Keywords
cultural health capital, migrants, professional
experiences, psychosocial well-being, refugees,
subjective theories
Introduction
Recent estimates indicate that more than a third of
registered doctors (General Medical Council, 2011)
and one in twelve nurses (Royal College of Nursing,
2007) qualified outside the UK. The necessity for and
usefulness of a diverse healthcare workforce are consistently
highlighted in the European context (Bach,
2003). In the UK it is also acknowledged that the
healthcare sector relies on staff from migrant backgrounds
(Rechel et al, 2006). However, in this age of
super-diversity, making the best use of these people’s
resources is a complex matter, as professionals arriving
in the UK experience difficulties in transferring
and utilising their knowledge and skills (Phillimore,
2010).
The post-migration experiences of highly skilled
migrants and refugees in theUKare neither simple nor
straightforward (Psoinos, 2007). Studies of overseas
professionals from the healthcare and welfare sectors
indicate that they struggle to utilise their skills because
of interconnected reasons, such as complicated systems
for assessing and converting their educational
and professional qualifications, recruitment processes
and professional development which are often indirectly
discriminatory, racism experienced in the
workplace, and inadequate levels of local support and
mentoring (Butler and Eversley, 2009; Henry, 2007;
Sinclair et al, 2006; Smith et al, 2006). Studies exploring
these professionals’ post-migration experiences
also report poor psychosocial well-being outcomes,
such as low self-esteem, frustration, depression, demoralisation
and disappointment (Alexis et al, 2007;
Cohn et al, 2006; Stewart, 2003).
In this article we explore the meanings that overseas
doctors and nurses in the UK attach to their professional
experiences, and we examine the processes
that impede or facilitate their professional progress
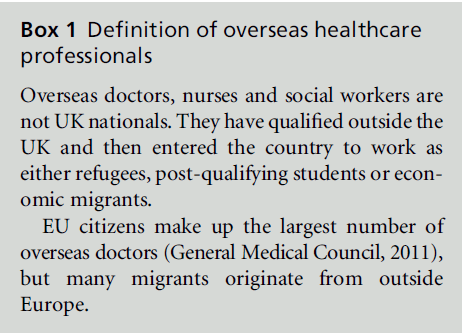
and influence their psychosocial well-being (see Box 1).
We do so by drawing on an innovative framework for
the interactional dynamics that occurs in healthcare contexts. We use the theoretical approach of cultural
health capital (CHC) (Shim, 2010) while exploring
the subjective theories of overseas healthcare professionals
in the UK institutions that employ them. The
aim is to highlight some of the micro-interactional
and also macro-structural mechanisms that affect the
development and well-being of these groups. Following
a brief literature review of the field of migration
of healthcare professionals, we discuss the CHC approach
and how it can address the shortcomings in
this area. We then employ this approach to analyse the
subjective theories conveying the professional experiences
of a group of overseas doctors and nurses in
the UK.
Box 1: Definition of overseas healthcare
professionals.
The components of CHC are defined by Shim
(2010, p. 3) as a ‘coherent collection of cognitive,
behavioural, social and cultural resources theorised to
serve as a ‘‘tool kit’’ for patients ... to optimise their
relationships with health professionals and the care
they receive.’ We argue that such resources can also
serve as a tool kit for overseas healthcare professionals,
who may activate them to improve relationships with
colleagues and service users in the healthcare institutions
in which they work. In our analysis of the
subjective theories of a sample of overseas doctors and
nurses we examine whether or not the participants
fully utilise these resources. Our proposition is that
those who cannot use their CHC effectively will
emerge as the most vulnerable in terms of professional
development and/or psychosocial well-being. We
conclude with recommendations about the barriers
that need to be addressed, and we discuss how these
professionals’ potential for the delivery of healthcare
can be utilised in the best possible way.
Post-migration experiences of
overseas healthcare
professionals
An increasing shortage of healthcare staff has led to
recruitment of these professionals from less developed
countries as one of the main responses of developed
countries to this challenge (Clark et al, 2006). The
main motives for this migratory movement include
poor remuneration, bad working conditions, political
instability and discrimination, as well as personal
motives such as a need for security, escape from the
threat of violence, and better education of children
(Pang et al, 2002). Common attracting factors are better
working conditions, better quality of life and greater
career opportunities. Migration of healthcare professionals
occurs in two ways, namely through active
recruitment by employers or agencies, or through
passive recruitment by professionals’ access to infor- mation and work opportunities via new communication
technologies (Batnitzky and McDowell, 2013;
David and Cherti, 2006; Troy et al, 2007).
In the UK, as far as post-migration experiences are
concerned, there is a growing research literature
examining either motivations and psychosocial processes
or socio-economic outcomes (Batnitzky and
McDowell, 2011; Cohn et al, 2006; Jones et al, 2009;
Larsen et al, 2005). In the first area, looking at psychosocial
processes, most studies draw on models of the
acculturation process (Ward, 1996) and acculturation
strategies (Berry, 1997) to explore, at the micro-level,
overseas professionals’ adaptation to the host society.
These classic models have been criticised on several
grounds, such as the lack of importance given to how
the host majority can shape and be shaped by migrants’
acculturation orientations, and the models have been
amended to include a more interactive dimension
(Montreuil and Bourhis, 2001).
In the second area, which looks at socio-economic
dimensions, most studies draw on theories such as
that of Loury (2002) on how racial/ethnic inequalities
are structured, and they often use the theory of Bourdieu
(1986, 2001) about the forms of cultural capital ,while
exploring highly skilled migrant groups’ integration
into the receiving society’s labour market. According
to Bourdieu (1986), migrants’ cultural capital refers to
non-financial assets, that is, the educational, intellectual
and social resources that people either inherit from
their family through socialisation or consciously acquire
over time, for instance, through formal education.
Cultural capital includes formal or institutionalised
cultural capital, such as educational and professional
qualifications and recognised work experience, as well
as informal/incorporated cultural capital, such as migrants’
affiliation to ethnic communities and social
and professional networks both in their country of
origin and the host country, and the values, motivation
and the strategies that they use to cope with
change.
Bourdieu’s theory of cultural capital has been
criticised for not paying enough attention to people’s
self-concept, because Bourdieu assumes that professionals
seek to maximise their status out of habit
(Lamont, 2010). In contrast, Lamont (2002) conceptualises
cultural capital as stemming from people’s
self-worth, and she assigns to cultural capital a nuance
which is both habitual and purposeful.
Criticisms of these two theories of acculturation
and cultural capital, when applied to research with
overseas professionals, suggest that psychosocial acculturation
models focus too much on intra-individual
or interpersonal states. Consequently, they cannot
explain the macro-mechanisms that suppress collective
minority rights and perpetuate socio-economic inequalities
between native-born and foreign populations
(Rudmin, 2003). Criticisms of sociological approaches such as cultural capital do not explain
the psychological processes which are co-constructed
in sociocultural contexts (Garcı´a-Ramı´rez et al, 2010)
and through which people respond to the challenges
that they face during acculturation.
The need for conceptual frameworks that look
beyond the agency–structure dichotomy and constructively
blend the personal with the collective is widely
acknowledged (Flyvbjerg, 2001; Heron and Reason,
2001; Stephenson and Papadopoulos, 2006). In accordance
with this view, we highlight the CHC framework
with ‘its simultaneous focus on biography and
social structure’ (Lareau, 2003, p. 311; Shim, 2010, p. 4,
note 6). Such frameworks are rooted in Bourdieu’s
conception of culture as an emergent set of resources
critical to the exercise of professional power and
embedded in the habitus of healthcare systems. Moreover,
CHC is a specialised form of cultural capital that
is leveraged in healthcare contexts to lead to more
effective engagements with providers of care.
The theoretical framework of
cultural health capital
Cultural health capital is ‘the repertoire of cultural
skills, verbal and nonverbal competencies, attitudes
and behaviours and interactional styles, cultivated by
patients and clinicians alike, that, when deployed, may
result in more optimal healthcare relationships’ (Shim,
2010, p. 1). These attributes of CHC are specific to a
given socio-historical moment. Shim (2010) points
out that in the current US healthcare system, with its
emphasis on patient initiative, self-knowledge and
self-management, certain features tend to be rewarded
in healthcare contexts and clinical interactions. These
features include health literacy, which is ‘the degree to
which individuals have the capacity to obtain, process
and understand basic health information and services
needed to make appropriate health decisions’ (Ratzan
and Parker, 2000, p. vi), knowledge of what information
is relevant to healthcare personnel, an enterprising
disposition which presupposes a sense of mastery
and self-efficacy, an orientation towards the future and
its control through action, sensitivity to interpersonal
dynamics and the ability to adapt one’s interactional
styles (Shim, 2010, p. 3).
In drawing parallels with cultural capital, Shim
(2010, p. 4) points out that CHC is similarly:
1 purposeful, since patients enact health-related practices
such as engaging in self-surveillance and risk
reduction, but also habitual in that many patients
engage in the above practices because these are
rooted in their experiences and long-lasting ways
of organising action
2 empowering for individuals, and structurally restricted
because holders of CHC are not entirely free
agents who can use resources at will, but are also
constrained by systematic inequalities
3 deeply relational because, in interacting with patients,
clinicians can encourage them to be the kinds of
actors they would like them to be.
This description of CHC suggests that this is indeed
one of the integrative theoretical frameworks that
combine agency and structure. Moreover, similarities
between the American and British healthcare systems,
in terms of an emphasis on ill health prevention and
risk reduction, maximising people’s capabilities through
lifelong learning and enabling them to have control
over their lives, and citizen participation and community
engagement in healthcare decision making,
indicate that this framework can be applied to the
current UK healthcare context (Marmot, 2010).
Through our analysis in the following sections, we
show that the CHC theoretical framework can be
valuable for exploring the repertoire of competencies,
attitudes and interactional styles that not only patients
but also healthcare professionals cultivate. It may also
highlight social inequalities in clinical encounters, and
help to explain how barriers that overseas healthcare
professionals may face at the workplace shape their
professional development and well-being.
The study
The project aimed to explore the experiences of
overseas health and social care professionals before
and after migrating to the UK, and the relevance of
cultural capital for their professional development.
The project focused on medical doctors, nurses and
social workers, as these professions attract the majority
of overseas-trained professionals in health and
social care (Bach, 2003). We employed purposive
sampling to recruit 5 doctors, 5 nurses and 5 social
workers via our professional networks in London. For
the purposes of this article, we discuss findings referring
to the doctors and nurses in our sample. The
Faculty Research Ethics Committee issued a favourable
opinion. All participants were ensured of confidentiality
and anonymity with regard to the accounts
that they provided.
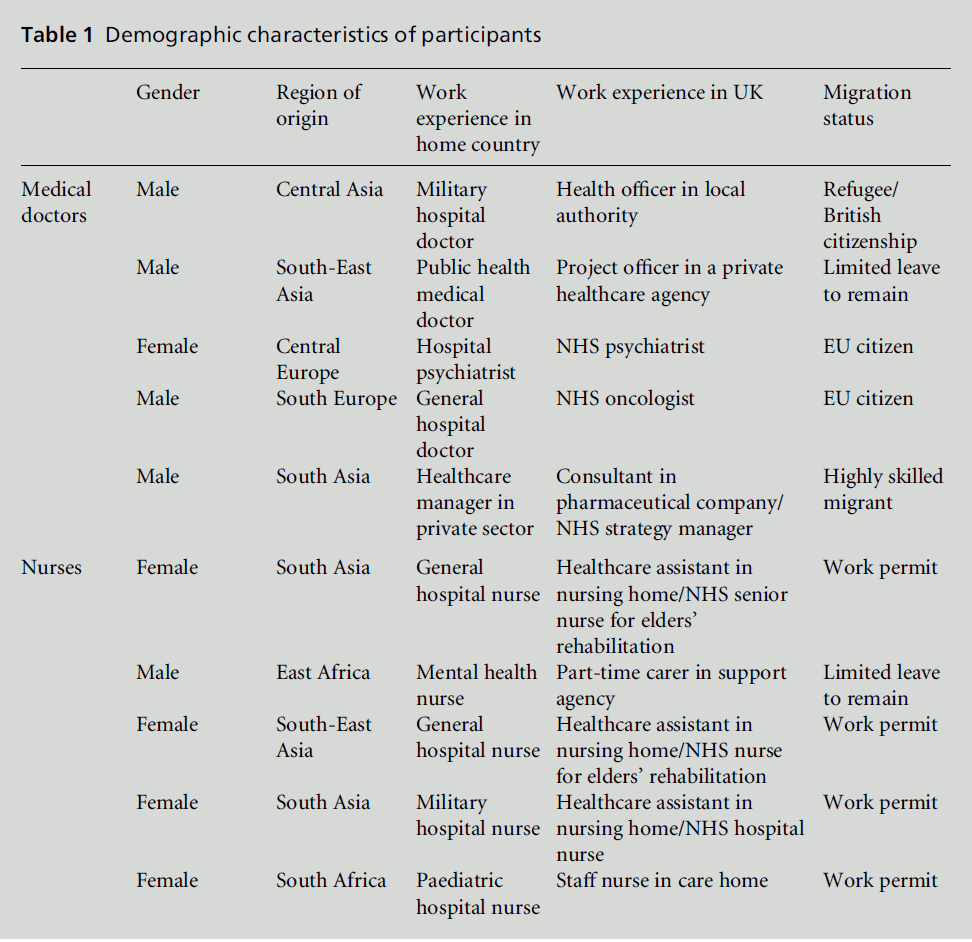
Participants
The study participants originated from a mix of
developing and European countries, and their ages
ranged from28 to 52 years. Two participants were EU
citizens, and four were economic immigrants with
work permits. One was on the Highly Skilled Migrant Programme (HSMP), one was a refugee with British
citizenship, and two were asylum seekers with limited
leave to remain (LLR) (see Table 1).
The sample of doctors consisted of four men and
one woman. Four had lived in theUKfor an average of
five years. One arrived in the early 1990s as a refugee,
and although he had lived in the UK for much longer
than the other participants, we still consider his
experience to be relevant since, at the time of the study,
he was still actively trying to join the UK medical
workforce. All of the doctors had a university degree in
medicine and significant work experience in their
home countries and elsewhere. Two were working as
doctors in NHS hospitals. One had a managerial post
in the NHS, the refugee doctor with British citizenship
worked as a health officer in a local authority, and the
doctor with LLR status was a project officer in a private
healthcare agency.
The sample of nurses consisted of four women and
one man; they had lived in the UK for an average of
seven years. All of them had nursing qualifications
from their home countries, and one also had a degree
in socialwork. They had significant work experience in
their home and other countries. Three were employed as
NHS nurses, one was working part-time as a carer in a
community support agency, and one was a staff nurse
in a private care home.
Data collection
The participants were invited to take part in an
autobiographical narrative interview. Each interview
was conducted in English, lasted for approximately 1.5
hours, and was audio-recorded with the participants’
consent. Three interviews were conducted at the participants’
homes, and two were conducted in a public
place suggested by the participants (coffee shop and
community centre). The remaining interviews were
conducted at the participants’ workplace, after they
had finished work.
At the start of each interview, the interviewer
described the aim of the study in detail, provided an
opportunity to ask further questions and obtained
written consent. The interviewer began by saying ‘I
would like to ask you to tell me the story of your
educational and professional life before and after you
came to the UK. A good way to do this would be to
start talking about your education and work experience
you gained in your home country, and then
about your education and work experience in the
UK until today. After that you can also tell me your
thoughts about your professional future.’ There were
also specific narrative questions regarding experiences
with UK institutions (‘Did you approach an employment
agency or job centre?’), psychosocial resources
(‘How are your relations with other compatriots?’) and individual coping (‘Do you think you are in
control of things in your life?’) and psychosocial
well-being (‘Are you satisfied with the way your life
is?’). After the interview each participant was asked to
complete a questionnaire to gather information about
their educational and professional history and demographic
data.
Table 1 :Demographic characteristics of participants
Analysis
Verbatim transcriptions of interview data were analysed
with the assistance of a qualitative data analysis software
program, NVivo version 8. Thematic network
analysis was used to organise the narrative interview
material and to interpret the participants’ emerging
subjective theories (Attride-Stirling, 2001). Thematic
analyses of qualitative data in general attempt to reveal
the themes that are salient in a text at different levels, and thematic networks in particular aim to facilitate
the structuring and depiction of these themes
(Attride-Stirling, 2001, p. 387).
The first step in a thematic network analysis is to
code the material. This was done by dissecting the text
into meaningful text segments related to three themes:
1 first work-related experiences in the UK
2 the psychosocial resources that the participants
said they used while facing various post-migration
challenges
3 psychosocial well-being.
Sections initially coded as psychosocial resources were
further coded according to CHCelements such as health
literacy, an enterprising disposition presupposing a
sense ofmastery and self-efficacy, an orientation toward
the future and its control through action, and adaptive
interactional styles. Once the text was coded, the
themes were abstracted by going through the text
segments in each code and by extracting the common or significant themes (Miles and Huberman, 1994).
Inter-judge reliability was attained by creating codes
and themes separately and then cross-checking the
codes and themes that each of the researchers had found.
Discrepancies were resolved through discussion and
re-examination of the data.
The emerging themes were assembled into groupings
based on content and theoretical grounds. These
groupings became the basic themes. Clusters of basic
themes centred on larger, shared issues from which
the organising themes were created. Finally, the main
claim to which the organising themes referred was
summarised and became a subjective theory, a term
that refers to the fact that each interviewee constructs a
complex stock of knowledge about the topic under
study. This knowledge includes assumptions that are
explicit and immediate and which the individual can
express spontaneously when answering an open question.
These are complemented by implicit assumptions,
which can be derived through more direct
questions (Flick, 2002, p. 80). Subjective theories do
not refer to objective stocks of knowledge that people
hold, but rather they are shaped by existing social
norms and cultural values and are influenced by
interactions with others. Individuals create meaning
from interactions, relating their existing beliefs to new
ideas and social situations (Schwandt, 1998).
In this study, the meanings that overseas doctors
and nurses attached to their experiences were constructed
through various interactions in different
social contexts in the UK.
Subjective theories can be contrasted with expert
theories through which scientists, researchers and
policy makers explain participants’ experiences. Expert
theories, such as the CHC framework, make
claims that attempt to describe an ‘objective’ socialpsychological
reality (Denzin and Lincoln, 1998). In
this paper we open a dialogue between what is objective,
expert knowledge and the subjective. Thus we
discuss overseas doctors’ and nurses’ subjective theories
of their professional experiences while exploring
how they use the attributes comprising CHC, when
constructing these theories.
Findings
Two thematic networks, consisting of basic and organising
themes, are presented. The basic and organising
themes are first discussed and relevant quotes are
integrated, to illustrate how these themes link together
into a subjective theory. After each quote the gender,
occupation and migration status of that interviewee
are noted in parentheses.
Basic themes
These were themes raised by all participants. The
generative narrative question prompted the participants
to talk about their educational and professional
experiences before and after migration. The issues of
accrediting one’s qualifications in the UK and being
recruited, and how these were influenced by migration
status, constituted the basic themes emerging from all
interviews.
The process of accrediting qualifications
and its dependence on migration status
Recognition of qualifications acquired depended
largely on participants’ migration status. This was
far from straightforward, especially for refugees. For
one refugee doctor who later acquired British citizenship,
the long delay in the accreditation process
affected his professional development:
Because I had no documents I was not eligible to update
my training or continue my training and follow registration.
So I was just waiting for my status to be clarified
by the Home Office. After two years, with the help of [X]
University, they sent my diplomas for recognition to the
British Council. Then the British Council doesn’t recognise
my qualification and they say that because of the
[time] gap.
(Male doctor, health officer in local authority,
refugee/British citizen)
The process was more straightforward for EU citizens:
I had my interview before I had my certificate of completion
of training and I emigrated [to the UK] very
quickly after receiving the certificate. So I worked in my
home country for about 6 years and then I came to theUK
and I have worked here for about 5 years as well.
(Female doctor, NHS psychiatrist, EU citizen)
Pace of recruitment based on migration
status
Fast and successful recruitment also depended on
migration status. Once again, the process was simpler
for those with a work permit than for those with a
more temporary status:
I sent in my application [in] July and then in October the
agency phoned me. ... I went for an interview and it is this
Trust, so I’m lucky I got the job. I came here in January
2001 so it’s very quick. It’s a straightforward process, after
the interview, in 3 months I came here.
(Female nurse, employed in the NHS, with work permit)
Interviewees with a temporary status faced a more
complex and slower recruitment process. Delays due
to migration status were compounded by time spent
out of the UK workforce:
I’m afraid if I can’t get back into the system, what shall I
do? It’s shocking, you know. Sometimes I think ‘I’ve been
out of job nearly two years, it is really bad’, although I can
qualify now for interview. But if I get a job in one year,
then there will be a gap, three years gap, and then more
difficult to get back into the system again.
(Male doctor, project officer in private healthcare agency, LLR)
Organising themes
The organising themes refer to the participants’ active
use of resources in order to progress professionally in
the UK. This active use of resources was selected as the
main principle linking the basic themes because it
showed what they claimed to do in order to overcome
difficulties. The resources presented here refer mainly
to aspects of CHC such as health literacy, sensitivity to
interpersonal dynamics and ability to adapt one’s
interactional styles, an enterprising disposition which
presupposes self-efficacy, orientation toward the future
and its control through action. We selected quotes in
which interviewees described what they did in order to
progress professionally, and where the above aspects
of CHC are captured.
Enhancing health literacy
Opportunities to undertake training and thus improve
one’s health literacy were positive experiences,
allowing the participants to progress professionally. In
the following example, an NHS nurse highlighted the
complexity of the training that she was required to
undertake. She acknowledged that it enhanced her
health literacy, and thus improved her chances of
career progression:
We have many skills from back home we can use here but
we are not allowed to ... until we do the training. So I’ve
done that and now I am able to do everything I was doing
back home, even mentor the students which is very good.
It’s very good, I have been always interested in learning
more and accepting the challenges, that’s why I’m trying
to do much training ... because everybody wants to go
higher up the bands and I love to improve as well.
(Female nurse, employed in NHS hospital, with work permit)
Sensitivity to interpersonal dynamics/
adaptability
The ability to adapt while interacting with others was
also noted when discussing professional advancement.
The next quote captures another relevant aspect
of CHC, namely sensitivity to interpersonal dynamics
and the ability to adapt one’s interactional styles. This
interviewee noted discriminatory attitudes at the
workplace, but also discussed how to bypass them:
You can hear most of the staff has been abused, not
physically but verbally, especially if you’re a foreigner,
although I haven’t experienced that or maybe I didn’t give
attention, but I’ve heard a lot about racism and it’s true
with colleagues, especially if they’re coloured. But so far
when I’m with the patients and the relatives we always
have good feedback ... they will say all your nurses are
good so that’s good because everywhere you go you find
nurses from mycountry ... it’s all right, I don’t regret being
here.
(Female nurse, employed in NHS rehabilitation
ward, with work permit)
The doctor in the following quote also raised the issue
of adjusting interactions. He narrated how he embraced
the interprofessional aspects in his first post
in the UK, later on experienced tension within the
workplace, and finally realised the sacrifices he had to
make:
I liked that I didn’t have to rush, I could see the patient and
talk with them. I liked the close interaction with teams,
not only medical but palliative care, psychology, counselling,
social care. I thought it was very holistic. So I just
clicked I could do this for the rest of my life and after that I
got this job. ... There is a problem that you need to be
prepared to work more than 12 hours a day ... if you say to
one of the bosses, this is out of hours, I’m not going to do
this, they see that as a sign of weakness. Colleagues will
think you’re not motivated. ... And I’ve come across that
competitiveness here a lot. I guess I need to make sacrifices
in my personal life ... now I’m more prepared to do [that].
(Male doctor, NHS oncologist, EU citizen)
Orientation towards the future and its
control through action
Some interviewees described their long-term professional
plan, thus indicating that progress could be
attained through another aspect of CHC and, in
particular, an orientation towards the future and its
control through action. In the following quote from a
doctor, professional progress was made possible by
being clearly future-oriented and taking (in her case)
radical actions towards achieving her goals:
In [my country’s] system it’s very hierarchical ... doctors
use the power with the patient. ... In the UK, it’s far more
equal and doctors have to consider the cultural background
and the patient’s belief system and share the
decision making. So the patient has to be part of the
process, and that’s why I embraced it once I landed. ... But
the regulatory bodies they’ve been really pushing on
doctors and there’s a lot of discontentment ... there’s a
trend in the UK psychiatry of people coming to a doctor
with what I call ‘life syndrome’ and expecting I prescribe a
happy pill and they’ll be happy ever after. I just disagree
with that ... it’s overwhelming and I ampreparing my exit
from the profession.
(Female doctor, NHS psychiatrist, EU citizen)
An enterprising disposition that
presupposes self-efficacy
Another element of CHC, an enterprising disposition
that presupposes self-efficacy, also emerged in some
narratives. The doctor in the next quote discusses the
different professional pathways that he took while
trying to attain his main professional goal:
When I was working for the pharmaceutical industry it
was very different ... that was not me ... because it was a lot
of commercial work and was too far away from what I was
doing not so long ago which was dealing with patients. I
just didn’t feel comfortable. So coming into theNHSwas a
personal decision. I wanted to get into the public sector
and see how it goes ... because pursuing international
development, that’s probably the ultimate career goal for
me, do a bit of consulting and then get into the international
development sector. I think the public sector
would offer more development opportunities than the
private sector. I don’t know if that’s true but that’s my
perception of it.
(Male doctor, NHS strategy manager, highly skilled migrant)
Subjective theories
Two subjective theories emerged from our interpretation
of the narrative material. Their differences were
not immediately evident, but the significant ones rest
on the psychosocial well-being outcomes that they
presented.
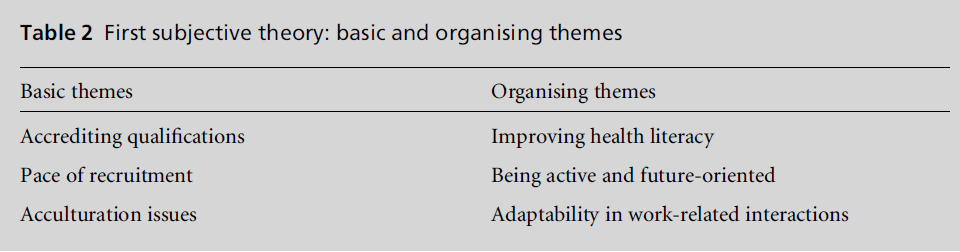
First subjective theory
Four nurse participants made sense of their professional
experiences in the UK through the first subjective
theory (see Table 2). They all discussed having
positive psychosocial well-being and reported using
various resources to cope with problems.
In this subjective theory, the basic themes referred
to accreditation of qualifications and recruitment, and
in particular how these depended on migration status.
Other issues, such as initial problems of acculturation, were also raised. With regard to the organising themes,
participants said they used several resources, such as
adapting their interactional styles at work and improving
health literacy. Finally, this theory contained a
positive psychosocial outlook, since this group presented
itself as resilient, optimistic about the future
and expressing overall satisfaction with their postmigration
life.
In the next quote, a nurse discussed the difficulties,
compounded by his temporary status, of acquiring a
permanent healthcare post. He confronted this issue
by cultivating two CHC elements, namely choosing to
actively strengthen his knowledge of psychiatry and
being future-oriented:
I amworking as a carer but it’s part-time, it’s not enough.
I also do voluntary work, because I am willing to increase
my knowledge of psychiatry. If I go to work in a factory or
something I’ll be missing all my education so I want to be
inside the medical field and then get full-time work. ... I’ll
get my goal, because I’m willing ... and patient. ... They
sent me a letter and said they are processing [the asylum
claim] so I can’t say when. ... Some people get into
depression. I know doctors [from my country] that
became mentally sick. Like me, they waited for a good
document [and did not get it]. But I continue with what I
do.
(Male nurse, carer in support agency, LLR)
Another participant, who experienced difficulties in
securing a post as a hospital nurse, provided another
example using a different CHC element. She adapted
her interactional style at work and eventually emerged
as resilient and satisfied in her post:
When I came here I told myself I am going to work in a
care home and then maybe go back into a hospital. After
two years I tried applying for the post. I went for interviews
four or five times and they would ask ‘Do you have
the adaptation course?’ I would say ‘No.’ ... And then also
when you’re working in a care home you know, you are
not a nurse. This is the thing I noticed and then it took me
time to say, you know what, you’re a foreigner and you are
not working as a nurse in a hospital, but I amhere and it’s
been fine.
Table 2:First subjective theory: basic and organising themes.
(Female nurse, working in private care home,
with work permit)
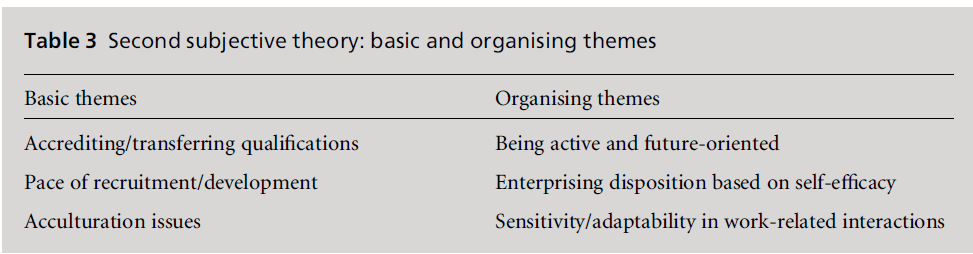
Second subjective theory
The remaining six participants (all five doctors and
one nurse) made sense of their professional experiences
in theUKby focusing on the difficulties that they
experienced as they were trying to enter the British
labour market, failed efforts to activate resources
and subsequent negative psychosocial well-being (see Table 3). They discussed accreditation, recruitment
and acculturation problems, inability to activate resources
to cope with these problems, and declining
psychosocial well-being.
In this subjective theory, the basic themes again
related to the issues of accreditation of qualifications
and recruitment, and how these depended on migration
status. The participants discussed the resources
that they attempted to activate in order to cope with
some of their difficulties, and how they still failed to
attain the state they were aiming for. With regard to
psychosocial well-being these interviewees presented
themselves as lacking the confidence to overcome
difficulties, and being dissatisfied with their professional
lives in the UK.
In these participants’ accounts there is a sense of
failure to use CHC, despite making concerted efforts
to do so. For example, one of the doctorsmade reference
to two CHC elements while describing how he tried
to cope with his problems. These elements were an
orientation towards the future and its control through
action, as he kept applying for different jobs that
matched his qualifications, and a clear sensitivity to
interpersonal dynamics, as he did not want to insult
his friends who had lower skills. However, he expressed
shame about his current professional stagnation and
anxiety about his future. He revealed his hurt pride
and his subsequent depression because, despite his
credentials and continual efforts, he could not find a
medical post in the NHS:
Then I was applying for jobs here and there, one position
with Oxfam, monitoring evaluation, that’s my specialisation,
and also with a PCT in London, a position of Public
Health Information Officer there. With Oxfam, I didn’t
even get an interview. With the PCT I got one interview,
but I didn’t do well, my English or my presentation skills
were still not good ... then friends told me ‘Why don’t you
work in the supermarket?’ I was controlling myself not
to say anything. ... They are graduates but not in any profession, so they don’t understand how we build up our
professional pride. ... Even if I’m not qualified here as a
medical doctor, still as a public health professional, I am
qualified to work somewhere and I am still getting
interviews. ... But it’s quite depressing, I feel this is quite
difficult.
(Male doctor, project officer in private
healthcare agency, LLR)
Another doctor also felt ashamed of his professional
exclusion. Despite his efforts to cultivate the CHC
element of adaptability, he was not given the opportunity
to convey his skills as a medical doctor in the
UK:
I am capable of work in my profession. In my home
country I was working as a head of the hospital, but I don’t
want to be head of the hospital here in London because ...
they won’t give it to us. Because of the age, the race, the
status, because there is no racial equality. So we don’t
expect these things, but this diploma I have, [I] put it in a
pharmacy department, [to] see if I was capable of work, if
not, fine. But they didn’t give us a chance, they should use
us in a positive way to help ourselves and to help this
country. ... So it’s a shame for us, a shame for the profession
and [a] shame for all those people who see us like
that.
(Male doctor, health officer in local authority,
refugee/British citizen)
Finally, a doctor employed in the NHS discussed his
frustration at not being able to advance his career in
his current post because, despite his enterprising disposition,
his contribution remained unacknowledged
due to differential treatment:
The other thing this organisation doesn’t do well is talent
management. Clearly I’ve managed quite a few things and
I’ve actually done well on the change management programmes
... every time they need somebody I’m always
approached. But when I try to make that as a permanent
career I’m always told there isn’t a permanent need so that
pushes me back ... because I’m from that country and
we’re classified in that bracket it’s a much tougher road
than people from the EU ... and the biggest frustration I
have doing this role is it’s still not considered a strategic
priority, and ... it doesn’t help at all in terms of confidence
building.
Table 3:Second subjective theory: basic and organising themes.
(Male doctor, NHS strategy manager,
highly skilled migrant)
Discussion
Our study is limited by its small sample and the
participants’ diverse backgrounds. We therefore need
to be cautious when drawing conclusions about the
professional experiences of overseas doctors and nurses
in the UK. Also, although we attained inter-judge
reliability, the participants did not validate our interpretations,
mainly because of the difficulties of researching
mobile populations, such as migrants and refugees,
who may be unable to meet the researcher more than
once. Despite these limitations, our findings add indepth
knowledge to an expanding body of research
related to health workforce development and highly
skilled migration, and offer an alternative way to
conceptualise professional experiences and career development.
Our findings show the crucial role of migration
status in overseas nurses’ and doctors’ professional
progression in the UK. Participants with a temporary
migration status experienced barriers and delays as
they tried to develop professionally,whereas thosewith a
more permanent status progressed more quickly. The
finding that migration status largely shapes foreignborn
professionals’ participation in the labour market
confirms the results of previous research (Bloch,
2004).
There was an obvious divergence between doctors
and nurses in terms of professional development and
psychosocial well-being. Doctors appeared to be more
negative about their professional prospects, despite
the fact that some of them had succeeded in initiating
a career in the UK healthcare sector. They expressed
dissatisfaction with their life in the UK. Two doctors
reported that they often felt depressed and two others,
one of whom was preparing to leave the UK, were
deeply disappointed with their experience. In contrast,
despite initial difficulties and slow professional
development, nurses emerged as more psychosocially
adjusted and satisfied with life in the UK. Only one
nurse appeared psychosocially vulnerable, and this
was due to specific family circumstances. This difference
between the two professional groups could perhaps
be attributed to psychosocial factors such as
perceived and experienced discrimination. However,
these factors have been identified in relation to both
doctors (Esmail, 2007) and nurses (Larsen, 2007), so
they could not explain the differences in well-being
between the two groups.
Structural factors could offer another explanation
(Hugman, 1991). The historical dominance of medicine
restrained other professions such as nursing from
asserting its professional identity and seeking equal
treatment to doctors. According to this analysis,
nurses were often perceived as semi-professional and
‘tended to ‘‘silence’’ themselves in order to maintain the culture of the workplace’ (Roberts, 2000, p. 74).
The nurses in our sample could have been sharing this
traditional view of their profession, an attitude that
was possibly reinforced in the developing countries.
Perhaps their expectations about their career progression
were lower than those of doctors, who regarded
themselves as having ‘a strong and unchallenged position
in medical work’ (Svennson, 1996). However, it
is still unclear why doctors emerged as psychosocially
vulnerable.
Alternatively, doctors’ low well-being could be
attributed to their inability to use CHC effectively.
The ‘deeply relational’ (Shim, 2010, p. 4) aspect of
their CHC was affected by work relationships and
environment restrictions. The narratives of doctors
who were EU citizens and worked in the NHS suggested
that they felt constrained by what they saw as
distorted doctor–patient interactions (in which patients
requested ‘happy pills’), working conditions in which
overtime was expected, and competitive relationships
with colleagues. These observations support previous
findings that overseas-trained doctors are constantly
more supervised than UK-trained doctors because
they are not trusted to use their discretion and have
low morale (Oikelome and Healy, 2007). It is highly
possible that interactional difficulties, compounded
by increased regulation of the medical profession
(Case, 2011), lead doctors to feel frustrated and disappointed.
Such observations echo Foucault’s thesis
that ‘power is everywhere’, diffused and embodied in
discourse, knowledge and ‘regimes of truth’ such as
the highly regulated English medical environment
(Foucault, 1994, p. 194). Foucault points to a kind
of ‘disciplinary power’ that can be observed in the
administrative systems and welfare services. Their
systems of surveillance and assessment no longer
require force or violence, as people learn to discipline
themselves and behave in the ways that are expected.
Our analysis demonstrates that the theoretical
framework of CHC is a useful tool for considering
the relationship of professional development and
psychosocial well-being in participants’ narratives,
and for exposing structural and institutional barriers
to career aspirations compounded by social inequalities
faced by immigrant groups. As our examples
suggest, CHC functions when overseas professionals
can communicate cultural skills and attributes in ways
that are recognisable and usable in the healthcare
systems.
Conclusion
Overseas healthcare professionals are a significant group
of workers in the UK. Although they represent a great
opportunity for diversification and multiculturalism of healthcare provision, their multifaceted professional
experiences and needs cannot be fully understood
by applying existing theories of acculturation
and cultural capital. Instead, an integrative, more
specific approach, such as CHC, is needed. Our analysis
supports an integration of macro- and microperspectives
(Larsen et al, 2005). Having established
the usefulness and applicability of the CHC framework,
we conclude with some recommendations for
improving the professional experiences of overseas
doctors and nurses.
The work-related experiences of highly skilled workforces
such as healthcare professionals are more favourable
than those of unskilled workforces because of their
qualifications and bargaining power (Wickramasekara,
2002, p. 3). This distinction should not divert attention
from the vulnerability of overseas professionals
who are trying to integrate into the healthcare sector
(Bach, 2003). Our findings highlight the importance
of removing barriers which obstruct their entry into
the workforce and hamper their career progression.
This will benefit not only individual professionals but
also communities that require a diverse workforce to
meet local healthcare needs. In the current UK context,
migration is not only greater in terms of numbers
in comparison with previous decades, but is also more
diverse. This diversification of migrant populations is
beginning to have an impact on what diversity means
and how to take advantage of it (Kyambi, 2007).
Policies that encourage highly skilled migrants’ socioeconomic
inclusion are needed now as never before.
It is also necessary to attend to the professional
advancement of overseas doctors and nurses who are
fully employed. Maintaining one’s professional identity
is important for highly skilled migrants in modern
western societies (Liversage, 2009). Continuing professional
development is crucial for their well-being
(Dawson et al, 2009). This is especially the case for staff
working in the NHS, where changes in terms of
managerial processes can produce shifts in the balance
of power between healthcare staff and managers, with
the locus of control having clearly shifted towards the
latter (Sheaff, 2008, p. 16). Maintaining sensitivity to
interpersonal dynamics is crucial in both clinical and
interprofessional encounters. Attending to this will
again benefit not only individual doctors and nurses
but also the organisations and the communities that
they serve. Further research drawing on CHC theory
and utilising larger, more ethnically diverse samples of
overseas healthcare professionals is required to provide
a deeper understanding of how to use these
populations’ potential for the delivery of healthcare
in the best possible way.
Acknowledgements
We wish to thank all of the participants in the study..
The project was funded by a small grant from the
South West Academic Network (SWAN) Interprofessional
Institute, awarded to EH in July 2009.
CONFLICTS OF INTEREST
None.
References
- Alexis O, Vydelinqum V and Robbins I (2007) Engaging with a new reality: experiences of overseas minority ethnic nurses in the NHS. Journal of Clinical Nursing 16:2221’8.
- Attride-Stirling J (2001) Thematic networks: an analytic tool for qualitative research. Qualitative Research 1:385’405.
- Bach S (2003) International Migration of Health Workers: labour and social issues. Working Paper 209. Geneva: International Labour Office.
- Batnitzky A and McDowell L (2011) Migration, nursing, institutional discrimination and emotional/affective labour: ethnicity and labour stratification in the UK National Health Service. Social and Cultural Geography 12:181’201.
- Batnitzky A and McDowell L (2013) The emergence of an ‘ethnic economy’? The spatial relationships of migrant workers in London’s health and hospitality sectors. Ethnic and Racial Studies 36:1997’2015.
- Berry JW (1997) Immigration, acculturation and adaptation. Applied Psychology 46:5’34.
- Bloch A (2004) Labour market participation and conditions of employment: a comparison of minority ethnic groups and refugees in Britain. Sociological Research Online 9(2). www.socresonline.org.uk/9/2/bloch.html (accessed 4 February 2012).
- Bourdieu P (1986) Distinction: a social critique of the judgement of taste (trans. R Nice). London: Routledge and Kegan Paul. Bourdieu P (2001) Forms of capital. In: Granovetter M and Swedberg R (eds) The Sociology of Economic Life, 2nd edn. Boulder, CO: Westview. pp. 96’111.
- Butler C and Eversley J (2009) Refugee Healthcare Professionals’ Survey. Final report for the Refugee Healthcare Professionals Programme: NHS employers. London: PPRE Limited.
- Case P (2011) Putting public confidence first: doctors, precautionary suspension, and the General Medical Council. Medical Law Review 19:339’71.
- Clark P, Stewart JB and Clark DA (2006) The globalization of the labour market for health-care professionals. International Labour Review 145:37’64.
- Cohn S, Alenya J, Murray K et al (2006) Experiences and expectations of refugee doctors. British Journal of Psychiatry 189:74’8.
- DavidNand ChertiM(2006) Losing Out Twice? Skill wastage of overseas health professionals in the UK, London: Migrant and Refugee Communities Forum.
- Dawson J, Chu C, KaurMet al (2009) Health and Well-Being of NHS Staff: a benefit evaluation model. London: The Work Foundation.
- Denzin NK and Lincoln YS (eds) (1998) The Landscape of Qualitative Research: theories and issues. Thousand Oaks, CA: Sage
- Esmail A (2007) Asian doctors in the NHS: service and betrayal. British Journal of General Practice 57:827’31.
- Flick U (2002) An Introduction to Qualitative Research. London: Sage.
- Flyvbjerg B (2001) Making Social Science Matter: why social inquiry fails and how it can succeed again. Cambridge: Cambridge University Press.
- Foucault M (1994) Discipline and Punishment. New York: Vintage Books.
- Garcı´a-Ramı´rez M, De la Mata M, Paloma V et al (2010) A liberation psychology approach to acculturative integration of migrant populations. American Journal of Community Psychology 47:86’97.
- General Medical Council (2011) The State of Medical Education and Practice in the UK. London: General Medical Council.
- Henry L (2007) Institutionalized disadvantage: older Ghanaian nurses’ and midwives’ reflections on career progression and stagnation in the NHS. Journal of Clinical Nursing 16:2196’203.
- Heron J and Reason P (2001) The practice of co-operative inquiry: research with rather than on people. In: Reason P and Bradbury H (eds) Handbook of Action Research: participative inquiry and practice. London: Sage. pp. 179’ 88.
- Hugman R (1991) Power in Caring Professions. Basingstoke: Macmillan. Jones A, Bifulco A and Gabe J (2009) Caribbean nurses migrating to the UK: a gender-focused literature review. International Nursing Review 56:285’90.
- Kyambi S (2007) Migrants and social inclusion: what would a progressive approach look like? In: Flynn D and Williams Z (eds) Towards a Progressive Immigration Policy. London: Compass. pp. 32’4.
- LamontM(2002) The Dignity of Working Men: morality and the boundaries of race, class and immigration. Cambridge, MA: Harvard University Press.
- Lamont M. (2010) Looking back at Bourdieu. In: Silva E and Warde A (eds) Cultural Analysis and Bourdieu’s Legacy: settling accounts and developing alternatives. London: Routledge. pp. 128’41.
- Lareau A (2003) Unequal Childhoods: class, race and family life. Berkeley, CA: University of California Press.
- Larsen JA (2007) Embodiment of discrimination and overseas nurses’ career progression. Journal of Clinical Nursing 16:2187’95.
- Larsen JA, Allan HT, Bryan K et al (2005) Overseas nurses’ motivations for working in the UK: globalization and life politics. Work, Employment and Society 19:349’68.
- Liversage A (2009) Vital conjunctures, shifting horizons: high-skilled female immigrants looking for work. Work, Employment and Society 23:120’41.
- Loury GC (2002) The Anatomy of Racial Inequality. Cambridge, MA: Harvard University Press.
- Marmot M (2010) Strategic Review of Health Inequalities in England Post-2010. The Marmot Review final report: fair society, healthy lives. London: University College London.
- Miles MB and Huberman AM (1994) Qualitative Data Analysis. Thousand Oaks, CA: Sage.
- Montreuil A and Bourhis RY (2001) Majority acculturation orientations toward “valued’’ and “devalued’’ immigrants. Journal of Cross-Cultural Psychology 32:698’719.
- Oikelome F and Healy G (2007) Second-class doctors? The impact of a professional career structure on the employment conditions of overseas- and UK-qualified doctors. Human Resource Management Journal 17:134’54.
- Pang T, Lansang MA and Haines A (2002) Brain drain and health professionals. British Medical Journal 324:499’500.
- Phillimore J (2010) Approaches to health provision in the age of super-diversity: accessing theNHSin Britain’s most diverse city. Critical Social Policy 31:5’29.
- Psoinos M (2007) Exploring highly educated refugees’ potential as knowledge workers in contemporary Britain. Equal Opportunities International 26:834’52.
- Ratzan SC and ParkerRM(2000) Introduction. In: Selden C, Zorn M, Ratzan S et al (eds) National Library of Medicine Current Bibliographies in Medicine: health literacy. Bethesda, MD: National Institute of Health. pp. v’vii.
- Rechel B, Dubois C-A and McKeeM(eds) (2006) The Health Care Workforce in Europe: learning from experience. Brussels: European Observatory on Health Systems and Policies, WHO European Centre for Health Policy.
- Roberts S (2000) Development of a positive professional identity: liberating oneself from the oppressor within. Advances in Nursing Science 22:71’82.
- Royal College of Nursing (2007) Here to Stay? International nurses in the UK. London: Royal College of Nursing.
- Rudmin FW (2003) Critical history of the acculturation psychology of assimilation, separation, integration and marginalization. Review of General Psychology 7:3’37.
- Schwandt TA (1998) Constructivist, interpretivist approaches to human inquiry. In: Denzin NK and Lincoln YS (eds) The Landscape of Qualitative Research: theories and issues. Thousand Oaks, CA: Sage. pp. 221’59.
- Sheaff R (2008) Medicine and management in English primary care: a shifting balance of power? In: McKee L, Ferlie E and Hyde P (eds) Organising and Reorganizing: power and change in healthcare organizations. Basingstoke: Palgrave Macmillan. pp. 1’18.
- Shim JK (2010) Cultural health capital: a theoretical approach to understanding healthcare interactions and the dynamics of unequal treatment. Journal of Health and Social Behavior 51:1’15.
- Sinclair J, LatifiAHand LatifiAW(2006) Refugee doctors as doctors’ assistants in psychiatry. The Psychiatrist 30:430’ 31.
- Smith PA, Allan H, Henry LW et al (2006) Valuing and Recognizing the Talents of a Diverse Healthcare Workforce. Report from the REOH Study: researching equal opportunities for overseas-trained nurses and other healthcare professionals. London: Royal College of Nursing, and Guildford: University of Surrey. www.rcn.org.uk/__ data/assets/pdf_file/0008/78713/003078.pdf
- Stephenson N and Papadopoulos D (2006) Analysing Everyday Experience: social research and political change. Basingstoke: Palgrave Macmillan.
- Stewart E (2003) A Bitter Pill to Swallow: obstacles facing refugee and overseas doctors in the UK. New Issues in Refugee Research. Working Paper No. 96. Geneva: UNHCR Evaluation and Policy Analysis Unit.
- Svensson R (1996) The interplay between doctors and nurses—a negotiated order perspective. Sociology of Health & Illness 18:379’98.
- Cultural health capital and experiences of overseas healthcare professionals 47 Troy PH, Wyness LA and McAuliffe E (2007) Nurses’ experiences of recruitment and migration from developing countries: a phenomenological approach. Human Resources for Health 5: 15.
- Ward C (1996) Acculturation. In: Landis D and Bhagat RS (eds) Handbook of Intercultural Training, 2nd edn. Thousand Oaks, CA: Sage. pp. 124’47.
- Wickramasekara P (2002) Asian Labour Migration: issues and challenges in an era of globalization. International Migration Papers 57. Geneva: International Labour Office. www.ilo.org/asia/whatwedo/publications/WCMS_ 160632/lang’en/index.htm