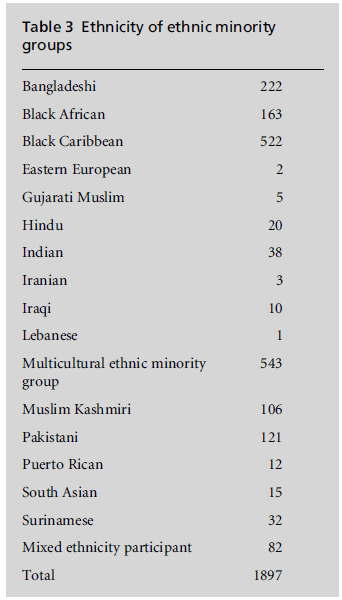
Of the 22 included studies (see Table 2), 18 used qualitative methods (one used mixed-qualitative methods (Greenhalgh et al, 1998), 13 used in-depth interviews (Kelleher and Islam, 1994; Duthie-Nurse, 1998; Rhodes and Nocon, 2003; Rhodes et al, 2003; Fagerli et al, 2005; Hjelm et al, 2005; Lawton et al, 2005, 2006a, 2006b, 2007, 2008), two used focus groups (Greenhalgh et al, 2011; Brown et al, 2006), and two used case study methods (Narayan and Rea, 1997; Fleming et al, 2008). Two studies used mixed methods (Greenhalgh et al, 2006; Lloyd et al, 2008) and three used quantitative methods (Naeem, 2003; Sedgwick et al, 2003; Povlsen et al, 2005). Studies were conducted in six different countries, namely theUK(n = 16), the USA (n = 2), Denmark (n = 1), Sweden (n = 1),Norway (n = 1) and theNetherlands (n = 1). Atotal of 1897 participants with varied ethnicities, of which 15 were stated and two were unspecified (see Table 3), were recruited from three settings (community, primary care and acute sectors). Nine studies included adults with type 2 diabetes (Greenhalgh et al, 2006, 2011; Fleming et al, 2008; Lawton et al, 2005, 2007; Lloyd et al, 2008; Kohinor et al, 2011; Duthie-Nurse, 1998; Kelleher and Islam, 1994), two studies involved women with gestational diabetes (Narayan and Rea, 1997; Hjelm et al, 2005), one study included children with type 1 diabetes (Povlsen et al, 2005), four studies included participants with both type 1 and type 2 diabetes (Fagerli et al, 2005; Stone et al, 2005; Rhodes and Nocon, 2003; Rhodes et al, 2003), and five studies did not specify the diabetes type (Brown et al, 2006; Greenhalgh et al, 1998; Naeem, 2003; Sedgwick et al, 2003; Gonzalez, 2008). The characteristics and cultural and linguistic needs of these populations were varied. Participants’ ages in all 22 studies ranged from 0 to 80 years. Although 21 of the studies included between 5 and 1100 ethnic minority participants each, one study (Narayan and Rea, 1997) included only one participant with gestational diabetes.
Quality assessment of the included studies and risk of bias
Of the 22 included studies (see online Tables S1S3), 14 studies were of good quality and met 80100% of the quality criteria (scored A) (Lloyd et al, 2008; Greenhalgh et al, 1998, 2006, 2011; Kohinor et al, 2011; Gonzalez, 2008; Lawton et al, 2005, 2007; Stone et al, 2005; Hjelm et al, 2005; Fagerli et al, 2005;Rhodes andNocon, 2003; Rhodes et al, 2003; Chowdhury et al, 2000). A further 8 studies were of moderate quality and met 5079% of the quality criteria (scored B) (Fleming et al, 2008; Brown et al, 2006; Duthie-Nurse, 1998; Narayan and Rea, 1997; Kelleher and Islam, 1994; Povlsen et al, 2005; Naeem, 2003; Sedgwick et al, 2003). No study scored below 50%. Ten studies included a range of different ethnic minority groups; the largest was black Caribbean (n = 522) in a UK study (Sedgwick et al, 2003), and the smallest number of minority participants involved in the studies were Lebanese (n = 1) in a Swedish study which included 27 participants from four ethnicities (Hjelm et al, 2005). Of all the included studies, 73% (n = 16) were published in the UK, and smaller numbers were published in the USA (n = 2), Denmark (n = 1), Sweden (n = 1), Norway (n = 1) and the Netherlands (n = 1).
Cultural barriers to diabetes care and management
Analysis revealed eight themes related to cultural barriers to diabetes care and management:
• cultural adherence in diet, exercise, and social interactions
• commitment to religious beliefs
Table 3: Ethnicity of ethnic minority groups.
• linguistic differences between patients and health workers
• low health literacy levels
• different beliefs about health and illness
• belief in expert and professional support
• low accessibility of culturally appropriate services/ information
• low concordance with western professional advice.
Cultural adherence with regard to diet, exercise and social interactions
A total of 13 studies reported strict adherence to cultural norms (Kelleher and Islam, 1994; Narayan and Rea, 1997; Greenhalgh et al, 1998, 2006, 2011; Chowdhury et al, 2000; Naeem, 2003; Hjelm et al, 2005; Lawton et al, 2005, 2006b, 2008; Stone et al, 2005; Fleming et al, 2008; Gonzalez, 2008; Kohinor et al, 2011). Participants in ten of these studies were of South Asian origin (Narayan and Rea, 1997; Kelleher and Islam, 1994; Lawton et al, 2005, 2006b, 2008; Stone et al, 2005; Chowdhury et al, 2000; Greenhalgh et al, 1998, 2006, 2011; Fleming et al, 2008; Naeem, 2003). They had strong traditions with regard to food, and their traditional dishes generally had a very high content of fat or deep-fried food despite awareness of the detrimental effects of these on health and wellbeing. Food classificationswere based on their perceptions of the strength of the food’s nourishing powers, rather than on western notions of nutritional content. Participants reported managing their diet by ‘cutting down on’ rather than replacing perceived unhealthy foodstuffs (Lawton et al, 2008). Food choices were determined by two interrelated and intersecting binary classifications, ‘strong’/‘weak’ and ‘digestible’/ ’indigestible’, which have social and symbolic meanings (Chowdhury et al, 2000). Some participants perceived western medicines as having detrimental effects if taken in excess or without eating traditional foodstuffs; this could lead to inappropriate self-adjustment of medication without medical consultation (Lawton et al, 2005). Surinamese participants also reported strong traditions related to food despite an awareness of the need to change their behaviour and adapt to healthy dietary guidelines (Kohinor et al, 2011).
Some participants of South Asian origin displayed more negative attitudes towards exercising, which they perceived as worsening their condition (Greenhalgh et al, 1998; Lawton et al, 2006b). Women reported more barriers to physical exercise, including fear of physical harassment, gender norms, social rules and cultural expectations that women should be indoors. It was stated that diabetes ‘weakened and aged’ the body, and this was reported as an additional barrier to undertaking physical exercise. Social interactions, and consumption of traditional dishes at social and cultural events such as weddings and religious festivals were regarded as very important (Chowdhury et al, 2000; Duthie-Nurse, 1998; Hjelm et al, 2005; Lawton et al, 2008). There was a strong attachment to social meanings and moral worth in real-life accounts of diabetes self-management (Greenhalgh et al, 2011).
Commitment to religious beliefs
Religious beliefs (Muslim, Christian, Hindu and Sikh) and practices were reported in 12 studies (Greenhalgh et al, 1998, 2011; Kelleher and Islam, 1994; Duthie- Nurse, 1998; Hjelm et al, 2005; Lawton et al, 2005, 2006a, 2007, 2008; Naeem, 2003; Kohinor et al, 2011; Stone et al, 2005; Gonzalez, 2008; Chowdhury et al, 2000). Eleven of these studies reported that participants, especially Muslims, demonstrated a strict commitment to religious beliefs about food and fasting during Ramadan, and diabetes self-management was a secondary consideration. All but one study (Lawton et al, 2007) identified religion and spirituality as major influences on coping with, managing and/or understanding diabetes. Religion was seen to be a source of support in coping with anxiety in one study (Stone et al, 2005).
Many studies found that most Muslim and some Hindus and Sikh participants reported an external health locus of control. For example, Muslim participants reported that having diabetes was the will of Allah, and thus beyond their control, and therefore they accepted their fate. They generally attributed their beliefs and other behaviours to Allah’s will, and held the view that adhering to dietary choices was the duty of an ill person. Although most of the participants were generally concerned about the impact of poor diabetes control, some Muslim participants held an attitude of ‘enjoying life and leaving the rest to Allah’, which resulted in poor diabetes control, especially during fasting periods (Naeem, 2003). In studies involving both ethnic minority and white European adults (Lawton et al, 2007; Hjelm et al, 2005; Stone et al, 2005), the ethnic minority participants, most of whom were Muslims, showed resignation at the diagnosis of diabetes, citing family history or a view that it wasAllah’s will,whereas theirwhite counterparts reacted with shock, denial, and concern about the perceived consequences of diabetes complications.
Linguistic differences between patients and health workers
In total, 14 studies attributed ineffective diabetes management to communication difficulties and lack of linguistically appropriate healthcare services (Greenhalgh et al, 1998, 2006, 2011; Duthie-Nurse, 1998; Rhodes and Nocon, 2003; Rhodes et al, 2003; Sedgwick et al, 2003; Fagerli et al, 2005; Hjelm et al, 2005; Stone et al, 2005; Lawton et al, 2005, 2006a, 2006b; Brown et al, 2006; Povlsen et al, 2005; Gonzalez, 2008). Five of these studies identified lack of knowledge about diabetes in ethnic minority groups arising from their inability to communicate in English (Greenhalgh et al, 1998, 2011; Hjelm et al, 2005; Lawton et al, 2005; Gonzalez, 2008). In three studies, participants preferred linguistically competent healthcare providers to interpreters because they wanted communication to be direct, and interpreters were perceived as a source of anxiety and frustration (Gonzalez, 2008; Brown et al, 2006; Lawton et al, 2006a). Two UK studies (Duthie-Nurse, 1998; Lawton et al, 2006b) reported that linguistic barriers between participants and the public limited participants’ knowledge of their neighbourhood and reinforced their vulnerability and social isolation, which led to some participants, especially women, staying indoors.
Seven studies identified a need for interpreter support (Greenhalgh et al, 1998, 2011; Rhodes and Nocon, 2003; Rhodes et al, 2003; Sedgwick et al, 2003; Fagerli et al, 2005; Povlsen et al, 2005), with four reporting a preference for professional interpreters rather than friends, relatives or receptionists (Rhodes and Nocon, 2003; Rhodes et al, 2003; Sedgwick et al, 2003; Fagerli et al, 2005). Reliance on family members or friends to interpret was inconvenient, as it disrupted people’s routines and responsibilities. These participants also reported being uncomfortable discussing some aspects of their illness in front of their relatives or friends, and preferred to ‘die in silence’ (Rhodes and Nocon, 2003; Fagerli et al, 2005). Some participants were unaware of the availability of local interpretation or advocacy services (Greenhalgh et al, 2011). Participants cited the use of medical jargon or technical terminology by health workers as a communication barrier (Fagerli et al, 2005; Stone et al, 2005; Lloyd et al, 2008).
Low health literacy levels
Eight studies reported low health literacy levels (low reading and numerical ability, resulting in reduced access to health information), which were perceived by the specific populations as hindering them from receiving effective diabetes care services (Narayan and Rea, 1997; Greenhalgh et al, 1998, 2011; Rhodes et al, 2003; Hjelm et al, 2005; Lawton et al, 2005, 2008; Povlsen et al, 2005; Gonzalez, 2008; Lloyd et al, 2008). Some participants’ lack of knowledge about diabetes was seen as a barrier to effective glycaemic control and/or diabetes self-management. For example, some participants only took their prescribed oral hypoglycaemic agents (OHAs) when their blood glucose levels were very high, over 18 mmol/l, or skipped meals in order to avoid taking them (Lawton et al, 2005).
In studies involving majority and minority populations, lower levels of educational attainment were reported within the minority groups, resulting in a lower level of understanding of diabetes care (Rhodes et al, 2003; Hjelm et al, 2005; Povlsen et al, 2005). The severity of the lack of literacy skills was noted in three studies (Greenhalgh et al, 1998; Rhodes et al, 2003; Lloyd et al, 2008). Audio-visual aids were used to improve comprehension, information retention, patient compliance and understanding if ethnic minority participants could not read or write in their first language. For some participants, lay and oral sources of health information were valued highly because of their low literacy skills (Greenhalgh et al, 1998, 2006; Lloyd et al, 2008). Lay diabetes information sources, such as family or personal experiences, appeared to have had a more profound influence on participants’ behaviours than scientific evidence.
Beliefs about health and illness
In total, 11 studies reported various beliefs about health and illness based on religious, individual and societal factors, as well as compromising healthcare service provision and/or concordance with professional advice or treatment (Greenhalgh et al, 1998, 2011; Kelleher and Islam, 1994; Duthie-Nurse, 1998; Hjelm et al, 2005; Lawton et al, 2005, 2006b, 2007; Brown et al, 2006; Naeem, 2003; Stone et al, 2005; Gonzalez, 2008). Muslim, Hindu and Sikh participants reported that these factors contributed to the way they perceived health and illness. Two sub-themes emerged in relation to perceived beliefs about health and illness, namely causation and the integration of curative and diabetes self-management measures into everyday life.
Causation
Nine studies discussed perceived beliefs relating to the cause of diabetes (Lawton et al, 2006b, 2007; Greenhalgh et al, 1998, 2011; Kelleher and Islam, 1994; Duthie- Nurse, 1998; Hjelm et al, 2005; Naeem, 2003; Stone et al, 2005). These included heredity, cold weather, unfamiliar western lifestyles, stress, Allah’s will and supernatural factors. It was believed that heredity meant that diabetes was unavoidable (Naeem, 2003; Stone et al, 2005). Attributing diabetes onset to ‘Allah’s will and beyond their control’ was common among Muslim participants in six studies (Lawton et al, 2006b, 2007; Kelleher and Islam, 1994; Hjelm et al, 2005; Naeem, 2003; Stone et al, 2005). Health, destiny, illness and death were perceived to be pre-ordained by Allah. Five studies discussed the power of Allah beyond the individual patient’s control, often leading to an attitude of resignation at diagnosis (Lawton et al, 2007; Hjelm et al, 2005; Greenhalgh et al, 2011;Naeem, 2003; Stone et al, 2005). In one study (Hjelm et al, 2005), involving ethnic minority and non-ethnic minority Swedish-born female participants, the nonethnic minority Swedish-born participants attributed the cause of gestational diabetes to scientific explanatory concepts, feared developing type 2 diabetes, and sought medical help and advice from healthcare professionals. Their beliefs about health and illness were explained in medical terms. Ethnic minority participants attributed the onset of diabetes to social and supernatural factors which made them reluctant to seek medical advice. In another study, South Asian participants attributed the onset of diabetes to UK lifestyles and/or values, or as a form of punishment for their past religious sins. Other life circumstances, such as poverty, limited access to healthcare services, and family-related stress, were also regarded as causes of diabetes. In contrast, white British participants considered their own lifestyle choices and personal failings,thus adopting an internal locus of control to a greater extent (Lawton et al, 2007). Five studies reported diet and/or lifestyle as factors that contributed to developing diabetes (Greenhalgh et al, 1998; Naeem, 2003; Hjelm et al, 2005; Brown et al, 2006; Lawton et al, 2006b), with one aligning ‘overweight figures’ with the cultural norms of projecting prosperity and well-being in the community rather than a health risk (Naeem, 2003). In two of these studies, participants partially associated physical exercise with diabetes, linking such exercise to worsening of their condition (Greenhalgh et al, 1998; Lawton et al, 2006b). South Asian participants linked cold weather rather than diet and/or inactivity to the onset of their diabetes, and believed that returning to South Asia would ‘cure’ them(Duthie-Nurse, 1998; Greenhalgh et al, 1998).
Integrating curative and diabetes selfmanagement measures into everyday life
This sub-theme examines the perceived healing paradigms and beliefs about diabetes self-management. In total, 11 studies reported at least one aspect of diabetes self-management, which demonstrated participants’ perceptions of diabetes and their daily coping mechanisms. In 10 studies, participants acknowledged that diabetes was a permanent condition and could be controlled, to an extent, through natural or supernatural and/or medicinal means. For example, in the study by Lawton et al (2005), participants reported that if western medicines were taken in excess, they could cause side effects, worsening their condition. In addition, they believed that traditional diets, such as chapatti and curry, had strengthening properties that counterbalanced these side effects of medication. In another study (Lawton et al, 2008), participants acknowledged the detrimental effects on their blood glucose control of some South Asian foodstuffs, such as ‘roti’, used by most participants to describe complete meals consisting of curries, chapatti and/or rice with side dishes, although its literalmeaning is ‘chapatti.’ However, most of them, especially among the first generation, did not effect dietary changes.
Participants also expressed initial qualms about taking oral hypoglycaemic agents, due to fear of acquiring the ‘sick person’s identity’ (Lawton et al, 2005). In one study, Gujarati Muslim men believed in the healing powers of ‘allopathic medicine’, western medicine and other complementary therapies, especially herbal therapies (Fleming et al, 2008). In another, the Puerto Rican participants preferred and perceived better effects of western medicines as opposed to complementary or alternative medicines (Gonzalez, 2008).
Belief in expert and professional support
In seven studies, some participants expressed reduced confidence in health workers, and questioned their competence and the support that they offered (Narayan and Rea, 1997; Greenhalgh et al, 1998; Lawton et al, 2005, 2006a; Rhodes and Nocon, 2003; Rhodes et al, 2003; Brown et al, 2006; Gonzalez, 2008). Participants in three of these studies had confidence in UK doctors and perceived them to be competent and trustworthy. In contrast, doctors from the Indian subcontinent were perceived as untrustworthy, lacking training, and as sometimes giving preferential treatment to the wealthy and to relatives and friends (Lawton et al, 2005, 2006a; Rhodes and Nocon, 2003; Rhodes et al, 2003). One of these studies reported that medicines available in the UK were superior but inherently dangerous compared with those available from the Indian subcontinent (Lawton et al, 2005). Another perceived the purpose of healthcare services to be the prompt detection and treatment of complications, rather than the provision of advice about managing their condition (Lawton et al, 2006a).
In one study (Narayan and Rea, 1997), family members of a Hindu patient with gestational diabetes felt humiliated and embarrassed following their exclusion from her care planning. They saw this as contrary to their customs of involving family members and valuing their contribution to care. In two studies involvingAfrican-Caribbeans, SouthAsians (Brown et al, 2006) and Puerto Ricans (Gonzalez, 2008), participants valued one-to-one linguistically and culturally concordant support from their health workers.
Low accessibility of culturally appropriate services and information
Nine studies reported variations in participants’ experiences, with negative issues relating to accessing culturally appropriate services or information (Narayan and Rea, 1997; Greenhalgh et al, 1998, 2011; Rhodes and Nocon, 2003; Rhodes et al, 2003; Stone et al, 2005; Brown et al, 2006; Lawton et al, 2006a, 2006b, 2008; Kohinor et al, 2011). These included gender issues, lack of culturally sensitive facilities during clinical consultations, and preferences for same-sex health workers irrespective of language barriers (Rhodes and Nocon, 2003). Some women avoided mixed-sex leisure facilities, such as swimming pools, and male gym instructors (Rhodes and Nocon, 2003; Lawton et al, 2006b), due to social and cultural beliefs about modesty (Greenhalgh et al, 2011). Six studies reported inappropriate and/or lack of culturally appropriate information about diet and foods (Greenhalgh et al, 1998; Narayan and Rea, 1997; Stone et al, 2005; Brown et al, 2006; Lawton et al, 2008; Kohinor et al, 2011). Participants in one study expressed a particular preference for gender-specific diabetes education sessions (Stone et al, 2005). Participants in two studies reported having received inappropriate information from healthcare workers that led to non-concordance with dietary and other healthcare advice (Greenhalgh et al, 1998; Rhodes et al, 2003). For instance, some Bangladeshi participants reported receiving leaflets in Bengali despite having very limited literacy skills (Rhodes et al, 2003). A further two studies reported the receiving of culturally insensitive advice (Narayan and Rea, 1997; Lawton et al, 2006a). For example, a Hindu patient was prescribed beef, perceived by Hindus as taboo, which contributed to the patient’s non-concordance with the care package recommended by the nurse (Narayan and Rea, 1997).
Low concordance with western professional advice
In total, 11 studies reported that participants did not follow professional advice due to lack of cultural knowledge, religious and language differences, or contextual factors, which were sometimes misinterpreted by health workers (Kelleher and Islam, 1994; Narayan and Rea, 1997; Duthie-Nurse, 1998; Chowdhury et al, 2000; Naeem, 2003; Hjelm et al, 2005; Lawton et al, 2005, 2008; Stone et al, 2005; Fleming et al, 2008; Greenhalgh et al, 2011; Kohinor et al, 2011). Participants expressed a desire for dietary balance, but reported the importance of the traditional norms and beliefs about their foods, which some claimed made them ‘weak and not strong enough’ (Kelleher and Islam, 1994; Duthie-Nurse, 1998; Chowdhury et al, 2000; Lawton et al, 2008; Fleming et al, 2008). All of these factors contributed to their non-adherence to professional recommendations. Two studies reported conflicting professional dietary advice and prescriptions that were contrary to participants’ traditions (Narayan and Rea, 1997; Kohinor et al, 2011). Two studies reported healthcare professionals’ lack of cultural awareness resulting in a mismatch between prescribed interventions and the patient’s beliefs and values (Narayan and Rea, 1997).
In one study, participants reported deliberately reducing their tablet intake without medical advice and concordance when they were lethargic or unwell, and despite awareness of the importance of prescribed oral hypoglycaemic agents (Lawton et al, 2005). In another study (Fleming et al, 2008), Gujarati Muslim men noted that contextual factors such as the choice of allopathic or cheaper homeopathic medicines influenced their choices. Stigma associated with having diabetes was reported as a factor contributing to low concordance with professional advice (Lawton et al, 2006b, 2007; Greenhalgh et al, 2011).
Discussion
The themes identified from this review of different ethnic, cultural and religious groups are participants’ strong adherence to culture, religious beliefs, linguistic differences between them and their health workers, low health literacy levels, different beliefs about health and illness, belief in expert and professional support, low accessibility of culturally appropriate services and information, and low concordance with western professional advice. Although we do not claim that our findings are universal, our review has collated and demonstrated significant cultural and linguistic barriers that are perceived by members of ethnic minority groups as compromising diabetes care. There appeared to be gaps in identifying and making reasonable adjustments to meet specific needs which could enhance the engagement of members of ethnic minority groups, increase their personal satisfaction with diabetes service provision, and ultimately improve their health-related outcomes. Only three studies (Lawton et al, 2006a; Sedgwick et al, 2003; Brown et al, 2006) reported specific attempts to seek their opinions of services or their cultural needs (Goody and Drago, 2009; Brown et al, 2002; Hill, 2006). More work is needed to improve cultural competence among health workers to enable them to more effectively empower patients to self-manage their diabetes. Health policies should therefore be directed towards improving cultural competence training to facilitate partnership working between patients and their healthcare providers. This has been shown to improve professional skills, cultural knowledge and attitudes among healthcare professionals, enabling them to work effectively in cross-cultural situations, thereby yielding positive health-related outcomes for their ethnic minority patients (Majumdar et al, 2004; Khanna et al, 2009).
For people with diabetes, knowledge of diabetes can significantly predict their perceptions of the quality of services they receive, as well as their own illness perceptions (Baradaran and Knill Jones, 2004). The inability of members of ethnic minority groups to speak English fluently and low levels of health literacy in their own mother tongue are seen, in the UK context, as factors contributing to increasing social distance and reducing communication, which often threaten trust between patients and their health workers (Audit Commission, 2000; Greenhalgh et al, 2011). Appropriate linguistically competent tools have been proposed to provide high-quality diabetes care services to ethnic minority groups (Roy and Lloyd, 2008).
As culture consists of shared but dynamic patterns of behaviours and interactions that remain ongoing among different ethnic groups (Naeem, 2003), caution should be exercised when interpreting these results, due to the heterogeneity of the studies with regard to factors such as place of publication, recruitment setting, study design, studied population, and the cultural barriers explored. In total, 73% (n = 16) of the included studies were published in the UK, which has a significant number of ethnic minority people with diabetes (Zeh et al, 2012), and merits substantial investment in researching the cultural differences faced by these populations (Brown et al, 2002, 2006). Therefore this review may be more applicable to the UK primary care situation.
Health workers need to acknowledge cultural similarities and differences and build trust that might encourage concordance (Goody and Drago, 2009). Dietary advice and information should not be prescriptive, but rather it should be negotiated, affordable, culturally sensitive, and take account of the importance of food in the individual patient’s ethnic and social context, as well as the importance of their religious, cultural, and health and illness beliefs (Brown, 1997; Hill, 2006). Diabetes health workers need to possess culturally competent knowledge of different cultures and ethnic foods, in order to empower patients with diabetes to adopt healthy lifestyles rather than to abandon familiar foods, as the evidence from the studies included in this review demonstrates limited cultural competence in these areas.
Strengths and limitations of the review
The search criteria included all ethnic minority groups with all types of diabetes and all primary qualitative and quantitative studies, excluding randomised controlled trials and quasi-experimental studies (which have been reported elsewhere), that have explored cultural differences globally. We assessed the quality of studies and included any research design to uncover any relevant studies that have explored cultural differences in diabetes. Triangulation of the results from the three included designs (quantitative, qualitative and mixed-methods) was a strength of the review, as they complemented each other, thereby improving the validity and generalisability of the findings. Our design was rigorous compared with previous systematic reviews that limited their search to specific ethnic minority groups, certain study types or specific types of diabetes, and which did not formally assess the methodological quality of the included studies (Brown et al, 2002; Fleming and Gillibrand, 2009).
The limitations of this review include the heterogeneity of the included studies, which causes difficulties in analysing the results or drawing firm conclusions. Some current research involving Eastern European populations within the UK may have been excluded, as only published studies were included. Excluding randomised controlled trials and quasi-experimental studies from this review may have resulted in the omission of some important information about ethnic minority groups, such as exploration of different aspects of cultural barriers and their effectiveness. However, our aim was to collate and highlight these barriers in order to target appropriate interventions for ethnic minority groups with diabetes. Zeh et al (2012) identified the key elements for such interventions. Further reviews, including both randomised controlled trials and observational studies, may provide more insight into this area. Some cultural barriers may be specific to certain ethnic minority groups. Grouping all ethnic minority groups together may be contentious, as they may differ in terms of health patterns and the effects of interventions, making it difficult to provide generic recommendations (Davidson et al, 2013). In fact the definitions of ethnic minority groups, culture and cultural barriers have been restricted in this review, as they have diverse interpretations. The fact that not all of the studies included participants’ health literacy levels may pose training and comprehension problems, and it is difficult to ascertain whether specific cultural barriers pertained to specific ethnic groups and/or age groups, which may have different educational needs. In addition, some vital information about ethnic minority groups may have been missed by excluding other chronic conditions, such as cancer.
Conclusions, implications for practice and recommendations for further research
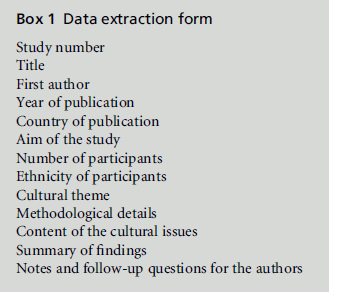
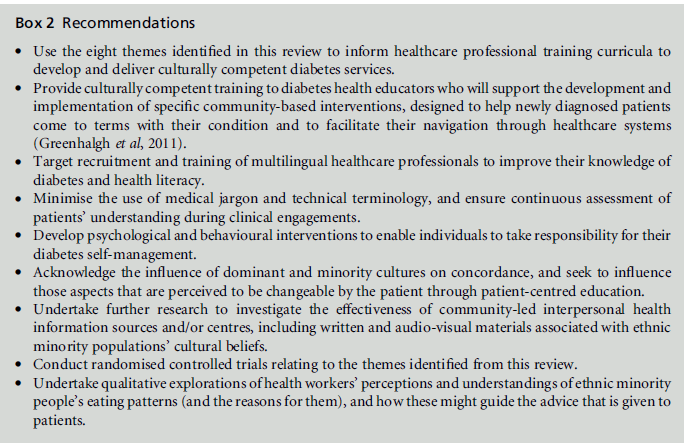
This review has examined cultural barriers that can affect the quality of life of ethnic minority groups with diabetes and their glycaemic control, including communication problems, religion, health literacy levels and beliefs about health and illness. Understanding these issues may enable health workers to deliver culturally appropriate and individualised care, and thus reduce health inequalities in diabetes service provision. The review has examined some of these cultural issues and offers suggestions to guide the planning and commissioning of culturally appropriate diabetes services for ethnic minority populations. Sustained and targeted actions by health commissioners and partnership with all stakeholders in diabetes management (local authorities, community organisations, diabetes leads in primary and secondary care, academic institutions and service users) are essential for improving diabetes-related outcomes (see Box 2).
ACKNOWLEDGEMENTS
We wish to thank all those who, either in person or online, helped us to undertake this review, especially Samantha Johnson and Jackie Cox, who reviewed the search strategy, Professor Trisha Greenhalgh and Professor Julia Lawton for providing additional clarifications and/or identifying further studies, and Professor Sudhesh Kumar, Professor Annie Young, Richard Dune and Peter Ewane, who provided practical guidance or directed us to possible sources of evidence. We are also grateful for the feedback received as a result of presenting this review at various meetings.
This review is part of a research fellowship funded by NHS West Midlands.
CONFLICTS OF INTEREST
None.
References
- Alam R, Speed S and Beaver K (2012) A scoping review on the experiences and preferences in accessing diabetesrelated healthcare information and services by British Bangladeshis. Health and Social Care in the Community 20:155–71.
- Audit Commission (2000) Testing Times: a review of diabetes services in England and Wales. London: Audit Commission.
- Baradaran H and Knill Jones R (2004) Assessing the knowledge, attitudes and understanding of type 2 diabetes amongst ethnic groups in Glasgow, Scotland. Practical Diabetes International 21:143–8.
- Brown K, Dyas J, Chahal P et al (2006) Discovering the research priorities of people with diabetes in a multicultural community: a focus group study. British Journal of General Practice 56:206–13.
- Brown SA, Garcia AA and Winchell M (2002) Reaching underserved populations and cultural competence in diabetes education. Current Diabetes Reports 2:166–76.
- Brown V (1997) Diabetic pregnancy: an inner-city perspective. Journal of Diabetes Nursing 1:45–50.
- Bulmer M (1996) The ethnic group question in the 1991 Census of population. In: Coleman D and Salt J (eds) Ethnicity in the 1991 Census. Volume One. Demographic characteristics of the ethnic minority populations. London: HMSO. pp. 33–62.
- Chowdhury AM, Helman C and Greenhalgh T (2000) Food beliefs and practices among British Bangladeshis with diabetes: implications for health education. Anthropology & Medicine 7:209–27.
- Cohen J (1960) A coefficient of agreement for nominal scales. Educational and Psychological Measurement 20: 37–46.
- Cone DC, Richardson LD, Todd KH et al (2003) Health care disparities in emergency medicine. Academic Emergency Medicine 10:1176–83.
- Creswell JW and Plano Clark VL (2007) Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage.
- Davidson EM, Liu JJ, Bhopal RS et al (2013) Consideration of ethnicity in guidelines and systematic reviews promoting lifestyle interventions: a thematic analysis. European Journal of Public Health doi: 10.1093/eurpub/ckt093
- Davies K (2006) Addressing the needs of an ethnic minority diabetic population. British Journal of Nursing 15:516–19.
- Department of Health (2001) National Service Framework for Diabetes: standards. London: The Stationery Office.
- Duthie-Nurse G (1998) An anthropological study into the views on diet and disease of a sample of Hindu Gujaratispeaking women with type 2 diabetes. Practical Diabetes International 15:109–12.
- Fagerli RA, Lien ME and Wandel M (2005) Experience of dietary advice among Pakistani-born persons with type 2 diabetes in Oslo. Appetite 45:295–304.
- Fleming E and Gillibrand W (2009) An exploration of culture, diabetes, and nursing in the South Asian community: a metasynthesis of qualitative studies. Journal of Transcultural Nursing 20:146–55.
- Fleming E, Carter B and Pettigrew J (2008) The influence of culture on diabetes self-management: perspectives of Gujarati Muslim men who reside in northwest England. Journal of Clinical Nursing 17:51–9.
- Gohdes D (1988) Diet therapy for minority patients with diabetes. Diabetes Care 11:189–91.
- Gonzalez L (2008) Health-care seeking behaviors of Puerto Ricans with diabetes mellitus who live in South Florida: an exploratory study. Doctoral dissertation. Orlando, FL: University of Central Florida.
- Goody C and Drago L (2009) Using cultural competence constructs to understand food practices and provide diabetes care and education. Diabetes Spectrum 22:43–7.
- Greenhalgh PM (1997) Diabetes in British South Asians: nature, nurture, and culture. Diabetic Medicine 14:10–18.
- Greenhalgh T (2008) Communicating with people who have limited English. Diabetes & Primary Care 10:89–93.
- Greenhalgh T, Helman C and ChowdhuryAM (1998) Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. British Medical Journal 316:978–83.
- Greenhalgh T, ChowdhuryMand Wood GW (2006) Storybased scales: development and validation of questionnaires to measure subjective health status and cultural adherence in British Bangladeshis with diabetes. Psychology, Health & Medicine 11:432–48.
- Greenhalgh T, Collard A, Campbell-Richards D et al (2011) Storylines of self-management: narratives of people with diabetes from a multiethnic inner city population. Journal of Health Services Research & Policy 16:37–43.
- Hawthorne K, Mello M and Tomlinson S (1993) Cultural and religious influences in diabetes care in Great Britain. Diabetic Medicine 10:8–12.
- Hill J (2006) Management of diabetes in South Asian communities in the UK. Nursing Standard 20:57–64; quiz 66.
- Hjelm K, Bard K, Nyberg P et al (2005) Swedish and Middle- Eastern-born women’s beliefs about gestational diabetes. Midwifery 21:44–60.
- International Diabetes Federation (2009) International Diabetes Federation Diabetes Atlas. Brussels: International Diabetes Federation.
- Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials 17:1–12.
- Kelleher D and Islam S (1994) The problem of integration: Asian people and diabetes. Journal of the Royal Society of Medicine 87:414–17.
- Khanna SK, Cheyney M and Engle M (2009) Cultural competency in health care: evaluating the outcomes of acultural competency training among health care professionals. Journal of the National Medical Association 101:886–92.
- Kohinor JE, Stronks K, Nicolaou M et al (2011) Considerations affecting dietary behaviour of immigrants with type 2 diabetes: a qualitative study among Surinamese in the Netherlands. Ethnicity & Health 16:245–59.
- Landis JR and Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–74.
- Lawton J, Ahmad N, Hallowell N et al (2005) Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. British Medical Journal 330:1247.
- Lawton J, Ahmad N, Hanna L et al (2006a) Diabetes service provision: a qualitative study of the experiences and views of Pakistani and Indian patients with type 2 diabetes. Diabetic Medicine 23:1003–7.
- Lawton J, Ahmad N, Hanna L et al (2006b) ‘I can’t do any serious exercise’: barriers to physical activity amongst people of Pakistani and Indian origin with type 2 diabetes. Health Education Research 21:43–54.
- Lawton J, Ahmad N, Peel E et al (2007) Contextualising accounts of illness: notions of responsibility and blame in white and South Asian respondents’ accounts of diabetes causation. Sociology of Health & Illness 29:891–906.
- Lawton J, Ahmad N, Hanna L et al (2008) ‘We should change ourselves, but we can’t’: accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethnicity & Health 13:305–20.
- Lloyd CE, Sturt J, Johnson M et al (2008) Development of alternative methods of data collection in South Asians with type 2 diabetes. Diabetic Medicine 25:455–62.
- Mainous AG 3rd, Diaz VA, Saxena S et al (2007) Heterogeneity in management of diabetes mellitus among Latino ethnic subgroups in the United States. Journal of the American Board of Family Medicine 20:598–605.
- Majumdar B, Browne G, Roberts J et al (2004) Effects of cultural sensitivity training on health care provider attitudes and patient outcomes. Journal of Nursing Scholarship 36:161–6.
- Modood T and Berthoud R (1997) Ethnic Minorities in Britain: diversity and disadvantage – Fourth National Survey of Ethnic Minorities. London: Policy Studies Institute.
- Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6:e100097.
- Naeem AG (2003) The role of culture and religion in the management of diabetes: a study of Kashmiri men in Leeds. Journal of the Royal Society for the Promotion of Health 123:110–16.
- Narayan MC and Rea K (1997) Nursing across cultures: the South Asian client. Home Healthcare Nurse 15:460–70.
- NHS Health Scotland (2004) Diabetes in Minority Ethnic Groups in Scotland: a report by the National Resource Centre for Ethnic Minority Health in collaboration with the Scottish Diabetes Group. Glasgow: NHS Health Scotland.
- Oldroyd J, Banerjee M, Heald A et al (2005) Diabetes and ethnic minorities. Postgraduate Medical Journal 81:486–90.
- Pluye P, Gagnon M, Griffiths F et al (2009) A scoring system for appraising mixed methods research, and concomitantlyappraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. International Journal of Nursing Studies 46:529–46.
- Popay J, Rogers A and Williams G (1998) Rationale and standards for the systematic review of qualitative literature in health services research. Qualitative Health Research 8:341–51.
- Povlsen L, Olsen B and Ladelund S (2005) Diabetes in children and adolescents from ethnic minorities: barriers to education, treatment and good metabolic control. Journal of Advanced Nursing 50:576–82.
- Rhodes P and Nocon A (2003) A problem of communication? Diabetes care among Bangladeshi people in Bradford. Health & Social Care in the Community 11:45–55.
- Rhodes P, Nocon A and Wright J (2003) Access to diabetes services: the experiences of Bangladeshi people in Bradford, UK. Ethnicity & Health 8:171–88.
- Roberts S (2007) The Way Ahead: the local challenge. London: Department of Health. Roy T and Lloyd CE (2008) Development of audio methods of data collection in Bangladesh. Diversity in Health and Social Care 5:187–99.
- Salimbene S (1999) Cultural competence: a priority for performance improvement action. Journal of Nursing Care Quality 13:23–35.
- Sedgwick JE, Pearce AJ and GullifordMC(2003) Evaluation of equity in diabetes health care in relation to African and Caribbean ethnicity. Ethnicity & Health 8:121–33.
- Stone M, Pound E, PancholiA et al (2005) Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester, UK. Family Practice 22:647–52.
- Wilson C, Alam R, Latif S et al (2012) Patient access to healthcare services and optimisation of self-management for ethnic minority populations living with diabetes: a systematic review. Health and Social Care in the Community 20:1–19.
- Zeh P (2010) Delivering diabetes care to ethnic groups: a pilot general practice survey. Diabetes and Primary Care 12:280–90.
- Zeh P, Sandhu HK, Cannaby AM et al (2012) The impact of culturally competent diabetes care interventions for improving diabetes-related outcomes in ethnic minority groups: a systematic review. Diabetic Medicine 29:1237–52.