Keywords
Australia, culture, cultural racism, ethnic
minorities, healthcare, language prejudice, patient
safety
Introduction
The purpose of this article is to explore the idea that
racial and ethnic disparities in patient safety and quality
care may be substantively expressive of unrecognised
and unacknowledged cultural racism in healthcare
contexts (see Box 1). The research data considered
in this article contribute to further understanding the
often disguised and sophisticated ways in which cultural
racism may work in a healthcare environment.
To this end, attention is given to describing the specific
phenomenon of language prejudice and discrimination
as a form of cultural racism that was discovered
serendipitously in the context of a broader study
exploring cultural safety and cultural competency in an
Australian healthcare context (Johnstone and Kanitsaki,
2007a,b). A key conclusion drawn from this study is
that the failure to name and distinguish language prejudice
and discrimination as a form of racist practice in
hospital contexts, and the tendency to portray language
prejudice as merely a communication issue, risks at
least two undesirable outcomes. First, it risks seriously
undermining progressive policy and practice initiatives
aimed at genuinely improving the capacity of hospitals
and individual healthcare providers to respond appropriately
and effectively to the health and care needs
of people from minority cultural and language backgrounds.
Second, it risks the loss of an important
opportunity to identify and eliminate racial and ethnic
disparities in patient safety and quality care that until
now have been poorly investigated.
Background to the study
The failure to provide culturally and linguistically
appropriate healthcare has been substantively implicated
in racial and ethnic disparities in health (Smedley
et al, 2003). More recently, the failure to provide
culturally and linguistically appropriate healthcare
has also been implicated in disparities in patient safety
and quality care, with recent research suggesting that
patients of a non-English-speaking background (NESB)
maybe at disproportionate risk, compared to the average
population, of experiencing preventable adverse events,
including permanent disability and even death (Flores
2005; Johnstone and Kanitsaki, 2006; Schnittker and
Liang, 2006; Divi et al, 2007).
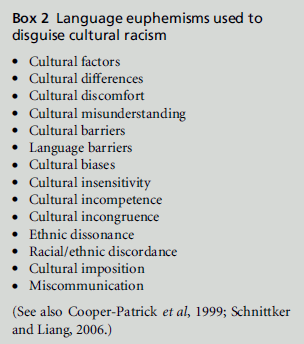
Significantly, the language most commonly used to
interpret and explain racial and ethnic disparities in
health, patient safety and quality care reflects a focus
on and valuation of cultural factors (see Box 2).
Discourses on possible solutions to recognised disparities
in ethnic health, in turn, tend to be framed by
language that refers to various pragmatic processes
such as ‘valuing cultural diversity’, promoting cultural
competency, and adopting the principles and standards
of culturally and linguistically appropriate services,
which is sometimes referred to using the acronym
‘CLAS’ in healthcare (Johnstone and Kanitsaki,
2007a,b). The use of such language and related discourse
is, however, problematic because of its capacity
to disguise cultural racism (Johnstone and Kanitsaki,
2008).
Box 2:Language euphemisms used to
disguise cultural racism.
Cultural racism is a process whereby people who are
strongly identified with certain ‘language groups,
religion, group habits, norms and customs, including
typical style of dress, behaviour, cuisine, music and
literature, are treated in a prejudicial and discriminatory
way based on these characteristics (Goldberg,
1993, p.70). Although racism is being increasingly
named by researchers as a possible cause of persistent
health differences by racial or ethnic classifications in
Canada, the US,UK, Europe, and more recently Australia
(Smedley et al, 2003; Roberts, 2006; Schnittker and
Liang, 2006; Larson et al, 2007), the possible impact of
cultural racism as a determinant and predictor of the
hospital safety and quality care of NESB patients is
under-investigated (Johnstone and Kanitsaki, 2006;
Divi et al, 2007). Moreover, the link between cultural
racism and disparities in health is one that is highly
disputed and contested in some fields (seeWolf, 2006).
A troubling consequence is a tendency by health researchers
and scholars to shy away from explicitly
using the term cultural racism in their professional
discourses on racial and ethnic disparities in healthand
hospital safety and relying instead on less contentious
terms to account for adverse events (see Box 2).
The failure to name cultural racism as a determinant
and predictor of patient safety and quality care
risks a number of undesirable outcomes. Of particular
concern is the risk it entails of perpetuating what we
have described elsewhere as ‘the illusion of non-racism
in healthcare’ (Johnstone and Kanitsaki, 2008, p.178),
an illusion that rests on the frequently articulated belief
that racism is no longer an issue (afterMiles and Brown,
2003, p.11). The denial of racism seriously undermines
attempts to introduce more progressive policy and
practice initiatives aimed at improving the capacity of
hospitals and individual healthcare providers to respond
appropriately and effectively to the needs of
NESB people in hospital contexts. It also risks impeding
an important opportunity to identify and eliminate
ethnic disparities in patient safety and quality care. In
contrast, naming cultural racism as a health justice
issue provides an interpretive framework to explainthe
disparities discerned (Bhopal, 2006; Roberts, 2006).
It is acknowledged that education, employment and
other socio-economic factors have been substantially
implicated in racial, ethnic health and social care
disparities.However, socio-economic indicators alone
do not always explain all of the differences noted,
notwithstanding that lower levels of education and
employment among different ethnic groups may, in
themselves, be indicators of past and current discriminatory
social policies and practices (Daniels, 2006;
Powers and Faden, 2006; Larson et al, 2007). It is also
noteworthy that the disparate care and treatment of
NESB people is remarkably consistent ‘across a range
of illnesses and healthcare services’ (Smedley et al,
2003, p.5). Nonetheless an important consideration
remains: although racial and ethnic disparities in health
have been convincingly demonstrated, and ethnic disparities
in patient safety and quality care have been
strongly suggested, it doesn’t follow that these disparities
are necessarily the consequences of racism. That
these disparities are expressive of racism thus needs to
be shown. While certain practices may well be expressive
of racism, ‘this must always be demonstrated
rather than assumed to be the case’ (Miles 1989, p.84).
It is an important aim of this paper to offer such a
demonstration.
Cultural context of the study
This study was conducted in the cultural context of
Australia. Australia is recognised as one of the most multicultural and multilingual countries in the world.
According to the 2006 Census of Population and
Housing, Australians, 22% of whom were born overseas,
claim more than 250 ancestries, speak over 400
different languages at home, and observe over 116 different
religions (Australian Bureau of Statistics, 2006).
Although themajority originates fromEnglish-speaking
countries and is English speaking, a significant minority,
over 19%, does not speak English at home and may
have difficulty communicating in English outside of
the home context, for example in workplace and mainstream
healthcare contexts (Allotey et al, 2002).
The cultural and linguistic diversity of Australia’s
population has significant implications for the country’s
healthcare services and for those at the forefront of
providing direct care to its multicultural and multilingual
population. It is known, for example, that the
emergency presentation and hospital admission rates
for people of culturally and linguistically diverse backgrounds,
especially those whose first language is not
English, in select metropolitan health services in
Australia is often close to and in excess of 50% (i.e.
one in every two), with an average of between 32% and
44% (i.e. one in every three or four) of all emergency
presentation and hospital admission rates per annum
(Centre for Culture, Ethnicity and Health, 2003).
Research problem
The terms used to explain ethnic disparities in health,
patient safety and quality care may be indicative of a
form of cultural racism – notably language prejudice
(see Box 2). The nature of language prejudice and its
possible implications for patient safety and quality
care outcomes in Australian hospital contexts has not
been systematically explored or described, and hence
is not known.
The research questions informing the component of
the study reported here were:
• Are people whose first language is not English the
subject of prejudice and discrimination in hospital
contexts because of their ‘language difference’?
• How is language prejudice demonstrated in hospital
contexts?
• What are the possible implications of language
prejudice for patient safety and quality care, and
related outcomes?
Study design and methods
Method
The original study on which this report is based was
undertaken as a naturalistic inquiry using the data
collection and analysis strategies commonly used in
qualitative exploratory descriptive (QED) research
(Patton, 2002). A QED approach was selected for the
purposes of this study since it is eminently suited to
facilitating the rich description, comparison, classification
and conceptualisation of new knowledge from
previously disorganised and/or non-related data
(Patton, 2002). It is also a highly pragmatic approach
that enables ‘quite concrete and practical questions’ to
be addressed by people who are ‘working to make the
world a better place (and wondering if what they are
doing is working)’ (Patton, 2002, pp.135–6). Moreover,
unlike other qualitativemethods such as grounded
theory and critical ethnography:
There is no mandate to produce anything other than a
descriptive summary of an event, organised in a way that
best contains the data collected and that will be most
relevant to the audience for whom it was written
(Sandelowski 2000, p.339).
Accordingly, the primary purpose of a QED approach
is fundamentally to describe rather than explain, and
thereby to permit ‘an understanding of the empirical
foundations of theory’ (Hamel, 1993, p.34). To this
end, the descriptive study does not ‘go against the
grain of theoretical sociological models; it permits
them to exist under more propitious conditions’
(Hamel, 1993, p.34).
Participants
Prior to the commencement of the project, institutional
ethics committee approval was obtained
from RMIT University and participating health services
who subsequently advised their staff of the
opportunity to participate in the project. Prospective
participants, who contacted the researchers upon
learning about the study,were given a letter explaining
the nature and purpose of the study and were formally
asked for their consent before taking part. Participants
were assured that confidentiality and anonymity
would be maintained by the use of numerical codes
on all transcripts of interviews and by the removal of
any identifying information from reports of the study.
One-hundred and forty-five participants were recruited
from over 17 different healthcare organisational and
domestic home sites. They represented staff and patients
from over 27 self-identified different ethnocultural
and language backgrounds.
Data collection
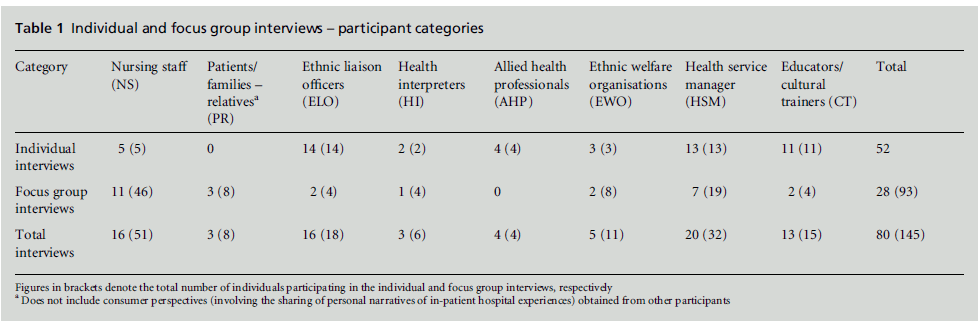
Data were collected via 52 individual interviews and
28 focus group interviews, as per the eight categories
depicted in Table 1. Interviews were conducted by the
authors, and were semi-structured and guided by the
use of open-ended questions that sought to explore
what the participants knew and understood about
cultural competency and cultural safety in healthcare;
the possible relationship between cultural competency,
cultural safety, and patient outcomes; and the processes
best suited to promoting cultural competency
and cultural safety in healthcare. Participants were
also invited to describe their best and worst experiences
when working with or caring for people from
diverse cultural and language backgrounds in an
Australian healthcare context. The length of each
interview ranged from 45 to 90 minutes.
Data analysis
Data were analysed independently by the two researchers
leading the study. The specific steps followed
included: producing a verbatim transcription of all
audiotaped interviews and organising these under each
of the categories of participants interviewed (see Table 1).
Then, for each category of participants interviewed,
summaries of the researchers’ respective field notes
and memos were drafted; transcript data and summaries
were read and interrogated and annotations
made in the margins of the transcripts and summaries;
tables and matrices were developed, categories created
and coded, and comparisonsmade. The two researchers
discussed the categories created and agreed to the
themes that had been identified. Quotations were
selected and agreed to on the basis that they were
representative of the consensual views that had been
captured. All material was then sorted into further
categories, with variables and relationships between
the categories pertinent to each of the groups interviewed
noted. Finally the analytic framework and
findings of the study were related to the literature
(Patton, 2002).
Research rigour and validity
In order to ensure the rigour of the study, due
attention was given to upholding the following principles:
credibility, fittingness, auditability, confirmability,
and triangulation (notably, source and analyst
triangulation; Patton, 2002). The application of these
principles, in this study, was described, in full, in
companion articles reporting the original research
(Johnstone and Kanitsaki, 2007a,b).
Table 1: Individual and focus group interviews – participant categories.
Presentation of the findings
Three key findings that emerged following analysis of
the data were:
• individual prejudice: patients and healthcare staff,
especially nurses and interpreters, who were born
overseas, and who spoke accented English as a second
language, or who could not speak English proficiently,
were especially vulnerable to being treated
in a prejudicial and discriminatory way by others
• internalised prejudice: negative attitudes experienced
by people whose first language was not English
were sometimes minimised, explained and justified
as being ‘not racism’ – even though their experience
left them feeling upset
• institutional prejudice: negative attitudes toward
people who either did not speak English as a first
language or did not speak it at all were embedded in
the system as demonstrated by such things as a lack
of infrastructure to support language services, a
lack of resources, and a lack of hard data defending
the need for resources that, paradoxically, were
difficult to obtain because of a lack of resources and
infrastructure.
Individual language prejudice
Patients and families
In the case of patients and their families, ‘othered’
language usage in hospital contexts was commonly
viewed as a ‘problem’ that was ‘caused’ by the inability
of patients to speak English rather than the inability of
health service providers to meet the patients’ communication
needs. As one nurse reflected:
‘Definitely communication is a big issue when you come
across people who do not speak a great deal of English ...
Somebody that doesn’t have a language problem can
freely express whatever it is that is on their mind. Whereas
a person like that who doesn’t speak English, they are not
less intelligent, they are not less capable, it is just this
language barrier.’ (NS09:2, 5)
A lack of access to qualified health interpreters meant
that patients who did not speak English proficiently
often relied on English-speaking family members to
assist them to communicate with hospital staff and, in
particular, to help ask the right questions. In some
instances, staff who were committed to ensuring that
their patients’ communication needs were met encountered
significant resistance when trying to obtain
the services of an accredited health interpreter:
‘I’m not supported and still, to this day, I feel a little bit of
trepidation that I’m going to have to fight a battle to get an
interpreter ... Whenever I have approached the topic of an
interpreter, cost is immediately brought up ... ‘‘Oh no, it’s
far too expensive to get an interpreter’’.’ (NS16:7–8, 9, 21–22) Some participants went on to suggest that NESB
patients were sometimes deemed by staff to be behaving
‘inappropriately’ when requesting assistance:
‘The nurses have a lot of difficulty understanding what
patients who don’t speak English want and they think
they’re demanding – that they become ‘‘demanding’’ and
do all this ‘‘inappropriate’’ behaviour. The nurses feel it’s
inappropriate behaviour to get their attention when, in
fact, if they could only understand what the patients are
trying to say, then a lot of the problems could be avoided.’
(PR02:R1:18–19)
Moreover, ‘how well’ patients and their family members
spoke English, and whether they spoke English
at all, had a significant influence on how they were
treated by attending staff. Numerous examples were
given of NESB patients and families often being judged
to be communicatively incompetent and even as not
speaking English at all when in fact they did. As one
registered nurse observed:
‘On a few occasions, because the patient has a strong
accent or doesn’t have perfect English, it has been written
on the care plan that the patient ‘‘doesn’t speak English’’.
It happened with one of my patients. I looked after that
patient and there were no problems whatsoever communicating
– maybe in a broken language, maybe with a
strong accent, but there was nothing wrong with her
English. Why did they put down that the patient didn’t
speak English? Because the staff had difficulty understanding
the accent.’ (NS09:6–7)
Patients who had been deemed communicatively incompetent
were also sometimes deemed to be rationally
incompetent (i.e. ‘stupid’). As one registered nurse
reflected:
‘Some staff think they are stupid, I can tell. Sometimes
they say, ‘‘They don’t understand what I say’’. Actually,
no, they do understand ... Some people who do not speak
English very well, it doesn’t mean they cannot think.
Sometimes they can think very well. It’s just they’re not
used to English or especially the medical terminology.’
(NS14:23)
Health interpreters reported that when staff thought
patients did not understand English, they sometimes
responded by treating them in a rude and abusive
manner, that in turn intimated and disempowered
such patients:
‘Sometimes the attitude of the reception staff is so cool –
they are extremely abrasive, they are extremely rude. They
yell at the patients if they don’t understand ... they speak
louder, so the patient gets intimidated. The patients are
often intimidated. Often the abrasive behaviour of the
professionals puts them in their place.’ (HI01:11)
The abrasiveness of staff was observed as particularly
acute in situations where they believed strongly that
patients who did not speak English were being ‘overly
advantaged’ and in ways that discriminated against English-speaking patients. According to one senior
health interpreter:
‘Sometimes the staff will make comments like, ‘‘You’re
getting free service, you should be grateful’’, which puts
the patients in their place straight away.’ (HI01:11)
In one instance, nursing staff were observed directly by
other staff to interfere with outpatient appointment
processes, which they perceived unfairly advantaged
non-English speaking patients over English-speaking
patients. In some cases staff were so concerned that
NESB individuals would get ‘preferential treatment’
that they would delay their appointments and ‘deliberately
put their file on the bottom of the pile’ (HI01:8),
thereby ensuring they would remain at the end of the
queue. In one case, when a health interpreter informed
staff in an outpatients’ clinic that he could no longer
wait because the time for which he had been booked
had expired and he had another patient booked in an
adjacent clinic, the receptionist responded, ‘But the
patient hasn’t been seen’. When he explained, ‘Well,
I’m terribly sorry, but my time has expired, I have to
go’, he was told, ‘Well, that’s on your conscience then’
(HI01:19).
It was acknowledged that patients who were dissatisfied
with the quality of their care could make a
formal complaint to the health service concerned.
Respondents noted, however, that people who did
not speak English tended to be reluctant to make a
complaint because of fearing repercussions and that:
‘If we complain we won’t get any more services.’
(ELO12:10)
Staff and co-workers
As in the case of patients, ‘how well’ staff members
spoke English also had a significant influence on how
they were treated by co-workers and their managers.
Nurses who spoke with accented English as a second
language were particularly vulnerable to being characterised
as communicatively incompetent and marginalised
by co-workers. One nurse participant recounted:
‘I have some personal experiences withmyaccent ... When
I get a little bit nervous, you have to say my language isn’t
that ‘‘fluid’’ – I can’t find the words, and so on. Where I
work, I feel I know so much – I know so much what’s
going on every day. But the other nurses don’t come and
ask me because they think it’s hard to get information
from me.’ (NS13:35)
Participants revealed that, in some instances, hospital
staff who spoke their first language at work experienced
animosity from their co-workers and in some
cases were directly told not to speak their first language
even when caring for patients who did not speak
English, because it made other co-workers ‘feel left
out’. In one case, a nurse overheard to speak her first
language at work was reported to management by other nurses, who subsequently reprimanded the nurse
and told her to ‘stop it’ (NS09:R1:28). In another case,
nursing staff were so intolerant and disrespectful of a
co-worker’s language difference that they repeatedly
criticised her given first name and asked her to change
it to a ‘shortened version’ (NS09:30).
Internalised language prejudice
Analysis of the data suggested that those who were the
targets of negative attitudes and behaviours of their
co-workers and managers sought to justify the prejudicial
attitudes and behaviours that had been directed
at them by normalising and internalising the behaviours.
As a nurse who had directly experienced such
negative behaviour explained:
‘I think it is quite normal. It is nothing to do with racism.
It is just that they don’t know you well and because you
look different and you are from a different place, so they
are a little bit scared or something.’ (NS09:R2:29)
In another incident, a nurse whose parents had been
Vietnamese refugees in the 1970s criticised a professional
development session on the use of health
interpreters, contending:
‘I don’t believe in all this stuff. This interpreter stuff is all
too expensive. If they [patients] want an interpreter, they
should bring their own.’ (ELO10:12)
Institutional language prejudice
Lack of infrastructure and resources
The lack of infrastructure and resources was most
evident in what participants described as the limited
availability of and access to accredited health interpreter
services. Several participants indicated that their
respective health services received only around 10%
of their actual funding requirements apropos the
provision of accredited health-interpreting services
per annum. Although most health services did their
best to meet patient demand for health-interpreting
services through their mainstream operations, they
were not always able to do so because of a lack of
infrastructure.And although the Telephone Interpreting
Services (TIS) is widely used in the healthcare sector,
some participants indicated that using TIS was not an
option for them because of a lack of basic telephone
equipment:
‘They don’t have a telephone that’s next to the bed. They
have the hands-free telephones but they disappear –
people take them, they can’t find the hands-free telephones
... So yeah, on the wards, it’s a real trouble, it’s a
challenge.’ (HI01:13)
Negative and discriminatory attitudes were also manifest
in system processes regulating the availability and flow of information to patients. For example, participants
revealed that in many instances, brochures and
posters containing information about a ward or a
health service tended to be available only in English.
Even when brochures and posters had been reproduced
in community languages, some patients still
could not access the information either because the
text was too small to read, or it was confusing in its
layout.
Sometimes patients could not read the material
because they were illiterate in their own language,
which had not been taken into account.
Lack of data
A key difficulty encountered by staff trying to develop
responsive communication services forNESB patients
was a lack of good data on the demand for and supply
of health-interpreting services. Participants pointed
out that the collection of data pertaining to the need
for and use of health interpreters was often hampered
because of various default options on the computer
software used by some services, and a reluctance by
staff responsible for completing the relevant documentation,
in either electronic or hard copy formats,
to ensure that data pertaining to the language backgrounds
of patients were recorded accurately, or even
at all:
‘I couldn’t work out why we have got so little number of
people using so many resources for language services.
Where are they coming from? I’ve got data saying:
English, English, English, only one out of every thirty
patients from diverse linguistic backgrounds. Iwas puzzled,
‘‘Why is my interpreter services budget going up?’’. And
we then found out that it was the computer defaulting to
‘‘English’’ [when the patient’s proper language wasn’t
added in] so that was why I couldn’t pick it up ... The
infrastructure was totally against me.’ (ELO07:11–12)
Contributors to negative attitudes
Underpinning the negative attitudes and related behaviours
discerned concerning people who spoke accented
English or who did not speak English proficiently were:
dislike of difference, fear of difference, intolerance of
difference, fear of competition for scarce (healthcare)
resources, repressed hostility toward difference, and
ignorance.
Dislike of difference
Some participants indicated that they did not like and
were deeply irritated by patients and families who
‘would not’ speak English even when it was known
that they did not and could not speak English, when
being cared for in a hospital context:
‘[What stands out for me] is them talking in their own
language while you’re with them. I don’t like that. I think it’s quite rude to do that when you’ve got somebody in
there that can’t speak that language. I think that’s not nice
... When they can’t speak both [English as well as their
own language], that really annoys me. I think it’s rude. I
don’t know, you go and say, ‘‘Hello’’ and talk to the
patient – talking in English – and the family would just
talk on in their own language. I just think it’s very rude, I
do ... It can make you feel uneasy in a room.’ (NS05:16–
18)
Fear of difference
Data suggested that in some contexts healthcare professionals
were afraid of the cultural and linguistic
differences exhibited by their patients:
‘What is it that frightens people? I don’t know. I think it
could be ‘‘difference’’, depending on the different cultures
that you are interacting with. Islam is a very good
example. Everyone is either hesitant about engaging
with Muslim people or they are afraid of them. They are
afraid of either doing something wrong to offend them –
that is definitely something – or, they are afraid – no, not
afraid, they just have this ‘‘hatred of things different’’.’
(ELO01:8)
Intolerance of difference
Many examples were given which suggested that
in addition to a fear of difference there was also a
profound intolerance of difference, expressed largely by
an attitude of ‘I don’t want to know about it’:
‘They do not want to know ... They often make that very
clear to me ... They don’t want to deal with it, they don’t
want to fund it, they don’t want to hear how hard it is.’
(ELO10:8)
Fear of competition with difference for
scarce resources
A majority of participants agreed that health services
have a responsibility to ensure that they provide
culturally and linguistically appropriate services to
patients of minority racial, ethnocultural and language
backgrounds. Nonetheless, even those with progressive
attitudes toward this stance included the rider ‘so
long as it was practical to do so’. One participant
contended that building language services into an
organisation’s infrastructure was not an option on
account of such services being cost prohibitive.Others
went even further, contending that, on the whole,
migrants were not entitled to any special consideration
on account of their cultural and language differences
because they had not earned it.
Repressed hostility toward difference
Some participants indicated that they were harbouring
repressed hostility toward ethnic patients and
families which sometimes burst through, especially when under pressure and stressed by their workplace
environments:
‘People are absolutely stressed to the max ... They are
really, really stressed out. They have to juggle so many
different priorities, and that is why (a) the priorities that
they deem as ‘‘lesser priorities’’ will be pushed down, or
will be less important. The other thing is that (b) they will
also have to lash out at something because they are so
incredibly frustrated.’ (ELO01:21–22)
Ignorance
Ignorance was also identified as a justification of
negative attitude and behaviours that were given
expression in healthcare domains. As one participant
reflected:
‘Maybe people just do not know how to deal with it, so
they just walk away and it’s not because they are mean
people or because they don’t care. It is just that, sometimes,
I suppose, they don’t know any better.’ (NS09:16–
17)
Discussion
Cultural racism is rarely expressed openly and can
come in many guises (Goldberg, 1993; Verkuyten,
1998; Ashcraft and Allen, 2003; Horne, 2005). It can
occur at several levels, each of which can have a
significant impact on health:
• institutionalised level characterised by a ‘differential
access to the goods, services, and opportunities of
society by race ... often evident as inaction in the
face of need’
• internalised level characterised by an ‘acceptance by
members of the stigmatised races of negative messages
about their own abilities and intrinsic worth’
• personally mediated level characterised by ‘prejudice
and discrimination, where prejudice is differential
assumptions about the abilities, motives, and
intents of others by race, and discrimination is
differential actions towards others by race’ (Jones
2001, p.300).
Language prejudice is a potent, but overlooked form
of cultural racism related to discrimination against
people who do not speak a country’s official language.
Language prejudice originates in anthropolitical linguistics
and is premised on the theory that languages,
dialects and accents are constructs that classify people,
as do race, in terms of skin colour, nationality,
ethnicity and kinship (Urciuoli, 1996; Lippi-Green,
1997). Like other observable differences, the language
differences of alien outsiders can be perceived by
homogenous insiders as being deeply threatening to
‘our way of life’.
When people are subject to language prejudice,
‘they are judged communicatively incompetent. Their
knowledge of language forms is judged inadequate
and contaminated: rules are said to be broken, boundaries
crossed, languages mixed, accents unintelligible’
(Urciuoli, 1996, p.2). Thus, in countries where English
signifies ‘the more valued language’ and other languages
the ‘less valued’, people whose first language is not
English are vulnerable to having their speech typified
by proficient English speakers in the moralistic terms,
for example, of being ‘ ‘‘broken’’ or ‘‘mixed’’ and their
accents as ‘‘heavy’’, all of which is contrasted with
‘‘good’’ English, as if good English were a clearly
defined object’ (Urciuoli, 1996, p.2). Also of concern
is the emerging evidence that, in countries where
English is the official or mainstream language, and if
there is a discordant relationship between the providers
and recipients of healthcare, the way in which
patients of minority racial and ethnocultural backgrounds
speak English even as a first language, or how
‘well’ they speak it, can have a negative influence on
whether they are treated fairly and respectfully by
attending professional caregivers in clinical domains
(Creese and Kambere, 2003; Johnson et al, 2004).
The sense that the language of foreign English
speakers is ‘different’, ‘bad’, or ‘wrong’ is further
reinforced ‘by reactions encountered in routine experiences’,
for example, by ‘information barriers: who
controls what one needs to know, what one must do or
say to be understood or believed’ (Urciuoli, 1996, p.3).
Language and communication in multicultural contexts
are thus highly politicised because, ultimately,
‘the interpretations that count depend on who has
power’ (Urciuoli, 1996, p.3).
Language prejudice, however, is not only manifest
in the spurious classification of peoples. It is also
fundamentally manifest in the often surreptitiously
unequal social structures and power relations that, in
turn, support the direct and indirect discrimination of
people who either do not speak English or speak
accented English as a second language (Lippi-Green,
1997).
The findings of the study reported in this article
have demonstrated that language prejudice and related
discrimination operated directly and indirectly
at three levels: individual, internalised and institutional.
When the findings were analysed using, as
an analytic frame, the theorised stances of language
prejudice and cultural racism advanced in the literature,
the following observations were made:
• language difference like skin colour was used as a
social marker to classify and categorise patients and
staff
• classifications were applied on the basis of whether
people:
– did not speak English
– spoke English, but not ‘proficiently’ or ‘fluidly’
– spoke English as a second language proficiently,
but with a ‘heavy’ accent
• people who did not speak English, or who spoke
English with only limited proficiency, orwho spoke
English proficiently as a second language but with
a ‘heavy accent’ were at risk of being evaluated
negatively as communicatively and rationally incompetent
and thus a threat to scarce healthcare
resources, the status quo. They were seen as ‘moral
failures’ who need to be ‘put in their place’
• negative evaluations of NESB people were used to
justify their exclusion from important healthcare
relationships and resources. For example, patients
were obstructed from getting access to qualified
health interpreters in a timely manner, or at all;
staff whose first language was not English were not
respected or accepted and included as knowledgeable
members of the healthcare team
• negative evaluations of NESB patients motivated
negative attitudes toward health-interpreting services
that, in turn, hampered the collection of
sound and reliable data to justify the appropriate
funding of responsive communication services for
NESB people.
Like racism based primarily on skin colour, the processes
that distinguish and motivate cultural racism are
extremely complex. There is, however, agreement among
racism theorists that social markers and dispositions
such as dislike of difference, fear of difference, intolerance
of difference, fear of competition with difference for
scarce resources, repressed hostility toward difference
and ignorance are foundational to racist thinking and
behaviour (Goldberg, 1993; Barker et al, 2001; Leets,
2001; Lo Bianco, 2001; Horne, 2005). Consistent with
the findings of studies in other fields outside of healthcare
(Urciuoli, 1996; Lippi-Green, 1997; Verkuyten,
1998; Barker et al, 2001), this study has implicated
dislike of difference, fear of difference, intolerance of
difference, fear of competition with difference for scarce
resources, repressed hostility toward difference, and
ignorance as key drivers motivating negative attitudes
and behaviours.
Communication has long been recognised as the
tool by which all interactions in the hospital environment
are governed (Raimbault et al, 1975) it ‘is not
only a means of communication but also a symbol of
common ground and a way of gaining deep access to
people’ (Clyne, 2007, p.6). In recent years, communication
failures have been implicated in 70–80% of
formally reported preventable adverse events in hospital
contexts and related poor patient safety outcomes
(Galvan et al, 2005; Johnstone and Kanitsaki,
2006; Divi et al, 2007). Language prejudice, by its very
nature, involves a profound failure in communication.
Moreover, given how vital communication is to the therapeutic relationship in healthcare, it can be seen
how language prejudice stands not only as a profound
failure in and a barrier tocommunication, but also as a
symbol of uncommon ground and a way of avoiding
the deep access to people that is otherwise critical to
the success of the therapeutic encounter. Thus, while
not able to demonstrate a conclusive link between the
practices of language prejudice discovered in the
context of this study and poor patient safety outcomes,
the examples captured nonetheless highlight
the risks that language prejudice and discrimination
obviously pose to the health, safety and quality care of
NESB patients.
Conclusions and recommendations
This study has underscored the need to recognise and
reconcile the manner in which racism has persisted
insidiously in healthcare domains, arguably because of
the illusion of its absence. Unless given practices are
shown to be expressive of racism, its harmful effects in
healthcare domains will remain hidden and will continue
operating in subtle and powerfulways. It will not
only go unnoticed and unchallenged, but will also be
continually reproduced (Apple, 1999).
The findings of this study suggest that healthcare
professionals, who are otherwise bound by anti-racist
ethical principles of conduct, sometimes engage in
racialised practices towards racial/ethnic minorities,
using terms of derogation and accusation that persistently
characterise ‘foreigners’ (alien outsiders) as ‘a
nuisance’, ‘a problem’, ‘getting out of control’, and a
threat to the common interests of ‘others’ (Verkuyten,
1998; Barker et al, 2001).
It is acknowledged that just as cultural racism and
its expression in the form of language prejudice will
probably never be eradicated in the broader community,
neither will they be eradicated in hospital
contexts. Nonetheless, cultural racism and language
prejudice can and should be managed to reduce, if
not prevent, their incidence and harmful impact in
healthcare domains. To this end, we conclude, first,
that the problemmust be recognised and its incidence
reported via formal incident-reporting processes.
Second, robust system processes must be put in
place that, although not always able to prevent language
prejudice in hospital contexts, may nonetheless make
it very difficult for the system and the people in it to
express their prejudices in cruel and harmful ways
(Horne, 2005). To this end, we contend that representative
health professional organisations as well as
governments have a responsibility to take into account
the mosaic of ‘minority interests that make up any
modern society’ and, rather than enforce uniformity,
accept the differing values, beliefs, opinions and ways
of life of racial and ethnic minority groups and enable
their harmonious expression (Horne, 2005, p.41).
Finally, we reiterate that this issue needs to be seen
and framed not just as a human rights and antidiscrimination
issue, but as a fundamental patient
safety and quality care issue for which everybody
shares responsibility (Johnstone and Kanitsaki, 2006).
Furthermore, professional educational initiatives must
include an emphasis not only on cultural competency
but also anti-racism.
Despite the obvious importance of the issue of
language prejudice to and in healthcare, it has not
been comprehensively investigated in the cultural
context of Australia. It is our hope that this article
will provide a catalyst for much needed debate and
further research on the subject, both nationally and
internationally.
References
- Allotey P, Manderson L and Reidpath D (2002) Addressing cultural diversity in Australian health services. Health Promotion Journal of Australia 13:29–33.
- Apple M (1999) The absent presence of race in educational reform [1]. Race, Ethnicity and Education 2:9–16.
- Ashcraft K and Allen B (2003) The racial foundation of organizational communication. Communication Theory 13:5–38.
- Australian Bureau of Statistics (2006) 2914.0.55.002–2006 Census of Population and Housing. Canberra: Australian Bureau of Statistics.
- Barker V, Giles H, Noels K et al (2001) The English-only movement: a communication analysis of changing perceptions of language vitality. Journal of Communication 51:3–37.
- Bhopal R (2006) Race and ethnicity: responsible use from epidemiological and public health perspectives. Journal of Law, Medicine and Ethics 34:500–7.
- Centre for Culture Ethnicity and Health (2003) Diversity in Hospitals: responding to the needs of patient and client groups from non-English speaking backgrounds. Policy and resource guide. Report prepared by the Acute Diversity Care Collaboration Program. Melbourne: Centre for Culture Ethnicity and Health.
- Clyne M (2007) Show-offs urgently required. The Australian, Higher Education Section, 14 November:26.
- Cooper-Patrick L, Gallo J, Gonzales J et al (1999) Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association 282:583– 9.
- Creese G and Kambere E (2003) ‘What colour is your English?’ Canadian Review of Sociology and Anthropology 40:565–73.
- Daniels N (2006) Equity and population health: toward a broader bioethics agenda. Hastings Center Report 36:2–35.
- Divi C, Koss R, Schmaltz S and Loeb J (2007) Language proficiency and adverse events in US hospitals: a pilot study. International Journal for Quality in Health Care 19:60–7.
- Flores G (2005) The impact of medical interpreter services on the quality of health care: a systematic review. Medical Care Research and Review 62:255–99.
- Galvan C, Bacha E, Mohr J and Barach P (2005) A human factors approach to understanding patient safety during pediatric cardiac surgery. Progress in Pediatric Cardiology 20:13–20.
- Goldberg D (1993) Racist Culture: philosophy and the politics of meaning. Oxford: Blackwell. Hamel J (1993) Case Study Methods. Newbury Park: Sage Publications.
- Horne D (2005) 10 Steps to a More Tolerant Australia. Melbourne: Penguin Books.
- Johnson R, Saha S, Arbelaez J, BeachMand Cooper L (2004) Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. Journal of General Internal Medicine 19:101–10.
- JohnstoneMandKanitsaki O (2006) Culture, language and patient safety: making the link. International Journal for Quality in Health Care 18:383–8.
- Johnstone M and Kanitsaki O (2007a) Health care provider and consumer understandings of cultural safety and cultural competency in health care: an Australian study. Journal of Cultural Diversity 14:96–104.
- JohnstoneMandKanitsakiO(2007b) An exploration of the notion and nature of ‘cultural safety’ and its applicability to the Australian health care context. Journal of Transcultural Nursing 18:247–56.
- JohnstoneMandKanitsaki O (2008) The problem of failing to provide culturally and linguistically appropriate healthcare. In: Barrowclough S and Gardner H (eds) Analysing Australian Health Policy: a problem orientated approach. Sydney: Churchill Livingstone/Elsevier Science, Australia, pp. 176–87.
- Jones C (2001) Invited commentary: ‘Race’, racism, and the practice of epidemiology. American Journal of Epidemiology 154:299–304.
- Larson A, Gillies M, Howard P, and Coffin J (2007) It’s enough to make you sick: the impact of racism on the health of Aboriginal Australians. Australian and New Zealand Journal of Public Health 31:322–9.
- Leets L (2001) Experiencing hate speech: perceptions and responses to anti-Semitism and antigay speech. Journal of Social Issues 58:341–61.
- Lippi-Green R (1997) English with an Accent: language, ideology and discrimination in the United States. London and New York: Routledge.
- Lo Bianco J (2001) From policy to anti-policy: how fear of language rights took policy-making out of community hands. In: Lo Bianco J and Wickert R (eds) Australian Policy Activism in Language and Literacy. Melbourne: Language Australia, pp. 13–44.
- Miles R (1989) Racism. London/New York: Routledge. Miles R and Brown M (2003) Racism (2e). London/New York: Routledge.
- Patton M (2002) Qualitative Research and Evaluation Methods (3e). Thousand Oaks: Sage Publications.
- Powers M and Faden R (2006) Social Justice: the moral foundations of public health and health policy. New York: Oxford University Press.
- Raimbault G, Cachin O, Limal J, Eliacheff C and Rappaport R (1975) Aspects of communication between patients and doctors: an analysis of the discourse in medical interviews. Pediatrics 55:401–5.
- Roberts D (2006) Legal constraints on the use of race in biomedical research: toward a social justice framework. Journal of Law, Medicine and Law 34:526–34.
- Sandelowski M (2000) Whatever happened to qualitative description. Research in Nursing and Health 23:334–40.
- Schnittker J and Liang K (2006) The promise and limits of racial/ethnic concordance in physician-patient interaction. Journal of Health, Politics, Policy and Law 31:811–37.
- Smedley B, Stith A and Nelson A (eds) (2003) Unequal Treatment: confronting racial and ethnic disparities in health care. Washington DC: The National Academics Press.
- Urciuoli B (1996) Exposing Prejudice: Puerto Rican experiences of language, race and class. Boulder, CO: Westview Press.
- VerkuytenM(1998) Personhood and accounting for racism in conversation. Journal of the Theory of Social Behaviour 28:147–67.
- Wolf S (2006) Introduction: debating the use of racial and ethnic categories in research. Journal of Law, Medicine and Ethics 34:483–6.