- (2011) Volume 12, Issue 3
Muhammad Wasif Saif, Marianne Brennan, Robin Penney, Susan Hotchkiss, Kristin Kaley
Columbia University College of Physicians and Surgeons, New York Presbyterian Hospital. New York, NY, USA
Received November 22nd, 2010 - Accepted February 15th, 2011
Pancreatic cancer is known to metastasize rapidly. Liver and peritoneum are the most common sites of metastases in pancreatic cancer, followed by lungs, bones and brain. Less common sites of metastases such as muscle, skin, heart, pleura, stomach, umbilicus, kidney, appendix, spermatic cord and prostate have also been reported in pancreatic cancer. Cutaneous metastasis mostly occurs around umbilicus. A site other than umbilicus is rarely reported. The authors report a case of multiple skin metastases in a patient with primary pancreatic cancer and review the literature.
Exanthema; gemcitabine-oxaliplatin regimen; Neoplasm Metastasis; Pancreas; Pancreatic Neoplasms; Skin
FOLFOX: folinic acid plus 5-fluorouracil plus oxaliplatin
Dear Sir:
Pancreatic cancer is known to metastasize rapidly [1]. Liver and peritoneum are the most common sites of metastases in pancreatic cancer, followed by lungs, bones and brain [2]. Less common sites of metastases such as muscle, skin, heart, pleura, stomach, umbilicus, kidney, appendix, spermatic cord and prostate have also been reported in pancreatic cancer [3, 4, 5, 6, 7, 8, 9, 10, 11, 12]. Cutaneous metastasis mostly occurs around umbilicus. A site other than umbilicus is rarely reported [13, 14]. We report here a case report of distant and multiple skin metastases in a patient with primary pancreatic cancer as a secondary site after developing bone metastases [15].
Our patient was a 46-year-old African American woman who was initially diagnosed with pancreatic adenocarcinoma in spring of 2007. A CT scan of chest/abdomen/pelvis revealed no evidence of metastatic disease, including bones. She underwent a distal pancreatectomy and splenectomy. The pathology showed pancreatic ductal adenocarcinoma with evidence of lymphovascular invasion, and with 3 of 18 lymph nodes involved. Her CA 19-9 was within normal limits (i.e., less than 37 U/L), and CEA was slightly elevated at 5.6 U/L (reference range: 0-4 U/L). Thus, the patient was staged as IIB. She was subsequently treated with six cycles of gemcitabine (Gemzar®, Eli Lilly, Indianapolis, IN, USA). The patient was in clinical remission until July of 2009 when she developed right clavicle pain. A repeat CT scan showed increased sclerosis of the medial right clavicular head with a moth-eaten appearance of the cortex and medullary space. The differential diagnosis included metastasis or chronic osteomyelitis. This was followed by a PET scan that showed increased tracer uptake in the medial right clavicle, consistent with either metastatic disease or osteomyelitis. A fine needle biopsy of the right clavicle was performed which confirmed metastatic pancreatic cancer. Upon further investigation, patient did notice pain in the area of the bone disease on the right neck area. The patient was started on zoledronic acid (Zometa®, Novartis, East Hanover, NJ, USA) and received a palliative course of radiation therapy to the affected clavicle (10 fractions). As she was near-completing her course of radiation therapy to the clavicle, she complained of new left hip pain. An MRI revealed radiographic evidence of focal disease in the left ischium, acetabulum, and femur. She was given an additional dose of 10 fractions of radiation therapy to the hip area.
Restaging CT showed interval progression of metastatic bony disease manifested by a new lesion in the left sacrum. Patient was started on modified FOLFOX6 consisting of 2 weekly cycles of oxaliplatin 85 mg/m2 i.v. over 2 h, together with leucovorin 400 mg/m2 over 2 h, 5-fluorouracil (5-FU) 400 mg/m2, and bolus, followed by a 46-h infusion of 5-FU at 2.4 g/m2. After a 12-week therapy with FOLFOX regimen, a repeat whole body bone scan showed multiple new foci of increased uptake: at the base of the skull involving the cervical spine, L2 and L3 vertebrae, approximate left 5th and 8th ribs/costovertebral regions of the thoracic spine, humeri (right more than left), proximal right radius/ulna, upper sacrum, multiple areas in the left bony pelvis, femora bilaterally, and left knee; previously noted increased uptake along the right clavicle appeared more intense compared to the baseline study. The FOLFOX therapy was discontinued.
Due to poor performance status, it was decided to hold further chemotherapy and continue best supportive therapy. The patient came for follow-up visit after 4 weeks and was found to have five areas of skin discoloration and thickening on the body as revealed in the Figures 1 and 2. The areas included right supraclavicular area, chest below right breast, right abdominal wall and a small area on the left abdominal wall. Since the right supraclavicular area was overlying the radiated area, we decided to perform the biopsy the other areas. A skin biopsy of the skin lesion on the abdomen was performed and the pathology confirmed metastasis from her primary pancreatic cancer. Immunohistochemical studies were performed. Tumor cells were positive for CK-7 and negative for CK-20, TTF-1, CDX2, estrogen receptor and progesterone receptor. This immunophenotype is not specific but was consistent with metastasis from the patient’s primary diagnosed pancreatic adenocarcinoma. Due to poor performance status, the decision was made to continue best supportive care and re-assess after another 3-4 weeks.
Cutaneous metastasis are rare [2, 3] and they are generally situated in the periumbilical area [16]. The mechanism of cutaneous metastasis in patients with pancreatic cancer is not well known. Multiple theories have been proposed (Table 1).
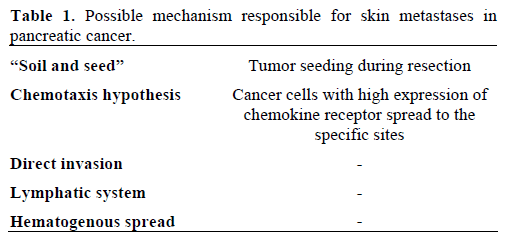
However, other investigators have proposed a “soil and seed” hypothesis. Tumor seeding during resection is a feared complication as recurrence within the peritoneal cavity commonly occurs after resection for curative intent [17].
In addition, pancreatic carcinoma is known to metastasize also via the lymphatic system through permeation, embolization, and retrograde spread due to lymphatic obstruction in the pancreas [18]. This hypothesis is further supported by Takeuchi et al. who found the umbilicus as the most frequent cutaneous metastatic site and suggested that spread through the blood or lymphatic systems may be responsible for the cutaneous sites [19].
Another investigator suggested that three different mechanisms, including direct invasion, local metastatic disease or distant metastasis can be responsible for cutaneous involvement in pancreatic cancer [20]. According to their experience, the last mechanism is most rare one, and when it occurs, skin metastases arise as multiple nodules grouped in a body area.
Review of most recent literature draws attention towards the chemotaxis hypothesis. Chemotaxis hypothesis narrates that cancer cell with high expression of chemokine receptor will spread to the specific sites where the ligand is highly secreted. Experiments by Wang and Ma suggest that the SDF- 1/CXCR4 receptor ligand system may have a possible role in the pancreatic cancer progression through tumor cell migration and angiogenesis [21].
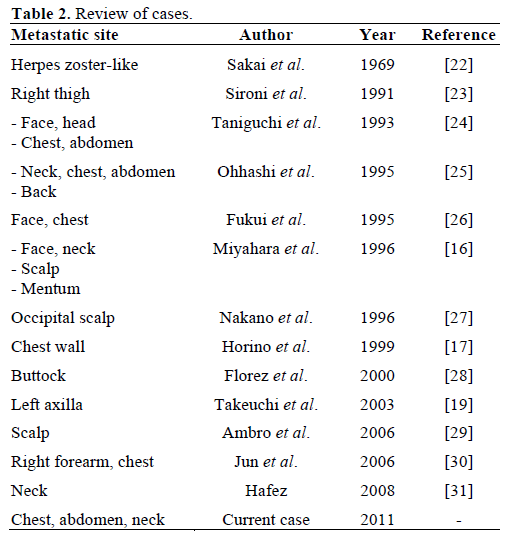
As described by other authors, majority of the cases reported had the cutaneous metastases present prior to the diagnosis of pancreatic cancer, while our case falls in to the category of those patients in whom the lesions were discovered by physical examination (Table 2).
In summary, cutaneous metastasis are rare but real sites of metastatic disease in patients with pancreatic cancer. Not only that their detection can lead to an underlying tumor but location can be indicated for palliative therapy. Topical 5-FU may be tested if similar cases continue to rise.
The authors have no potential conflicts of interest