Keywords
Cultural competency; Indigenous; Ethnic minorities; Health disparities; Cultural competency training; Health curricula
Introduction
Cultural competence is a broad concept used to describe strategies designed to ensure that health professionals are able to provide quality health care to diverse populations [1]. Over the last ten years or so, the term ‘cultural competence’ has become prominent in the health and medical education literature. According to Betancourt (2006), ‘physicians need a practical set of tools and skills that will enable them to provide quality care to patients everywhere, from anywhere, with whatever differences in background that may exist…’ Consistent with this imprimatur, most medical and nursing schools must provide some level of training in this area to meet accreditation requirements and therefore now include some level of cultural competency education and training in their curricula [2-4]. For example, in Australia, cultural competency is endorsed by the Australian Medical Council (AMC) and medical courses must provide cultural competency training in their curricula to meet accreditation requirements. Although these requirements ensure that cultural competency is included in health and medical curricula, there is variation between health and medical schools in the content and delivery of this training [2,5].
Several reviews have examined the effects of cultural competence interventions on trained health professionals [6-8]. The findings of these reviews demonstrate that cultural competence training can be effective for improving health professionals’ knowledge, attitudes and skills and patient satisfaction [6-9]. Despite the promise of cultural competency training, there has been little systematic evaluation of its potential impact when included in the university-based professional training of health professionals. The purpose of this study was to conduct a systematic review of the peer reviewed literature to, firstly, identify published evaluations of cultural competence education and training interventions in health and medical curricula; secondly, to describe the key characteristics and outcomes of these evaluations to determine which strategies are effective for improving the cultural competence of students undertaking university-based health professional training; and third, to critique their methodological quality using standardised criteria.
Methods
This review is derived from a broader review of the cultural competence literature. Specifically, studies included in this review were identified from a larger systematic search of the literature for cultural competency interventions in health care for Indigenous peoples and other minority ethnic/cultural groups in Australia, New Zealand, Canada and the United States.
Search strategy
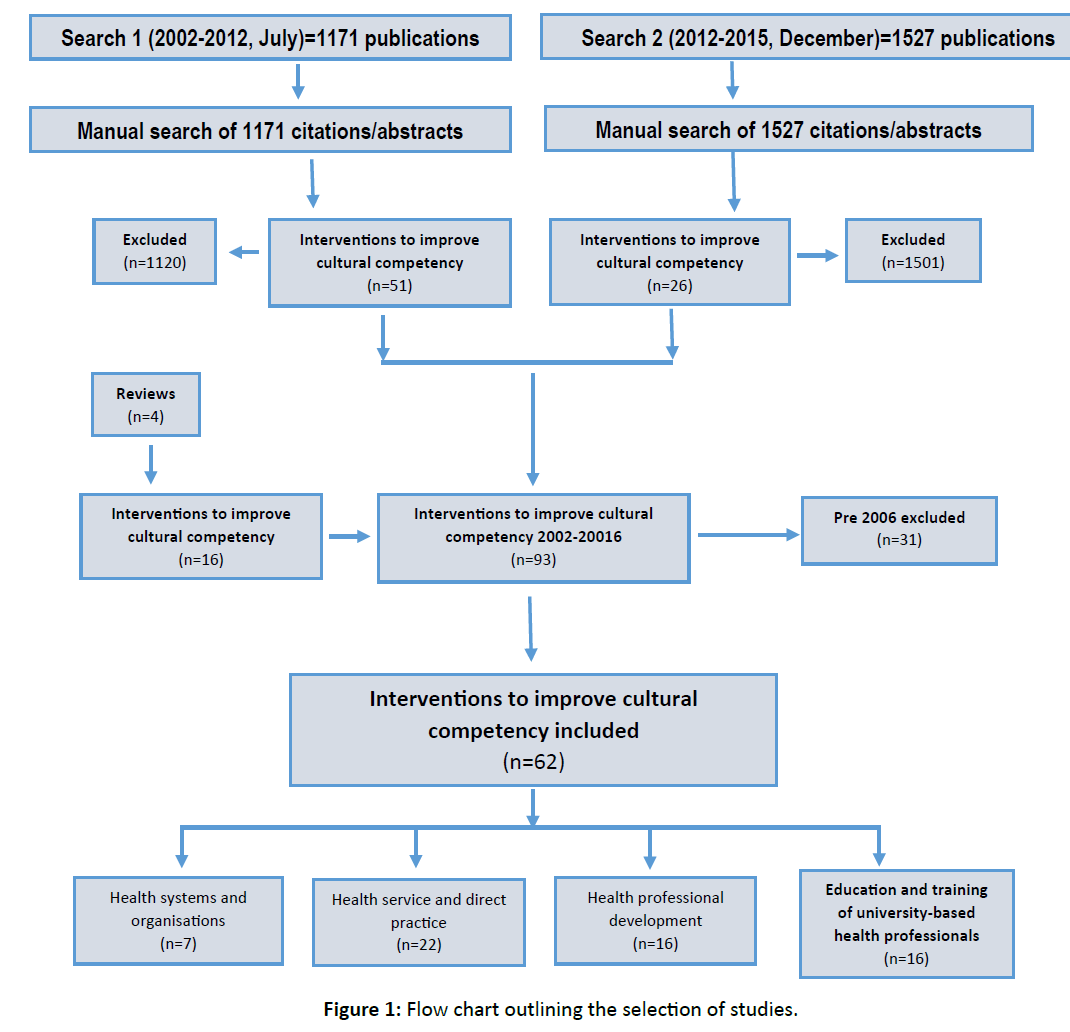
The search strategy employed for the broader review comprised six steps, including an initial search in 2012, for the period 2002-July 2012 (Search One) and an additional search in 2016 for the period 2012-2015 (Figure 1).
Step 1: A qualified archivist (MK) searched 17 relevant electronic databases for the period 2002 to 2012, July (Search One) identifying 1135 publications, after the removal of duplicates.
Step 2: Relevant clearinghouses and websites from each of the four countries were searched for grey literature publications. Thirty additional publications were identified.
Step 3: The reference lists of seven reviews identified in Step 1 were examined manually. Six additional publications were identified.
Step 4: The 1171 publications identified were imported into Endnote and their abstracts manually examined for studies meeting the following inclusion criteria. Fifty-one studies met inclusion criteria.
Step 5: Steps 1, 2, 3 & 4 were repeated again in June 2016 in a search update (Search Two). The search terms used were modified slightly in an effort to capture further relevant literature. Some websites previously searched for grey literature publications were no longer available so similar relevant websites and clearinghouses were identified and searched (Figure 1). The updated search identified 1527 publications, 1511 from the electronic database search and 16 from the grey literature search.
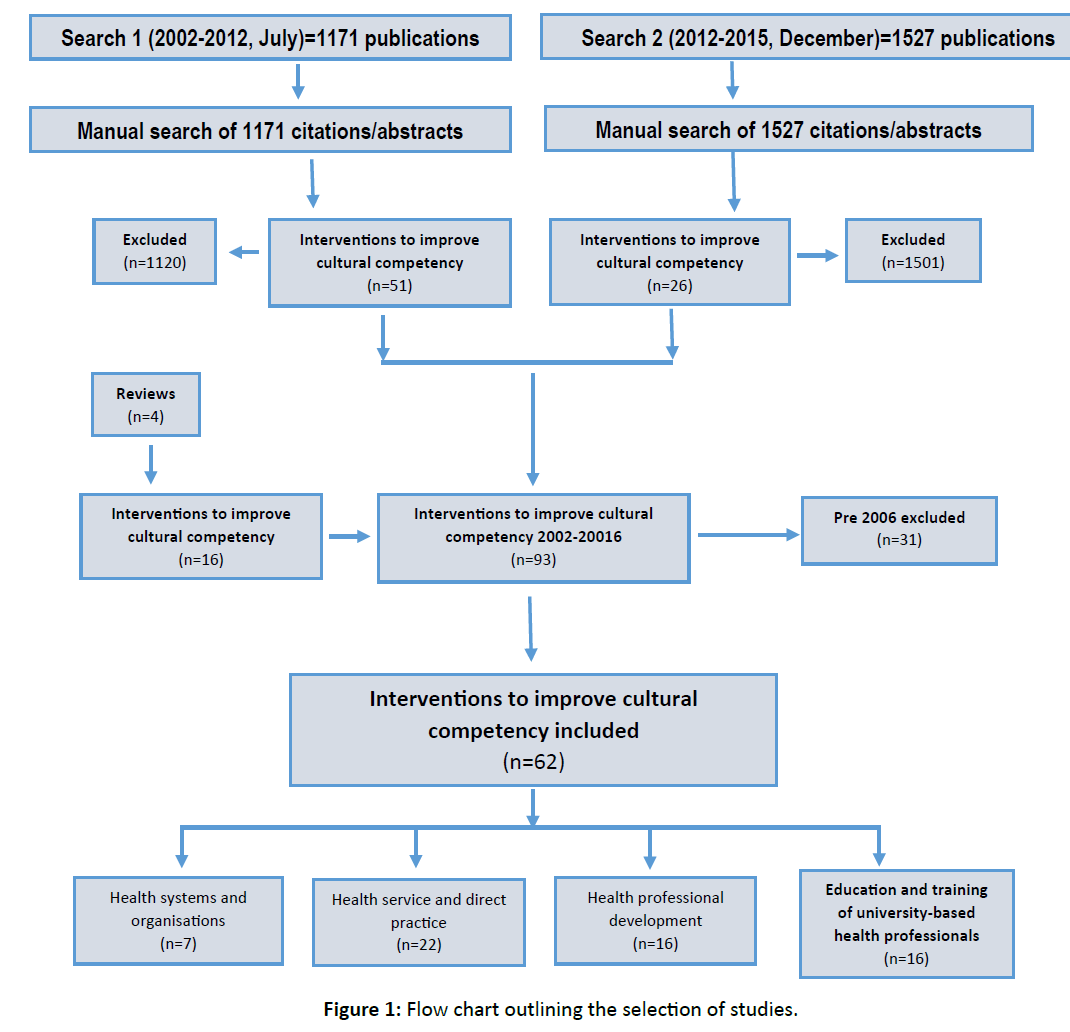
Figure 1: Flow chart outlining the selection of studies.
Search One and Two were imported separately into EndNote X7 and their duplicates removed. Given the findings of a review of cultural and linguistic competence in health care (9), it was decided to include only studies published from 2006-2015 (inclusive).
Studies were included if they met the following criteria:
1. Published in English from 2006 to 2016 (inclusive)
2. From Australia, Canada, New Zealand or the United States;
3. Focused on cultural competence and Indigenous or other racial or ethnic groups; and
4. Evaluations or trials of interventions (e.g. programs, services or policies) designed to improve cultural competence in health care.
Fifty-one studies met inclusion criteria.
Step 5: Steps 1, 2, 3 & 4 were repeated in June 2016 in a search update (Search Two). The search terms used were modified slightly in an effort to capture additional relevant literature. Some websites previously searched for grey literature publications were no longer available so similar relevant websites and clearing houses were searched (Figure 1). The updated search identified 1527 publications, 1511 from the electronic database search and 16 from the grey literature search. Twenty-six studies met inclusion criteria.
Identification, screening and inclusion of publications
The titles and abstracts of the 51 publications from Search One were screened by co-author RB, and the 26 publications from Search Two were further screened by co-author CJ for evaluations of trials or trials of interventions designed to improve cultural competence in health care (Figure 1). The full texts of the remaining publications were screened by blinded reviewers (RB, JM, AC, KT). Disagreements were resolved by discussion and consensus. A total of 62 intervention publications were identified (Figure 1). Of these 62 intervention studies, 16 evaluated cultural competence training and/or education interventions targeting university based training health professionals. It is these 16 studies that are the focus of this review.
Data extraction and analysis
Data extracted from the full texts of the 16 studies included publication authorship, year and type, country, population and sample size, intervention setting, intervention type and strategies, study design, outcome measures, and outcomes reported. The quality of studies primarily employing quantitative methods was assessed using the Effective Public Health Practice Project quality assessment tool [10]. Studies primarily employing qualitative methods were assessed using the Critical Appraisal Skills Programme quality assessment tool [11].
Results
Characteristics of intervention studies
Table 1 summarises the sixteen studies evaluating cultural competence training and/or education interventions targeting university based training health professionals and describes the characteristics of their evaluations. Eight of the sixteen intervention studies were conducted in Australia [13,17-19,21-24,] and eight in the United States [12,14-16,20,25-27] Fourteen studies targeted undergraduate and two postgraduate university-based training health professionals. Medical students were the most common student group targeted, with five studies targeting this student group [12- 14,22,24]. Four studies targeted nursing students [19,20,23,27], three health science students [16,18,26] and two each psychology [17,25] and pharmacy students [15,21]. The sample size of study participants ranged from 31 to 1974 students. Three main types of education and training intervention strategies were employed by studies: Integration of cultural competency into core or elective curriculum; cultural immersion; and cultural awareness training. Strategies were evaluated using quantitative, qualitative or mixed methods.
Intervention strategies
Table 2 summarises the core components of education and/ or training strategies (content, delivery mode, type of participant assessment and outcomes measured) targeting university based training health professionals (Table 2).
Integration of cultural competence curriculum
Nine studies integrated cultural competency education/ training into university curriculum for delivery to medical, nursing, health science, pharmacy and/or psychology students [12-20]. Cultural competency curriculum was implemented into core or elective units of study [12,13,20]. Although the content of cultural competency education varied considerably across integration strategies, content areas most commonly reported related to cultural differences culturally competent health care and health disparities [12-20].Content was primarily delivered using a mix of didactic (e.g. lectures), interactive (e.g. tutorials) and experiential (e.g. case scenarios) teaching methods [12,13,15,19,20]. The duration of delivery varied from 6 hours of didactic and interactive sessions over 5 weeks to a one year program of didactic lectures, monthly meetings, mentoring and personal reflection [12, 14]. Measured outcomes of cultural integration interventions focused on participants’ knowledge of and attitudes to factors related to cultural competency, and their perceptions and experiences of receiving cultural competency education [14-16,18-20]. Knowledge outcomes measured by studies focused on participants’ knowledge of cultural factors and specific Indigenous health problems. Attitude outcomes measures related to participants’ perceptions of different cultural groups and their readiness to work in cross cultural situations. Confidence outcomes most commonly measured participants’ confidence to interact with clients from different cultural groups. Six out of the nine integration studies assessed pre-post changes in measured outcomes, with improvements related to knowledge of cultural competence, attitudes towards working with Indigenous people, and awareness of cultural differences most commonly reported [13-16,19,20].
| 1st author, year of publication |
Country |
Setting and study population |
Intervention Type and Strategy |
Study design and method |
Outcome measures |
Primary Outcomes |
| Castillo et al. (2010) [12] |
U.S. |
13 medical/paediatric students in global scholars program |
Integration
Elective unit in global health |
Post-test
Qualitative (thematic) analysis of journal entries |
Perceptions of skills and cultural competency |
N/A |
Sanner et al. (2010)
[27] |
U.S. |
47 university nursing students |
Education
Cultural diversity Forum |
Pre-post test
Survey |
Openness to diversity |
Significant increase (p<0.0001) in levels of cultural sensitivity |
Chiodo et al. (2014)
[17] |
Australia |
113 psychology students |
Integration
Intercultural Psychology unit |
Post-test
Survey |
Student learning outcomes |
Increased understanding of cultural diversity issues
Development of critical self-reflection on values and assumptions, culturally awareness |
Kickett et al. (2014)
[18] |
Australia |
745 1st year health science students |
Integration
Core unit in Indigenous health |
Post-test
Survey |
Qualitative survey items only reported: Satisfaction and self-reported awareness |
Self-reported increased knowledge and awareness
94% satisfaction for semester 1 cohort (n=147)
76% satisfaction for semester 2 cohort (n=598) |
Smith et al. (2015)
[24] |
Australia |
271 1st year medical students |
Immersion
Core cultural immersion program |
Post-test
Survey and group interviews |
Satisfaction |
Reported outcomes relate to student perceived value and quality of program |
Thackrah et al. (2013)
[19] |
Australia |
University: Midwifery school
16 × 1st year midwifery students |
Integration
Core unit in Indigenous cultures |
Pre-post
Survey, interviews and participant observations |
Attitudes |
Increase in positive attitudes towards Indigenous people from 63.3%-75.6%. as measured by an “attitude thermometer” |
Steinfeldt and Wong (2010)
[25] |
US. |
46 Counselling Masters students (22-50 years, mean age 25.7 years; 81% female) |
Education
Multi-cultural training |
Pre-post with parallel control group
Survey |
Racial attitudes, awareness of offensiveness of native theme mascots |
None |
Walton (2011)
[26] |
US |
65 Health science students; 30 student nurses (18-45 years; 70% female) |
Education
60 min presentation delivered by nurse |
Pre-post without control group survey |
Knowledge, awareness. Beliefs. Attitudes and critical reflection |
None |
Paul et al. (2006)
[13] |
Australia |
224 medical students |
Integration
Core and elective Aboriginal Health Curriculum |
Cohort with historical control survey |
Attitudes to Aboriginal health; readiness to work in Aboriginal health |
Significant improvements (p<0.05) in: preparedness to work with Aboriginal people; play an advocacy role; and responsibility to work for change in Aboriginal health |
Genao et al. (2011)
[14] |
U.S. |
109 3rd year medical students: 47control and 62 intervention group |
Integration
Core cultural competence training for 3rd year medical students |
Randomised controlled trial survey |
Change score in cultural competence |
19% increase in knowledge in intervention group vs. 4% in controls (p<0.01) |
Bennett et al. (2013)
[23] |
Australia |
31 undergraduate nursing students |
Cultural immersion
Elective 5 day education program and clinical placement |
Pre-post
Confidence logs and focus group interviews |
Confidence in interacting with Indigenous clients |
Increased confidence to do the following with Indigenous Australians: communicate (26.6%); provide culturally appropriate care (28.4%); meet their needs (49.1%); ask about their healthcare needs (40%); relocate to work in remote area health care services (36%) |
Morrissey and Ball (2014)
[21] |
Australia |
29 1st year pharmacy and clinical sciences students |
Cultural Immersion
Core 5 day Cultural immersion (5 day trip) |
Pre- and post-questionnaire: Modern Racism Scale (MRS), Attitudes Towards Indigenous Australians (ATIA) scale and reflective journals |
Level of knowledge and attitude |
In relation to attitudes towards Indigenous Australians, increases in positive attitude (62%-73% and 66%-83%); empathy (34%-48%); impartiality (51%-62%) and decreases in partiality (61%-57%) |
Benson et al. (2015)
[22] |
Australia |
University of Adelaide |
Cultural Immersion
Elective 2 day experience in a remote Aboriginal community |
Pre- and post-survey and reflections |
Student expectations and understanding |
Students reported increased understanding and insight, including a deepened understanding of the social and cultural determinants of health |
Vyas and Caligiuri (2010)
[15] |
U.S. |
25 2nd and 3rd year pharmacy students |
Integration
11 hours of cultural education over two semesters of pharmacy program |
Pre-post survey and post-test reflection |
Awareness and Attitudes |
Significant improvement in awareness of health beliefs (p<0.022) and different cultures (p<0.046) |
Musolino et al. (2010)
[16] |
U.S. |
University
1,974 Interdisciplinary health science students: Medicine, pharmacy, nursing and physical therapy |
Integration
Core Cultural Competency and Mutual Respect (CCMR) educational program |
Pre-post survey with control group
Inventory for assessing the process of CC among healthcare professionals |
Cultural Competence (CC) scores using Campinha-Bacote’s Inventory for Assessing the Process of Cultural Competence-Revised
(IAPCC-R) |
Increase in cultural awareness but not cultural proficiency |
Jeffreys and Dogan (2012)
[20] |
U.S. |
183 Associate degree nursing students |
Integration
Cultural competence education |
Pre-post with control group
Survey |
Changes in transcultural self-efficacy (TSE): Confidence in knowledge and practice, attitudes, values and beliefs |
Compared with novice students, advanced students´ scores were higher for all TSE subscales in both cross-sectional and longitudinal study designs |
Table 1: Characteristics of interventions studies evaluating cultural competence training and/or education interventions targeting university based training health professionals.
| Publication |
Strategy |
Content |
Delivery Mode |
Assessment |
Outcomes Measured |
| Castillo et al.(2010) [12] |
Integration
Paediatric residents |
Burden of Global disease
Immigrant/undeserved health
Traveller’s medicine |
Elective: Didactic lectures; mentoring; reflective journaling |
Reflective journal |
Perceptions of experiences
Established core Competency domains applied to code participant data |
| Chiodo et al. (2014) [17] |
Integration
2nd year psychology students |
Intercultural psychology
Identity and wellbeing of Indigenous Australians impacts of colonisation, racism and white privilege; immigration; community responses to racism |
6 weeks: 2 × 1 hour lectures, 1 hour tutorial, case studies, digital resources |
Reflective journal |
Knowledge, attitudes |
| Paul et al. (2009) [13] |
Integration
Aboriginal health across medical curriculum |
Aboriginal health |
Compulsory: 3 problem-based tutorials; lectures
Elective: Aboriginal health orientation; tutorials; and self-directed learning |
Assignments, PBLs, exam questions |
Perceptions of Aboriginal health as a social priority; Aboriginal health issues and service provision; and preparedness and ability to work in Indigenous health |
| Genao et al. (2009) [14] |
Integration
3rd year medical student cohort |
Health disparities; disease incidence/prevalence stereotyping; exploring culture; perception of health and illness; communication/language |
Compulsory: 5 consecutive weekly sessions: 1× 2 h, 4 × 1 h
Vignettes; open discussion; and Q&A |
None |
Knowledge of cross-cultural issues in medicine |
Kickett et al. (2014)
[18] |
Integration
Compulsory 1st year unit for health science students |
Indigenous cultures and health: International Indigenous health; Australia’s Indigenous peoples; Past policies and practices; Significance of identity; social determinants; family and community structure; case study; communication; and cultural safety |
Compulsory: 12 weeks: tutorials, workshops, vodcasts, reflective journals |
Reflective journal, e-tests, group presentations |
Perceptions of and satisfaction with program |
Thackrah and Thompson (2013)
[19] |
Integration |
Indigenous diversity; international comparisons; family structure, policies and practices; cultural beliefs in health contexts and professional practice issues |
Compulsory 12 × 2 h tutorials, including vodcasts, case studies and student presentations |
|
Perceptions and experiences of program |
Vyas and Caligiuri (2010)
[15] |
Integration
Core lectures |
Population demographics; health disparities; cultural differences; language barriers, religious beliefs, alternative medicine |
Compulsory 6 weeks, 11 h of instruction: lecture, scenarios and discussions |
|
Attitudes, awareness
Previously tested instrument |
Musolino et al. (2010)
[16] |
Integration |
|
Cultural Competency and Mutual Respect (CCMR) educational program |
|
Attitudes, knowledge, skills, encounters and desire
Validated tool |
Jeffreys and Dogan (2010)
[20] |
Integration
Integrated cultural competency in associate nursing degree |
Education: Cultural assessments, similarities and differences between cultural groups, dimension of acculturation, and importance of culturally competent health care
Application: concepts, skills and values to patient scenarios |
8 weeks of cultural competence education in lectures, nursing skills lab and clinical followed by application in patient scenarios |
|
Knowledge of cultural factors; confidence for interviewing clients from different cultural backgrounds; and attitudes, practices and beliefs towards different cultural groups.
Transcultural self-efficacy tool (validated tool) |
Sanner et al. (2010)
[27] |
Education |
Introduction, patient care scenarios and discussion: cultural diversity, health literacy and health disparities |
3 h: 45 min nurse educator presentation followed by interactive activity |
|
Awareness, attitudes |
Steinfeldt and Wong (2010)
[25] |
Education |
Knowledge about the negative impact of native themed mascots |
Compulsory 45 min training presentation on culturally-sensitive counselling practices with Native American clients versus 45 min presentation addressing issues important to the use of Native-themed mascots to improve multicultural competence |
|
Awareness of racially offensive behaviours; attitudes about native themed mascots |
Walton (2011)
[26] |
Education |
Findings of a native American research study: Native American traditions, practices, values and health challenges |
60 min presentation followed by discussion |
|
Cultural knowledge and awareness; application of cultural knowledge and awareness; beliefs, attitudes |
Bennet et al. (2013)
[23] |
Immersion |
Cultural education, primary health care theory and practice, community integration, resilience, person centred care and rural and remote practice, and clinical placement in Indigenous health |
5 day educational orientation program followed by rural and remote clinical placements |
|
Confidence in interacting with Indigenous clients: communicating, providing culturally competent health care; understanding needs of Indigenous clients; asking Indigenous clients about their health care |
Morrissey and Ball (2014)
[21] |
Immersion |
Cultural awareness, kinship system, historical events, milestones in Indigenous Australian society, social determinants and their impact on Indigenous health and well-being, closing the gap policy, and skills for working in Aboriginal health |
5 day visit to remote Aboriginal communities and health services |
|
Knowledge of and attitudes to Indigenous Australians |
Benson et al. (2015)
[22] |
Immersion |
Working in clinic and helping out in the community |
Elective 2 day clinical and community placement in a remote Aboriginal community |
|
Perceptions of experiences |
Smith et al. (2015)
[24] |
Immersion |
Cultural and historical aspects of native Hawaiian health, native concepts of health, knowledge and care. |
1.5 days, 50 min cultural education, history maps, talking circles, cultural survival session |
|
Program satisfaction |
Table 2: Core components of cultural competence education and/or education interventions
Cultural immersion
Four studies employed cultural immersion as the main strategy [21-24]. Cultural immersion strategies included three key components: education sessions, clinical placements and community experience. The duration of cultural immersion programs ranged from 1.5 to five days. The scope of content commonly delivered by the educational component of cultural immersion programs targeted participants’ cultural knowledge and awareness. Clinical placement and community experience components of immersion strategies targeted students’ attitudes to Indigenous peoples, confidence to interact with Indigenous people and their perceptions of the cultural immersion experience. Two cultural immersion studies assessed prepost changes in measured outcomes [21-23]. Improvements in measures related to students’ attitudes towards Indigenous people interacting with Indigenous people and providing culturally competent health care were reported. The other two studies assessed students’ perceptions of and/or satisfaction with the cultural immersion experience [21-24].
Cultural education and training
Three studies delivered cultural education to students in nursing, health science and counselling fields [25-27]. Education sessions were delivered using didactic and/or interactive sessions of 45 minutes 60 minutes and 3 hours duration [25-27]. Measured outcomes related to cultural competency included knowledge of cultural concepts, attitudes to and awareness of racial stereotypes and cultural sensitivity [25-27]. All three studies assessed prepost changes in outcomes measured, with statistically significant improvements in students’ cultural knowledge and attitudes towards racially offensive behaviour and cultural diversity[25-27].
Methodological quality
Eleven studies conducted a quantitative and five studies a qualitative evaluation [12-20,21-24]. The methodological quality of quantitative and of qualitative studies (Table 3 and 4). Nine out of the ten studies conducting a quantitative evaluation employed a pre–post study design) five of which employed a control group and one randomization [12, 14-16, 20, 21,23,25- 27]. No studies employing a control group reported blinding, although the nature of interventions implemented would make effective blinding difficult. Two of the five studies employing a control group were rated strong for confounding; one reported no important differences between groups prior to the intervention and the other controlled for differences in the analysis [14, 16]. The other four studies were rated weak because differences between groups were not reported or not controlled for in the analysis [12, 16, 20, 25]. Six out of the 10 quantitative studies collected outcome data using a previously tested or validated instrument. For the other four studies, the measurement instrument was not validated or adequately reported [12, 14- 16, 20, 25,27]. Two-thirds of studies rated weak for selection bias on the basis that the percentage of individuals consenting to participant was unclear or less than 60%, and/or rated weak for withdrawal and dropouts on the basis that less than 60% of participants completed the study. Two studies provided a citation to justify their method of statistical analysis [19, 24]. No study reported economic costs.
| 1st Author (year) |
Selection bias |
Study design |
Confounders |
Data collection |
Withdrawal and dropouts |
Morrisey and Ball (2014)
[21] |
Strong |
Moderate |
NA |
Strong |
Weak |
Paul et al. (2006)
[13] |
Moderate |
Moderate |
Weak |
Strong |
Moderate |
Bennett et al. (2013)
[23] |
Weak |
Moderate |
Weak |
Weak |
Strong |
Genao et al. (2009)
[14] |
Strong |
Strong |
Strong |
Strong |
Weak |
Sanner et al. (2010)
[27] |
Weak |
Moderate |
NA |
Strong |
Weak |
Steinfeldt and Wong (2006)
[25] |
Moderate |
Moderate |
Weak |
Strong |
Strong |
Walton (2011)
[26] |
Weak |
Moderate |
NA |
Weak |
Weak |
Smith et al. (2015)
[24] |
Weak |
Weak |
NA |
Weak |
Weak |
Jeffreys and Dogan (2012)
[20] |
Weak |
Moderate |
NA |
Strong |
Weak |
Vyas and Caligiuri (2010)
[15] |
Weak |
Moderate |
NA |
Moderate |
Weak |
Musolino et al. (2010)
[16] |
Weak |
Moderate |
Strong |
Strong |
Weak |
* NR, Not Reported; NA, Not Applicable.
Table 3: Methodological quality of quantitative studies.
| 1st Author (year) |
Clear Aims |
Appropriate methodology |
Appropriate research design |
Appropriate recruitment strategy |
Appropriate data collection |
Considers relationship between researcher and participants |
Ethical issues considered |
Appropriate data analysis |
Clear statement of findings |
Value of research discussed |
| Benson et al. (2015) [22] |
Yes |
Yes |
Unclear |
Yes |
Unclear |
Yes |
Yes |
Yes |
Unclear |
No |
| Kickett et al. (2013) [18] |
Yes |
Yes |
Unclear |
Yes |
Yes |
No |
Unclear |
Yes |
Yes |
Yes |
| Castillo et al. (2010) [12] |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
No |
Yes |
Yes |
Yes |
| Thackrah and Thompson (2013) [19] |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Unclear |
Yes |
Yes |
| Chiodo et al. (2014) [17] |
Yes |
Yes |
No |
Yes |
Yes |
No |
Unclear |
Yes |
Yes |
Yes |
Table 4: Methodological quality of qualitative studies.
The five qualitative studies were rated adequate on 70% to 90% of CASP criteria [21-24]. All five studies were rated adequate for aims, methodology and recruitment strategy criterion. The majority of studies were rated adequate for criterion related to the collection and analysis of data and the presentation and discussion of research findings. Ethical issues and the relationship between the researcher and the participants were rated adequate in <50% of studies.
Discussion
Consistent with previous reviews, a small number of published evaluations of cultural competency interventions were identified in the peer review literature and their methodological quality was less than optimal [6, 7]. No evaluation studies from Canada or New Zealand were identified, despite these countries having accredited cultural competence training programs [27, 28].
Strengths and limitations of interventions
Nine out of the 16 studies evaluated the integration of cultural competence education and training into health and medical curricula. This is encouraging given calls for cultural competence training of health professionals as part of a broad strategy to tackle health inequities and ensure quality health care for increasingly diverse populations [2, 29, 30]. Less encouraging was that only two studies evaluated the impact of integrating cultural competence education across the health and medical curricula within a program of study [13, 20]. The remaining seven studies evaluated the impact of integrating cultural competence education as discrete core or elective units of study [12, 14-19]. A review of Indigenous health curricula in health science courses found that in 17 out of the 35 studies identified, Indigenous health was integrated within the broader curriculum and not as a stand-alone element [5]. That only two of the studies in this review integrated cultural competency training within the broader curriculum suggests that the outcomes of this approach are not being evaluated or published in the peer review literature.
Our findings suggest that one indicator of the level of integration of cultural competency training is the level and type of student assessment. The two studies integrating cultural competence education within the broader health and medical curricula formally assessed students’ knowledge and skills in areas of cultural competence via examinations, assignments and case scenarios [13, 20]. The integration of cultural competency training and formalised assessment within the broader health and medical curriculum is consistent with a framework for implementing cultural competency training in the medical curricula [29]. The three components of this framework include: 1. creation of early classroom experiences to teach students the basic principles of culture and cultural diversity; 2. opportunities for students to engage in continued training of these early concepts throughout the pre-clinical years; and 3. the assessment and evaluation of knowledge and skills throughout the course [30]. Notably, for the seven studies integrating cultural competence education as a discrete unit of study, the second and third of these components were absent.
Four studies included in this review evaluated the impact of a cultural immersion experience on students’ knowledge and attitudes. This is heartening given that many of the challenges to improving health outcomes for Indigenous and ethnic minority populations relate to a lack of understanding among health care professionals of the contexts in which these populations live and their impacts of these contexts on their health care outcomes [29]. Consistent with the experiential focus of cultural immersion, evaluations of this strategy primarily assessed participants’ experiences and perceptions using qualitative methods. Future evaluations of cultural immersion programs could be strengthened by including outcome measures more closely linked to the primary rationales for implementing cultural immersion programs in health and medical curricula. These include increasing the number of health professionals who are culturally competent and/or willing to work with Indigenous and other ethnic minority populations, and the ensuing impact of these outcomes on health care and health outcomes of Indigenous and other ethnic minority populations [20,22].
Three studies evaluated the delivery of one-off cultural awareness education. Although cultural awareness education is an important component of an overall framework for cultural competence, it is generally insufficient to significantly change attitudes and in turn behaviour [5]. Improving these types of outcomes is likely to require structural changes at the level of the organisation, to reinforce and sustain behaviour change in health professionals [2]. Some strategies proposed for achieving this include embedding cultural competency in organisational policy, protocols and related key performance indicators [31]. Although there is some evidence that organisations that have integrated cultural competency standards into policies and practices influence health professionals to develop more culturally competent behaviours more rigorous research is needed in this area [32-34].
Methodological strengths and limitations of studies
Encouragingly, nine out of the 10 quantitative studies were rated moderate to strong for study design. Less encouraging, six of these studies did not employ a control group, making it difficult to attribute outcomes to the intervention. Five out of the 11 quantitative studies rated moderate or strong for study design also rated weak on at least two other methodological criteria, compromising their overall methodological quality. Selection bias and withdrawal and drop outs were rated weak for slightly more than one half of studies due to consent and/ or follow-up rates <60% and/or less than optimal reporting of these key methodological criteria. Variable reporting of an intervention evaluation makes it difficult for the intervention to be replicated or adapted for other populations and settings and implemented more widely [35]. Data used to measure outcomes was predominately collected using valid and reliable measurement instruments, with the exception of evaluations of cultural immersion programs in which two out of three studies were rated weak for data collection, increasing the potential for misreporting of outcomes assessed. No study reported costs. Economic analysis is important for understanding resources and the potential cost-effectiveness of intervention strategies designed to improve cultural competency in health care for Indigenous peoples and subsequent economic cost and social savings [36]. Overall, the evidence base for the effectiveness of cultural competency interventions targeting health and medical and students would be strengthened by quantitative evaluations that employ study designs with a control group, retain a higher percentage of study participants, control for confounding variables and conduct high-quality economic evaluations.
The methodological quality of the five qualitative studies included in this review was generally adequate, but could be strengthened with better reporting of ethical and methodological issues related to the role of the researcher.
Limitations
Although a rigorous and thorough search strategy was used, there is the possibility that the review did not locate all relevant studies. Relevant intervention evaluations may have been misclassified. However, a high level of agreement between blinded coders suggests otherwise. Since evaluations with positive findings are more likely to be published, it is possible that the published evaluations reviewed overestimate the true effectiveness of cultural competence education and training interventions included in the university based professional training of health care providers [37].
Conclusion
The quality of evidence derived from the studies reviewed is insufficient to provide a strong basis for recommending the inclusion of specific cultural competence education and training strategies in the professional training of university based health professionals. Notwithstanding, a number of clear recommendations for improving future evaluations can be posited. First, evaluations could be improved by more explicitly linking specific learner outcomes (e.g. knowledge and confidence to deliver culturally competent health care) to patient outcomes of interest (e.g. satisfaction, quality of health care and health outcomes), to determine the extent to which changes in outcomes of health professionals undertaking university based professional training translates to culturally competent health care delivery for patients. Studies comparing improvements in patient healthcare outcomes in disciplinary areas of medicine where medical and health professional schools include cultural competence curriculum with areas that do not might also be useful. Second, given the heterogeneity of cultural competence education and training strategies included in the professional training of university based health professionals, it would be helpful if future evaluations compared similar types of strategies (e.g. cultural competence education integrated into the curriculum as discrete versus related units of study). Third, researchers undertaking evaluations of cultural competence interventions should provide data on the resources and costs required for their implementation to enable economic analysis of the level of investment required to achieve a given outcome.
References
- Thackrah RD, Thompson SC (2013a) Refining the concept of cultural competence: Building on decades of progress. Med J Aust. 199: 35-38.
- Betancourt JR (2006) Cultural competence and medical education: Many names, many perspectives, one goal. Acad Med. 81: 499-501.
- Lyons Z, Laugharn EJ (2011) An overview of undergraduate training in cultural competency and cross-cultural psychiatry. ERP. 38: 57.
- Australian Medical Council (2010) Assessment and accreditation of medical schools: Standards and procedures.
- Ewen S, Paul D, Bloom GL (2012) Do indigenous health curricula in health science education reduce disparities in health care outcomes. Med J Aust. 197: 50-52.
- Clifford A, Mccalman J, Bainbridge R, Tsey K (2015) Interventions to improve cultural competency in health care for Indigenous peoples of Australia, New Zealand, Canada and the USA: A systematic review. Int J Qual Health Care. 27: 89-98.
- Truong M, Paradies Y, Priest N (2014) Interventions to improve cultural competency in healthcare: A systematic review of reviews. BMC Health Services Res. 14: 99.
- Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, et al. (2005) Cultural competency: A systematic review of health care provider educational interventions. Med Care. 43: 356.
- Crandall SJ, George G, MARION GS, DAVIS S (2003) Applying theory to the design of cultural competency training for medical students: A case study. Acad Med. 78: 588-594.
- National Collaborating Centre for Methods and tools Quality Assessment Tool for Quantitative Studies (2008) McMaster University: Hamilton.
- CASP UK (2013) Critical Appraisal Skills Programme(CASP) Qualitative Research Checklist. CASP UK, Oxford.
- Castillo J, Goldenhar LM, Baker RC, Kahn RS, Dewitt TG, et al. (2010) Reflective practice and competencies in global health training: lesson for serving diverse patient populations. J Grad Med Educ. 2: 449-455.
- Paul D, Carr S, Milroy H (2006) Making a difference: The early impact of an Aboriginal health undergraduate medical curriculum. Med J Aust. 184: 522.
- Genao I, Bussey-jones J, George DMS, Corbie-smith G (2009) Empowering students with cultural competence knowledge: Randomized controlled trial of a cultural competence curriculum for third-year medical students. Med J Aust. 101: 1241-1246.
- Vyas D, Caligiuri FJ (2010) Reinforcing cultural competency concepts during introductory pharmacy practice experiences. Am J Pharm Educ. 74: 129.
- Musolino GM, Shontol Torres Burkhalter S, Crookston B, Harris RM, Sue Chase-Cantarini RN, et al. (2010) Understanding and eliminating disparities in health care: Development and assessment of cultural competence for interdisciplinary health professionals at The University of Utah - A 3 year investigation. JOPTE. 24: 25.
- Chiodo LN, Sonn CC, Morda R (2014) Implementing an intercultural psychology undergraduate unit: Approach, strategies and outcomes. Austr Psychol. 49: 181-192.
- Kickett M, Hoffman J, Flavell H (2014) A model for large-scale, interprofessional, compulsory cross-cultural education with an indigenous focus. J Allied Health. 43: 38-44.
- Thackrah RD, Thompson SC (2013b) Confronting uncomfortable truths: Receptivity and resistance to Aboriginal content in midwifery education. Contemp Nurse. 46: 113-122.
- Jeffreys MR, Dogan E (2012) Evaluating the influence of cultural competence education on students’ transcultural self-efficacy perceptions. J Transcult Nurs. 23: 188-197.
- Morrissey H, Ball P (2014) Current research: First year pharmacy students' health services experience at the top-end of Australia. AJP. 95: 66.
- Benson J, Ryder C, Gill M, BalabanskI A (2015) A brief experience for medical students in a remote Aboriginal community. Aust Fam Physician. 44: 752.
- Bennett P, Jones D, Brown J, Barlow V (2013) Supporting rural/remote primary health care placement experiences increases undergraduate nurse confidence. Nurse Educ Today. 33: 166-172.
- Smith J, Wolfe CL, Springer S, Martin M, Togno J, et al. (2015) Using cultural immersion as the platform for teaching Aboriginal and Torres Strait Islander health in an undergraduate medical curriculum. Rural Remote Health. 15: 1-9.
- Steinfeldt JA, Wong YJ (2010) Multicultural training on American Indian issues: Testing the effectiveness of an intervention to change attitudes toward Native-themed mascots. Cultur Divers Ethnic Minor Psychol. 16: 110.
- Walton J (2011) Can a one hour presentation make an impact on cultural awareness? Nephrol Nurs J. 38: 21.
- Sanner S, Baldwin D, Cannella KA, Charles J, Parker L, et al. (2010) The impact of cultural diversity forum on students' openness to diversity. J Cult Divers. 17: 56.
- Caron N, Mackie J, Varley LC, Adams E (2015) Cultural competency—Canada’s history and today’s physician College of Physicians and Surgeons of British Columbia.
- Medical Council of New Zealand (2006) Statement on cultural competence.
- Rapp DE (2006) Integrating cultural competency into the undergraduate medical curriculum. Med Educ. 40: 704-710.
- National Health and Medical Research Council (2005) Cultural competency in health: A guide for policy partnerships and participation. Canberra.
- Bainbridge R, Mccalman J, Clifford A, Tsey K (2014) Cultural competency in the delivery of health services for Indigenous people.
- Betancourt JR, Green AR, Carrillo JE, Ananeh-firempong O (2003) Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 118: 293-302.
- Paez KA, Allen JK, Carson KA, Cooper LA (2008) Provider and clinic cultural competence in a primary care setting. Soc Sci Med. 66: 1204-1216.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I (2008) Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ. 337: a1655.
- Drummond MF, Mcguire A (2001) Economic evaluation in health care: Merging theory with practice, OUP Oxford.
- Easterbrook PJ, Gopalan R, Berlin J, Matthews DR (1991) Publication bias in clinical research. Lancet. 337: 867-872.