Key words
cultural competence, in-vitro fertilisation, Israel, public health policy, reproductive health
Introduction
The concept of ‘cultural competence’ in healthcare emerged as a field of scholarly work and implemental practice mainly in the USA and the UK (Lavizzo- Mourey and MacKenzie, 1996; Brach and Fraser, 2000; Betancourt et al, 2003, 2005; Rees and Ruiz, 2003; McGee and Johnson, 2004; Wilson, 2004; Gregg and Saha, 2006; Koehn and Swick, 2006; Rapp, 2006; Teal and Street, 2009; Stanley et al, 2009). As a field of investigation and intervention, cultural competence reflects two complementary processes, namely concern about existing ethnic/racial disparities in health (Dressler, 1993; Nazroo, 2001; Cooper, 2002; Davy- Smith et al, 2002; Karlsen and Nazroo, 2002; Daniels and Schulz, 2006), and recognition of the acute need to eliminate these disparities by means of education and regulation (Brach and Fraser, 2000; Betancourt et al, 2003; Koehn and Swick, 2006). The impact of the movement in the USA has been so impressive that recent years have witnessed an ‘astonishingly rapid development of Cultural Competence as a major curriculum element in medical education’ (Koehn and Swick, 2006, p. 548).
Different definitions of cultural competence emphasise different aspects of the ways in which culture is present in healthcare or should be integrated into healthcare initiatives (Brach and Fraser, 2000; Rees and Ruiz, 2003; Gregg and Saha, 2006). It has been noted, for example, that a culturally competent healthcare system (or intervention or clinician) involves cultural sensitivity, cultural responsiveness and cultural humility (Rees and Ruiz, 2003), all of which embody recognition of and reaction to existing ethnosocial- economic power structures within and around health and illness (Nazroo, 2001). As has been convincingly argued by Betancourt et al (2003, p. 294), a broad grasp of the field includes reference to three levels of healthcare systems (organisational, structural and clinical) within which it is crucial to acknowledge and incorporate the ‘importance of culture, assessment of cross-cultural relations, vigilance toward the dynamics that result from cultural differences, expansion of cultural knowledge, and adaptation of services to meet culturally unique needs’ (Betancourt et al, 2003, p. 294, my italics for emphasis).
Incorporating cultural competency into healthcare systems, organisations and clinical encounters is one strategic outcome of a critically applied science aimed at enhancing patients’ power within a given context (see Box 1). Indeed, the prime motivation of the cultural competence movement has been ‘the desire to alleviate barriers to effective health care for immigrants, refugees, and others on the sociocultural margin’ (Gregg and Saha, 2006, p. 542). Here the focus is on structural and experienced ethnic and racial disparitieswhich are built into, represented in and re-shaped by health disparities. Although some aspects of causality and effect are still debated, studies of the relationships between race, ethnicity and health provide strong evidence for the inequalities involved in, among others, restricted accessibility of medical knowledge and services (Dressler, 1993; Mayberry et al, 2000), intersection between socio-economic and ethnic positions (Cooper, 2002; Nazroo, 2001, 2003), and institutional racism, violence and discrimination (Westwood, 1994; Karlsen and Nazroo, 2002; Smedley et al, 2003).
Across all of these, it is widely agreed that culture plays a crucial role in shaping such disparities (Lavizzo- Mourey and MacKenzie, 1996; Brach and Fraser, 2000; Betancourt et al, 2003; Rees and Ruiz, 2003; McGee and Johnson, 2004; Wilson, 2004; see Box 2). Examples vary from linguistic barriers to cultural inhibitions and cultural difference, which in its mild form may lead to misunderstandings, and in more tragic circumstances to ‘disastrous healthcare consequences’ (Gregg and Saha, 2006, p. 542).
Thus the cultural competence movement advocates a sensitive, responsive, humble approach on the part of caregivers and administrators, assuming that such an approach will eliminate the existing gaps between differently located socio-cultural groups within a given healthcare system. The practical application of this approach means ‘the ability of systems to provide care to patients with diverse values, beliefs and behaviors, including tailoring delivery to meet patients’ social, cultural, and linguistic needs’ (Betancourt et al, 2002, cited in Rees and Ruiz, 2003, p. 6). It therefore echoes the politics of difference and recognition, within which due recognition is viewed ‘not only as a courtesy we owe people [but also as] a vital human need’ (Taylor, 1997, p. 99). It is the actual move from a conceptual acknowledgment of difference to a communicative responsiveness (to different needs) that is at the implemental heart of cultural competence.
Cultural versus ethical competency: potential clashes
Although the concept of cultural competency has been influential in shaping health policy sensitivities, and has had a much welcomed effect on health educators and care administrators, some attention has also been paid to the weaknesses of the concept, particularly when applied as a pedagogic enterprise. It has been noted, for instance, that the practice of cultural competency may, paradoxically, rely on ‘stereotypic oversimplifications and/or insufficient information’ (Koehn and Swick, 2006, p. 552), and that cultural competence programmes ‘run the risk of reinforcing cultural stereotypes and biases, and of seeing stable cultural norms or predictable culturally based behaviors where none exist’ (Gregg and Saha, 2006, p. 543). This problematisation of the concept of cultural competence is based within a more critical view of the notion of culture and of the ways in which it is imagined by health advocates (Ming-Cheng and Clare, 2008).
However, while these critical reactions point to some conceptual and applicable limits of cultural competency, they do not challenge cultural competency as an ethical project. Rather, they focus on the ways in which the ethics of empathy, which requires acknowledgment, sensitivity and responsiveness, can be better served by revisions and amendments to existing applications. For example, Koehn and Swick (2006, p. 534) suggest that ‘cultural competence’ curricula for medical students should include elements that have so far been lacking in students’ education, such as recognition of ‘variations in socioeconomic backgrounds, power relations, health care skills, health beliefs and behaviors, and transition experiences’ as well as contents relating to empathy with and responding to ‘ethnoculturally discordant patients’ expectations [and] vulnerability’ (Koehn and Swick, 2006, p. 534).
In otherwords, under critique here are implemental issues relating to the translation of recognition and acknowledgment into caregivers’ practices of attentiveness, sensitivity, empathy and responsiveness. As will be explored in the following sections and discussed at length in the concluding section, a nonreflexive commitment to act on behalf of ‘the other’ not only runs the risk of pre-assuming the homogeny of ‘cultural disposition’, but also gives shape to a series of ethical tensions.
Taking this as a point of departure, I shall now direct attention to some of the weaknesses inherent in cultural competency as an ethical project. I use the term ‘ethical’ to denote the praxis of moral values and principles. For example, the moral obligation to recognise differences may be translated into pedagogic, regulative or organisational practices of cultural competence. The preceding discussion points to disruptions in the seemingly continuous flow from ‘the morals of recognition’ to ‘the ethics of cultural competency’, and points to existing tensions and incongruities between recognition and responsiveness. My main argument is that some of the explicit commitments of a culturally competent healthcare system, namely avoidance of judgmental attitudes, and adopting an attitude of cultural responsiveness, run the risk of ethical incompetence in that they may encourage the amplification of existing ‘cultural needs’, particularly within a system that is tuned to providing a service for consumers. In this context, the use of the term ‘consumers’ indicates the relevance of an economic system operated under the logic of supply/demand for health services within the project of cultural competency. Potential clashes between cultural and ethical competency are particularly evident in situations where responsiveness to what are perceived as ‘culturally based’ consumer demands can have a negative impact on the physical and/or emotional well-being of individuals or groups.
Certainly, the ethical weaknesses of cultural competency do not lie in the recognition of cultural needs, or in the commitment to respond empathically to such needs, but rather in a kind of mechanistic, nonreflexive responsiveness to what are perceived to be essential cultural needs. To illustrate this argument, I draw on findings from an ongoing sociological study of the new reproductive technologies (NRT) in Israel (Shalev and Gooldin, 2006; Gooldin, 2008; Gooldin, 2010). The study explores the interaction between four spheres of NRT in Israel, namely regulation, consumption, media and therapy. The data used in this study include a wide and versatile textual corpus, as well as interviews with fertility experts. The texts used included transcripts of parliamentary sessions and parliamentary committees that documented the process of regulating IVF in the past 20 years in Israel, media coverage of NRT issues in the major news papers over the past 20 years, court cases and court acts in which various aspects of IVF were debated from the 1990s to the mid-2000s, legislative documents on utilisation and financing issues with regard to IVF, the Internet forums and chatrooms of IVF consumers in Israel, and Ministry of Health documentation of consumers’ petitions and applications. These texts were systematically analysed by means of an incorporated methodology of discourse analysis and content analysis (Manning and Cullum-Swan, 1994). Statistical data were also gathered from secondary sources such as the Israeli Ministry of Health and the Bureau of Statistics. In addition, data are being gathered in an ongoing study based on in-depth interviews with fertility experts in IVF units. The study examines experts’ perceptions of existing utilisation patterns and public funding of IVF. In the discussion below I briefly refer to some pilot interviews conducted with experts working in public hospitals and private clinics in Israel.
Although it is well documented that the rates of utilisation of IVF in Israel are high, very few attempts have been made to decode the interactive social dynamics within which this practice is shaped. The findings of my study demonstrate that the existing patterns of IVF usage have the overwhelming support of fertility experts, health regulators and the general public. Of particular interest to the current discussion are findings indicating that Israeli health legislators and fertility experts account for and legitimise the excessive usage of IVF in Israel, among others, by perceiving it to be the appropriate response of a public healthcare system to the culturally unique needs of Israeli IVF consumers. This will be described in detail below, but for now suffice it to say that the practical consequence of this attitude is an overwhelming rate of utilisation of NRT, which reproduces and amplifies existing ‘cultural needs’, and which can potentially have a negative effect on the physical and emotional wellbeing of ‘infertile’ individuals, particularly women.
Cultural versus ethical competency: the case of IVF in Israel
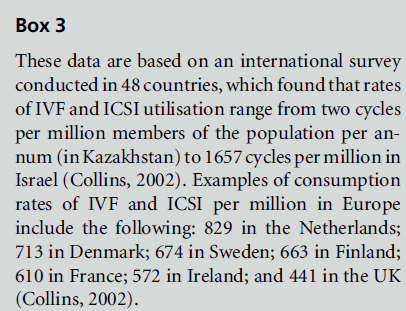
International comparison shows that assisted reproductive technologies (ART) are utilised in Israel in unique ways, both in terms of the extent of their usage (Shalev and Gooldin, 2006) and in terms of the meanings that they carry in the public (Portugese, 1998; Birenbaum-Carmeli, 2004; Gooldin, 2008; Sperling, 2010) and private (Khan, 1998; Remennick, 2000; Benjamin and Ha’elyon, 2002; Teman, 2003) spheres. Israel has the highest rates of ART intervention in the world, the highest per capita consumption rate of infertility therapy, and an internationally unprecedented public health policy, which poses very few restrictions on the eligibility of Israeli citizens for infertility treatments within the National Health Insurance (NHI) system (Shalev and Gooldin, 2006). For example, there are 3.52 IVF units per million members of the population in Israel, compared with 2.39 in France, 1.63 in Ireland, 1.31 in the USA, 1.28 in the UK, and 1.22 in Germany (Collins, 2002). Israeli women consume more IVF treatments than their counterparts anywhere else in the world, 1657 treatment cycles per million members of the population per annum (tcpm), which is six times the international average of 289 tcpm (Collins, 2002; see Boxes 3 and 4).

Israel’s consumption rates are consistent with a uniquely inclusive public health policy, which poses very few restrictions on the eligibility of Israeli citizens for publicly funded infertility treatments within the NHI system. To date, the basic ‘health basket’ in Israel, as specified in an addendum to the Law, includes infertility diagnosis and therapy, and IVF for the purpose of ‘Bearing a first and second child – for couples who do not have children from their current marriage, and also for a childless woman who wishes to establish a single-parent family’ (Paragraph 6(e) of the Second Addendum to the National Health Insurance Law, 1994, S.H. no. 1469, p. 183).
This applies to all Israeli citizens, with an upper age limit for women undergoing treatments of 54 years when eggs are donated, and 45 years when egg donation is not involved. This level of public funding, in which the overall number of IVF treatments per patient is not limited to the birth of two children, and entitlement to treatments is not affected by the patient’s marital status, sexual orientation, or whether they have children from previous relationships, is a unique Israeli phenomenon. Other countries in which fertility treatments are funded within the NHI system restrict the number of treatment cycles (usually to three to five), apply a lower age limit for women undergoing treatments (usually 40 years at most), and in some countries single or gay women are denied publicly funded treatments, as are couples who already have children from previous relationships (Plomer et al, 1999).
The magnitude of IVF usage in Israel raises a number of financial concerns because of health-related costs, as well as ethical questions regarding priority setting within a system of limited economic resources (Shalev and Gooldin, 2006). First, IVF is an invasive procedure and involves various medical risks, including ovarian hyperstimulation syndrome, which can be life-threatening. Although the connection between IVF and the risk of breast cancer has not been determined, some studies indicate that the long-termuse of certain infertility drugs could adversely affect the risk of breast cancer (Burkman et al, 2003), and that there is an increased risk of breast cancer in women who undergo more than four treatments (Pappo et al, 2008). A summary of other risks and costs involved in IVF has been provided by Shalev and Gooldin (2006). In addition, there are risks involved in multiple gestations, with a ‘20-fold increased risk of multiple pregnancy following ART compared with the general population’ (Fathalla, 2002, p. 4). Infants from multiple gestations are much more likely than singletons to be born prematurely with very low birth weights, with the attendant costs of neonatal intensive care. Such infants also carry an increased risk of perinatal death and permanent disability, and thus they challenge ‘the responsible practice of medicine’ (Lambert, 2002, p. 3011).
Secondly, IVF is an economically costly procedure, which, in the context of a limited publicly funded health service, raises issues of prioritising and rationing different services. From a medical sociological perspective, any practice of prioritisation services is always part of the politics of values, morality and socially constructed preferences. Since infertility is neither a disease nor a life-threatening condition, prioritising infertility treatments within a limited public system inevitably involves complex ethical dilemmas (Shalev and Gooldin, 2006).However, these dilemmas as well as concerns about health risks are almost invisible in the Israeli public discourse. Some academic publications have pointed to the problematic implications of the use of IVF in Israel (Landau, 1996; Birenbaum-Carmeli, 1998; Birenbaum-Carmeli et al, 2000; Remennick, 2000; Birenbaum-Carmeli, 2004; Shalev and Gooldin, 2006; Gooldin, 2008), and there has been some media interest in critical viewpoints. For example ‘Haaretz’, a widely read daily newspaper, published several articles, reports and opinion columns that voiced explicit criticism of ‘the Israeli obsession’ with fertility treatments (Gooldin, 2008). Nevertheless, the overall public mindset in Israel is overwhelmingly supportive of IVF utilisation, and lacks critical perspectives. In fact, during the past two decades the intense usage of IVF has been persistently and enthusiastically promoted by key actors in the public sphere, including legislators, policy makers, media agents, fertility experts and IVF consumers (Gooldin, 2008). Not surprisingly, the criteria for entitlement to publicly funded treatments have been continuously extended, and the number of IVF treatments per capita has been increasing (Shalev and Gooldin, 2006).
From a medical sociological perspective, this unique phenomenon calls for an explanation of the social and cultural forces at work in the production of reproductive technologies in Israel. Existing policy and utilisation patterns of IVF are entangled in Israel within four intersecting discourses of the (in)fertile body:
1 a traditional pro-natal discourse which compels biological parenthood and which is reflected in the high total fertility rate in Israel, which was 2.8 TFR in 2007, compared with an average of 1.7 TFR in other developed countries (Population Reference Bureau, 2007 World Population Data Sheet, www. prb.org/pdf07/07WPDS_Eng.pdf)
2 a pro-family discourse that shapes a normative compulsion for birthing ‘at least’ two children
3 a national discourse propelled by a sense of demographic risk which is related to the Jewish–Arab conflict, and to the collective memory of the annihilation of 6 million Jews in the Holocaust
4 a liberal discourse that assumes ‘emotional rights’, or more specifically the right for happiness via the experience of parenthood.
These discourses operate as ‘regimes of justifications’ (Boltanski and The´venot, 1999), that is, as contextual frameworks within and through which moral claims regarding the usage of IVF are being made and negotiated in the Israeli public sphere.
One example of this discursive dynamic was a public debate that took place in 2003 following the Ministry of Finance’s proposal to cut the public funding allocated to IVF treatments. According to the Ministry’s proposal, the basic ‘health basket’ would ‘only’ cover a maximum of five treatment cycles up to the birth of one child, rather than two. This proposal sparked a heated public debate in which consumers, policy makers, politicians and fertility experts called into question the moral validity of the Ministry’s attempt. As I have argued elsewhere (Gooldin, 2008), within this debate the rational imperative for a ‘cost– effect’ calculability was disputed, and alternative moral justifications were outlined. For instance, some argued that the Ministry’s proposal prevented Israeli fertility consumers, Jews and Arabs alike, from exercising a civil and human ‘right to parenthood’ which, they claimed, was crucial in Israel. It was also argued that, specifically in Israel, a family with one child was not a ‘real’ family, and that the right to form a family was being denied. Within this debate of IVF budgeting, some politicians argued that the demographic importance of child-bearing in Israel should be prioritised over any economic considerations. In addition, it was argued by politicians and IVF consumers that the Ministry’s proposal was profoundly immoral in that it might terminate continuity in the lineage of some Holocaust survivors’ families, whose grandchildren would be denied IVF therapy under the new regulations. As can be seen from these examples, throughout these different arguments the local and unique characteristics of Israeli IVF consumers were repeatedly emphasised.
Moreover, and of particular relevance to this paper, Israeli fertility experts who took an active part in this public dispute were explicitly reflexive about the unique cultural needs of their local IVF consumers. Both in statements provided for parliamentary committees and in interviews given to the media, fertility experts expressed the view that IVF consumers in Israel operate in a unique social and cultural environment and that this uniqueness compels responsiveness on behalf of the public health system. For example, one of the most prominent fertility experts in Israel testified for a special parliamentary committee, stating that, compared with families in other parts of the world, Israeli families, both Jewish and Arab, are unique because ‘In Israel, children are the essence of the family. ... Which of us [Israelis] would say that s/he would give up having a child? No one. Perhaps a fraction of the population, and they are out of their minds [‘mufra’im]’ (Professor Mashiach, Committee on the Status of Women, Protocol 44, The Israeli Knesset, Jerusalem, 18 September 2003). Consequently, he concluded, and specifically in Israel, IVF treatments are ‘the apple of one’s eye’ [tzipor hanefesh]. In the same spirit he testified for another parliamentary committee, arguing that ‘It would be a great injustice to deny couples the right for a second child. There is no family in Israel, neither Jewish nor Arab, that would be satisfied with one child’ (Professor Mashiach, protocol of the Finance Committee, The Israeli Knesset, Jerusalem, 4 December 2003).
Similarly, an Israeli–Palestinian MK, Ahmad Tibi, who is also a trained gynaecologist, argued that in Israel ‘infertility, like cancer, contains malignant aspects’ because ‘it spreads mentally, socially, and in the family. ... The whole family suffers. It [becomes] the ultimate everyday issue; [childless couples] only think about how to bear children, as a basic right, because every woman and man want to be a parent. ... They want to escape the mental and social distress. In many occasions families fall apart because of this’ (Ahmad Tibi, Committee on the Status of Women, Protocol 48, The Israeli Knesset, Jerusalem, 18 September 2003). This notion that Israeli consumers of IVF are unique, and moreover that the public health system and medical practice should acknowledge and respond to this uniqueness, was voiced by experts not only in parliamentary committees but also in interviews with the media. One example is an interview with Professor Neri Laufer, the head of a large gynaecological unit in a central hospital, which was published in one of the most widely read internet news sites in Israel (Yediot Achronot). In this interview Professor Laufer was quoted as saying that by cutting the public funding for IVF, the Ministry was ‘Trying to imitate what is accustomed in France and in some of the Scandinavian countries, where the State limits IVF funding up to three treatment cycles. But we do not resemble Europe in anything. ... The Israeli State is the only place in the world where ... the amount of treatment cycles has not been limited. This Ministry’s proposal chops off an extremely important stem of humane [medical] treatments, in a State where bereavement is constantly experienced’ (Professor Neri Laufer, quoted in YNET, 16 September 2003). In this statement it is again the unique characteristics of the Israeli society that shape IVF therapy as a humane solution to a problem that carries local meanings. The application of a unique public health policy is thus presented as an empathic response to the essentially unique needs of consumers. A similar discourse of ’unique needs’ of Israeli reproductive health consumers has been documented in a study of genetic counselors in Israel (Hashiloni-Dolev, 2007). In this study Hashiloni-Dolev shows that Israeli genetic concealers support the practice of abortion much more than their colleagues in Germany, based on the view that the Israeli society poses uniquely difficult challenges to children born with somemedical conditions, as well as to their parents. In the course of this argument, uniqueness and essential needs are objectified and become facts with which the health system has to cope. With regard to IVF, this objectification was summarised in a sub-headline in a leading Internet newspaper: ‘Senior gynaecologist: these are vital humane treatments’ (quoted in YNET, 16 September 2003).
The same logic was evident in a pilot study of fertility experts’ views of IVF utilisation in Israel. Most of the gynaecologists who were interviewed for this study showed that they were well aware of the pronatal environment in which their patients lived, and of the social expectations and pressures to which they were subjected. For example, a senior gynaecologist who had been working for 15 years in a large IVF unit in the centre of Israel explained that most of his patients wanted to start having IVF treatments ‘yesterday’, regardless of their medical condition. ‘They arrive at the clinic very stressed, and expect immediate results, and it is me who has to ‘‘put the brakes down.’’ [Q: How do you explain this? Why is that so?] The pressure they are under is enormous. Anyone who lives here understands this. ... I don’t have to tell you, [that] we are an extremely familial society, and children are extremely important. It’s the most natural thing for us [Israelis]. [It is] almost impossible not to feel this way.’ [Q: So what is your reaction to these expectations of your patients, to the fact that theywant IVF treatment ‘yesterday’?]. I do the best I can to give them the best treatment possible. This is my role as a doctor, nothing else. ... But I also understand their pressure, and many times it is very difficult for us [doctors] to face the pressure that patients are putting on us. There is a great difficulty in unsuccessful attempts to have children. This is of course the same for anyone, anywhere. But maybe here [in Israel] it’s even harder. It’s a social issue and a religious issue ... and we [doctors] have to take it into consideration.’
It seems, then, that fertility experts in Israel view themselves as culturally responsive to the need of Israeli consumers for biological parenthood in a pronatal context. These experts both account for and legitimise the excessive usage of IVF as the appropriate response to the culturally unique need of Israeli consumers. This attitude, in turn, shapes legislative and clinical practices and results in a continuous and overwhelming rate of utilisation of ART. Consequently, ‘pro-natal culture’ and ‘pro-natal needs’ are reproduced and amplified via the practice of reproductive technologies.
This dynamic can have a negative impact on the physical and emotional well-being of infertile individuals, and more specifically of women who are subjected to an ever growing pressure to use IVF on the one hand, and are potentially exposed to medical risks on the other. It is in this sense that a well-intended culturally competent attitude, that acknowledges and responds to consumers’ cultural needs while avoiding judgemental attitudes, runs the risk of ethical incompetence. The ethical weaknesses of cultural competency do not lie in the recognition of cultural needs, or in the commitment to respond empathically to such needs, but rather in a mechanistic, non-reflexive responsiveness towards what are objectified as ‘essential’ cultural needs.
Towards an ethically competent cultural competence
In recent years, the discourse of cultural competency has been characterised by issues related to managing the normative, cultural and habitual aspects of social distance in healthcare (Karakayali, 2009). Translating this project into the field of reproductive health can mean for example, recognising diverse meanings of infertility or childlessness among individuals from different ethnic groups with a single health care system (Culley and Hudson 2006) or around the globe (van Belen and Inhorn 2002). One applicable example of this is the emphasis on communication skills within a culturally competent clinical encounter, where physicians are encouraged to, among other things, recognise and manage potential cultural differences between themselves and their patients (Teal and Street, 2009). In this example, while the ethics of cultural competency lie in conceptually recognising cultural differences and social distance, it is actually through the communicative act of acknowledging such differences that the ‘problem’ of distance is managed. This is but one demonstration of the ways in which the discourse of social distance shapes both the analytical basis of cultural competency and its practical implementations. It is precisely to these issues that culturally competent experts should attend, while avoiding the traps of stereotyping and ‘othering’ health consumers (Bottorff et al, 2004; Jhonson et al, 2004: Gregg and Saha, 2006; Koehn and Swick, 2006).
Against this backdrop, the attitudes exhibited by Israeli physicians and administrators with regard to IVF utilisation make a fascinating example of a very different scenario. In the Israeli context, the notion of infertile couples’ cultural needs reflects and reproduces essentialist/stereotypical perceptions of ‘Israeli culture’, that is, the deep and total desire for biological parenthood. It seems that this construction emerges, paradoxically, from a sense of social closeness and cultural identification between health providers and consumers. This dynamic stands in opposition to the issues of social distance, which underlined the discourse of cultural competency. I want to suggest that this discursive mechanism carries some challenging ethical dilemmas for a culturally competent health policy for two reasons. First, it is based on the assumption that ‘the Israeli culture’ is a homogeneous entity. Secondly, it consequently assumes that consumers’ motivations and needs are also homogeneous. This leads to a dismissal of possible cracks in the totality of the pro-natal Israeli culture. One recent account of such cracks is documented in a study of a child-free community in Israel (Donat, 2010) that resists natalismin a similar vein to that documented in other post-industrial countries. Other examples that are directly related to reproductive health include the emerging, even if currently scarce, voices opposing the compulsive consumption of IVF in Israel. This tendency is shown, for example, in a critical presentation of IVF usage in a leading daily newspaper (Ha’aretz, 2005), in an article written by a woman journalist. In this article not only did the journalist identify herself as an Israeli woman who did not have children, but also she voiced, through quotations, acutely critical views of pro-natalism and IVF consumption. In addition, she quoted an anonymous female reader who had criticised an excessive IVF consumer (a woman), saying that ‘In my opinion, your efforts to gain the fruit of your womb are insane. ... Motherhood is a wonderful thing indeed, but there are other wonderful things in the world. Your willingness to devote all your life and physical and mental resources to giving birth to a child looks like an obsession’ (Ha’aretz, 2005).
Although these resistant voices are in a minority and do not represent the general identification with biological pro-natalism in Israel, to ignore their existence and the potential possibilities to which they point is to reproduce the perceived totality of pro-natalism in Israel. What is at stake here is the reproduction, by the agency of health experts and regulators, of the very same cultural matrix that is pre-assumed by them. Paradoxically, it seems that this mechanism is enforced via a non-reflexive tight identification with consumers’ needs, and possibly even by the sentiment of cultural closeness. It can thus be suggested that a more ethical cultural competence in this context will involve managing ‘cultural identification’ and ‘cultural sameness’ rather than ‘social distance’ and ‘cultural difference.’ As demonstrated by the Israeli example of reproductive healthcare, in some cases a more reflexive notion of cultural competency may involve taking on the anthropological directive for estrangement, that is, suspending the ‘taken for granted’ and ‘common- sensian’ understanding of our own culture and cultural knowledge (Keane, 2005).
This paper sought to offer an initial outline of some of the ethical limitations inherent in the project of cultural competency, by pointing to potential tensions between a culturally competent commitment to acknowledge and embrace consumers’ unique cultural needs, and an ethically competent commitment to best serve consumers’ physical and emotional wellbeing. The critique offered here does not undermine the enormous validity of cultural competency as a legislative, clinical or pedagogic project. However, based on the study of IVF in Israel, I want to propose that a careful consideration of cultural competency is needed, one that takes into account potential clashes between the ethics of empathy and the ethics of judgement, and incorporates them into a more reflexive framework. As we have seen above, potential clashes between cultural and ethical competence are particularly evident in situations where so-called passive responsiveness to culturally based consumers’ demands can have a negative impact on the well-being of individuals or groups. Such clashes can occur with regard to different cases, ranging from consumer demand for excessive usage of IVF to consumer demand for excessive plastic surgery (Brooks, 2004), female-selective abortions (Miller, 2001), the use of pre-implantation genetic diagnosis for the purpose of gender selection (Robertson, 2003), and so on.
To some extent, cultural competence can be seen as an agenda for ‘cultural relativism’, where differences are regarded ‘positively’ (McGee and Johnson, 2004, p. 76). In this respect, a culturally competent healthcare agent in the context of clinical interactions should become ‘culturally responsive by incorporating the individual’s beliefs, lifeways and practices into a mutually acceptable treatment plan’ (McGee and Johnson, 2004, p. 76). This agenda has been motivated by the desire to alleviate both barriers of ‘otherness’ and the health disparities that accompany them within a given system.
Empathy is obviously a vital element of cultural competence, but the ethics of empathy should not be sought separately from, or in opposition to, the ethics of judgement. Furthermore, in some cases, such as the utilisation of IVF in Israel, the latter has to be more vividly incorporated into a culturally competent healthcare system. Considering the limits of cultural competency and incorporating them into a more reflexive conceptual framework will help us to work towards a more ethically competent cultural competency.
CONFLICTS OF INTEREST
None.
References
- Baer HA (1997) The misconstruction of critical medical anthropology: a response to a cultural constructivist critique. Social Science and Medicine 44:1565–73.
- Baer HA, SingerMet al (2003) Medical Anthropology and the World System: a critical perspective. WestPoint, CT: Bergin & Garvey.
- Benjamin O and Ha’elyon H (2002) Rewriting fertilization: trust, pain, and exit points. Women’s Studies International Forum 25:667–78.
- Betancourt J, Green A et al (2003) Defining cultural competence: a practical framework for addressing racial/ ethnic disparities in health and health care. Public Health Reports 118:293–301.
- Betancourt J et al (2005) Cultural competence and health care disparities: key perspectives and trends. Health Affairs 24:499–505.
- Birenbaum-Carmeli D (1998) Reproductive partners: woman–doctor relations in Israeli and Canadian IVF contexts. In: Scheper-HughesNandSargentC(eds) Small Wars: the cultural politics of childhood. Berkeley, CA: University of California Press. pp. 75–92.
- Birenbaum-Carmeli D (2004) ‘Cheaper than a newcomer’: on the social production of IVF policy in Israel. Sociology of Health and Illness 26:897–924.
- Birenbaum-Carmeli D, Carmeli Y and Cohen R (2000) Our first ‘IVF baby’: Israel and Canada’s press coverage of procreative technology. International Journal of Sociology and Social Policy 7:1–38.
- Boltanski L and The´venot L (1999) The sociology of critical capacity. European Journal of Social Theory 2:359–77.
- Bottorff JL, Browne AJ, Grewal S et al (2004) Othering and being othered in the context of health care services. Health Communication 16:255–71.
- Brach C and Fraser I (2000) Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research and Review 57:181–217.
- Brooks A (2004) Under the knife and proud of it: an analysis of the normalization of cosmetic surgery. Critical Sociology 30:207–39.
- Burkman RT et al (2003) Infertility drugs and the risk of breast cancer: findings from the National Institute of Child Health and Human Development Women’s Contraceptive and Reproductive Experiences Study. Fertility and Sterility 79:844–51.
- Collins JA (2002) An international survey of health economics of IVF and ICSI. Human Reproduction 8:265–77.
- Cooper H (2002) Investigating socio-economic explanations for gender and ethnic inequalities in health. Social Science and Medicine 54:693–707.
- Culley L and HudsonN(2005) Diverse bodies and disrupted reproduction: infertility and minority ethnic communities in the UK. International Journal of Diversity in Organisations, Communities, and Nations 5:117–26.
- Daniels J and Schulz AJ (2006) Constructing whiteness in health disparities research. In: Mulling L and Schulz AJ (eds) Gender, Race, Class and Health: intersectional approaches. San Francisco, CA: Jossey-Bass. pp. 89–129.
- Davy-Smith G, Chaturvedi N, Harding S et al (2002) Ethnic inequalities in health: a review of UK epidemiological evidence. In: Nettleton S and Gustafsson U (eds) The Sociology of Health and Illness Reader. Cambridge: Polity Press. pp. 256–77.
- Donat O (2010) Cracked pro-natalism: narratives of reproduction and non-reproduction in Israel [in Hebrew]. Israeli Sociology 11:417–38.
- Dressler W (1993) Health in the African American community: accounting for health inequalities. Medical Anthropology Quarterly 7:325–45.
- Fathalla MF (2002) Current challenges in assisted reproduction. In Vayena E et al (eds) Current Practices and Controversies in Assisted Reproduction. Geneva: World Health Organization. pp. 3–12.
- Gooldin S (2008) Technologies of happiness: fertility management in a pro-natal context. In: Kemp A and Yona Y (eds) Citizenship Gaps: migration, fertility and identity [in Hebrew]. Jerusalem: Van Leer/HakibutzHameuchad. pp. 265–302.
- Gooldin S (2010) New reproductive technologies and emerging moral vocabularies: an agenda for studying technologiesin- action. Paper presented at the 35th Annual Meeting of the Society for Social Studies of Science, Tokyo, Japan, August 2010.
- Gregg J and Saha S (2006) Losing culture on the way to competence: the use and misuse of culture in medical education. Academic Medicine 81:542–7.
- Ha’aretz (2005) Bring six, bring seven, bring eight children. 25 January 2005. Hashiloni-Dolev Y (2007) A Life (Un)Worthy of Living: reproductive genetics in Israel and Germany. Dordrecht: Springer.
- Jhonson RL et al (2004) Patient/race ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health 94(12):2084–90.
- Khan SM (1998) Reproducing Jews: a cultural account of assisted conception in Israel. Durham, NC: Duke University Press.
- Karakayali N (2009) Social distance and affective orientations. Sociological Forum 24:538–62.
- Karlsen S and Nazroo JY (2002) Agency and structure: the impact of ethnic identity and racism on the health of ethnic minority people. Sociology of Health and Illness 24:1–20.
- KeaneW(2005) Estrangement, intimacy, and the objects of anthropology. In: SteinmetzG(ed.) The Politics of Method in the Human Sciences: positivism and its epistemological others. Durham, NC: Duke University Press. pp. 59–88.
- Koehn PH and Swick HM (2006) Medical education for a changing world: moving beyond cultural competence into transnational competence. Academic Medicine 81: 548–56.
- Lambert RD (2002) Safety issues in assisted reproduction. Human Reproduction 17:3011–15.
- Landau R (1996) Assisted reproduction in Israel and Sweden: parenthood at any price? International Journal of Sociology and Social Policy 16:29–46.
- Lavizzo-Mourey R and MacKenzie E (1996) Cultural competence: an essential hybrid for delivering high quality care in the 1990s and beyond. Transactions of the American Clinical and Climatological Association 107: 226–37.
- McGee P and Johnson MRD (2004) Cultural competence. Diversity in Health and Social Care 1:75–9.
- Manning P and Cullum-Swan B (1994) Narrative, content and semiotic analysis. In: Denzin N and Lincoln Y (eds) Handbook of Qualitative Research. London: Sage Publications.
- Miller BD (2001) Female-selective abortion in Asia: patterns, policies and debates. American Anthropologist 103: 1083–95.
- Ming-Cheng ML and Clare S (2008) Beyond cultural competency: Bourdieu, patients and clinical encounters. Sociology of Health and Illness 30:741–55.
- Nazroo JY (2001) Ethnicity, Class and Health. London: Policy Studies Institute.
- Nazroo JY (2003) The structuring of ethnic inequalities in health: economic position, racial discrimination and racism. American Journal of Public Health 93: 277–84.
- Pappo I, Lerner-Geva L et al (2008) The possible association between IVF and breast cancer incidence. Annals of Surgical Oncology 15:1048–55.
- Plomer A, Smith I and Martin-Clement N (1999) Rationing policies on access to in vitro fertilisation in the National Health Service. Reproductive Health Matters 7:60–70.
- Portugese J (1998) Fertility Policy in Israel: the politics of religion, gender and nation. Westport, CT: Praeger. Rapp DE (2006) Integrating cultural competency into the undergraduate medical curriculum. Medical Education 40:704–10.
- Rees C and Ruiz S (2003) Compendium of Cultural Competence Initiatives in Health Care. Henry J. Kaiser Family Foundation. www.kff.org/uninsured/6067-index.cfm
- Remennick L (2000) Childless in the land of imperative motherhood: stigma and coping among Israeli women. Sex Roles 47:821–41.
- Robertson JA (2003) Extending preimplantation genetic diagnosis: the ethical debate. Human Reproduction 18: 465–71.
- Scheper-HughesN(1990) Three propositions for a critically applied medical anthropology. Social Science and Medicine 30:189–97.
- Shalev C and Gooldin S (2006) The uses and misuses of invitro fertilization in Israel: some sociological and ethical considerations (with Carmel Shalev). NASHIM – Journal of Jewish Women’s Studies and Gender Issues 12:151–76.
- Smedley BD et al (2003) Unequal Treatment: confronting racial and ethnic disparities in health care. Washington: The National Academy Press.
- Sperling D (2010) Commanding the ‘be fruitful and multiply’ directive: reproductive ethics, law, and policy in Israel. Cambridge Quarterly of Healthcare Ethics 19:363– 71.
- Stanley S, Zane N, Nagayama Hall GC et al (2009) The case for cultural competency in psychotherapeutic interventions. Annual Review of Psychology 60:525–48.
- Taylor C (1997) The politics of recognition. In: Heble A et al (eds) New Contexts of Canadian Criticism. New York: Broadview Press. pp. 98–131.
- Teal CR and Street RL (2009) Critical elements of culturally competent communication in medical encounter: a review and model. Social Science and Medicine 68:533–43.
- Teman E (2003) The medicalization of ‘nature’ in the ‘artificial body’: surrogate motherhood in Israel. Medical Anthropology Quarterly 17:78–98.
- vanBalen F and Inhorn M (2002) Interpreting infertility: a view from the social sciences. In: Infertility Around the Globe: new thinking on childlessness, gender, and reproductive technologies. Berkeley, CA: University of California Press. pp. 3–32.
- Westwood S (1994) Racism, mental illness and the politics of identity. In: Rattansi A and Westwood S (eds) Racism, Modernity and Identity on the Western Front. Cambridge: Polity Press, pp. 247–65.
- Wilson DW (2004) Cultural diversity: what do we fear? Diversity in Health and Social Care 1:145–50.